What is Streptococcus pyogenes?
- Streptococcus pyogenes is a bacterium classified as a member of Group A Streptococcus (GAS). It is a Gram-positive organism that appears as spherical cells arranged in chains when viewed under a microscope. A defining feature of this bacterium is its beta-hemolytic nature, which means it has the ability to completely lyse red blood cells, forming clear zones around colonies on blood agar. This characteristic is often used for its identification in clinical laboratories.
- This microorganism is a significant human pathogen responsible for a range of diseases. It can cause pyogenic infections, which are characterized by the formation of pus, including bacterial pharyngitis (commonly known as strep throat) and cellulitis (a skin infection). In addition to these, S. pyogenes produces toxins that result in toxin-mediated illnesses such as scarlet fever and toxic shock syndrome, both of which can become severe without prompt treatment.
- Another major concern associated with S. pyogenes is its role in immunologic diseases. These occur when the body’s immune response to the infection inadvertently damages its own tissues. Examples include acute glomerulonephritis (AGN), which affects kidney function, and rheumatic fever, a condition that can lead to inflammation of the heart, joints, and other tissues.
- The ability of S. pyogenes to cause such a diverse range of infections is linked to its arsenal of virulence factors, including exotoxins and surface proteins, which help it evade the immune system and adhere to host tissues. Understanding the biology and pathogenic mechanisms of this bacterium is crucial for developing effective treatments and preventive measures.
Classification of Streptococcus
Streptococcus species are diverse bacteria that are classified based on their oxygen requirements, hemolytic activity, and antigenic structure. These classifications provide a framework for identifying different types of streptococci and understanding their roles in human health and disease.
Classification by Oxygen Requirement
- Aerobes and Facultative Anaerobes: These streptococci can grow in the presence of oxygen and include many medically relevant species.
- Obligate Anaerobes: Known as peptostreptococci, these species grow only in oxygen-free environments.
Classification Based on Hemolysis on Blood Agar
This system focuses on how streptococci affect red blood cells when grown on blood agar.
- Alpha-Hemolytic Streptococci:
- Produce a greenish zone of hemolysis due to partial lysis of red blood cells.
- This discoloration results from a reduced hemoglobin byproduct.
- Includes viridans streptococci and Streptococcus pneumoniae.
- These bacteria are common commensals in the upper respiratory tract but can cause opportunistic infections.
- Beta-Hemolytic Streptococci:
- Form clear, colorless zones of complete hemolysis around their colonies.
- Hemolysis is mediated by streptolysin O (oxygen-labile) and streptolysin S (oxygen-stable).
- These are the most pathogenic, with Streptococcus pyogenes being the most clinically important species.
- Gamma-Hemolytic Streptococci:
- Do not cause hemolysis or discoloration on blood agar.
- Typically nonpathogenic and found as commensals, such as Enterococcus faecalis (formerly Streptococcus faecalis).
Classification Based on Antigenic Structure
The Lancefield classification uses serological methods to group beta-hemolytic streptococci by detecting the group-specific carbohydrate antigen (C antigen) on their cell walls.
- Groups A to W:
- Streptococci are divided into 21 groups, skipping I and J.
- Group A (S. pyogenes) is the primary cause of human infections, while Group B (S. agalactiae) is another medically important group.
- Griffith Typing:
- Focuses on M, T, and R protein antigens on the surface of S. pyogenes.
- Divides S. pyogenes into 80 serotypes based on the M protein, a critical virulence factor.
- Useful for tracking epidemiological patterns in streptococcal diseases.
This structured classification system enables precise identification and study of Streptococcus species, aiding in diagnosis and treatment strategies.
Geographical Distribution and Habitat of Streptococcus pyogenes
Streptococcus pyogenes is found all over the globe, affecting various regions with differing patterns of prevalence and disease manifestation. The bacterium thrives in specific habitats within the human body, which makes it a persistent part of normal flora but also a potential pathogen under certain conditions.
Geographical Distribution
- Global Prevalence: S. pyogenes infections are found worldwide, making them a significant concern for public health across continents.
- Tropical Regions: In tropical areas, streptococcal pyoderma (a skin infection) is more common, with a higher prevalence. These infections show no seasonal variation, meaning they can occur year-round in these regions.
- Temperate Climates: In temperate zones, streptococcal pyoderma tends to be more frequent in the winter months, likely due to colder weather, which may encourage more indoor gatherings and the spread of infection.
- Rheumatic Fever: This condition is most common in children aged 5–15 years, the group most susceptible to S. pyogenes infections.
- The attack rate for rheumatic fever following an untreated or poorly treated upper respiratory tract infection is around 3%.
Habitat
- Normal Flora: S. pyogenes resides as part of the normal flora in several areas of the human body, including:
- Oral cavity
- Nasopharynx
- Skin
- Fingernails
- Perianal region
- Intestine
- Upper respiratory tract
- While it typically exists in these areas without causing harm, it can become pathogenic under certain conditions, leading to infections such as pharyngitis, skin infections, and more serious conditions like necrotizing fasciitis.
Morphology of Streptococcus pyogenes
Streptococcus pyogenes is a Gram-positive bacterium with distinctive structural characteristics that make it a vital subject in microbiological studies. Below is an organized breakdown of its morphology:
- Size and Arrangement:
- These bacteria are Gram-positive cocci, measuring approximately 0.6–1.0 μm in diameter.
- Cells typically form long chains due to their division in a single plane.
- In clinical samples or liquid cultures, they may also appear as pairs or chains of various lengths.
- Non-Motile and Non-Sporing Nature:
- The species lacks motility, relying on other mechanisms for survival and spread.
- It does not form spores, maintaining a simple cell structure.
- Capsule Formation:
- Certain strains can produce a capsule, particularly during the initial 2–4 hours of growth.
- The capsule is composed of hyaluronic acid, which includes repeating units of glucuronic acid and N-acetylglucosamine.
- This composition mimics host connective tissue, rendering the capsule nonantigenic and aiding in immune evasion.
- Encapsulated strains create mucoid colonies when cultured on blood agar.
Culture and Biochemical Reactions of Streptococcus pyogenes
Streptococcus pyogenes demonstrates specific growth patterns and biochemical behaviors that are vital for its identification and study. Here’s a detailed breakdown:
Culture
- Growth Conditions:
- Aerobic and facultatively anaerobic.
- Optimal growth occurs at 37°C with a pH range of 7.2–7.4.
- Enriched media, particularly blood agar, is essential for cultivating the organism.
- Blood Agar Characteristics:
- Colonies are small, white to gray, and measure 0.5–1 mm in diameter.
- Produces clear beta-hemolysis zones around colonies.
- Growth and hemolysis are enhanced in the presence of 10% CO₂.
- Virulent strains form matt colonies, while avirulent strains appear glossy.
- Strains with high hyaluronic acid production show a mucoid appearance.
- Selective Media:
- Crystal violet blood agar is selective due to its ability to inhibit other Gram-positive cocci.
- The addition of 0.0001% crystal violet ensures preferential growth of S. pyogenes.
- PNF medium (horse blood agar with polymyxin B sulfate, neomycin sulfate, and fusidic acid) is also effective for isolating the bacteria.
- Transport Medium:
- Pikes transport medium, containing crystal violet and sodium azide, is commonly used for throat swabs.
- These additives maintain bacterial viability while inhibiting contaminants.
- Liquid Media:
- In serum or glucose broth, the bacteria grow as granular turbidity with a powdery deposit at the bottom.
Biochemical Reactions
- Catalase Test:
- S. pyogenes is catalase-negative, a key distinction from staphylococci.
- Sugar Fermentation:
- Ferments many sugars, producing acid without gas.
- Ribose is not fermented, though these patterns are not heavily relied upon for diagnosis.
- Bile Solubility:
- The organism is not soluble in bile, aiding differentiation from other bacteria.
- PYR Hydrolysis:
- Hydrolyzes pyrrolidonyl naphthylamide (PYR), an important diagnostic reaction.
Cell Wall Components and Antigenic Structure of Streptococcus pyogenes
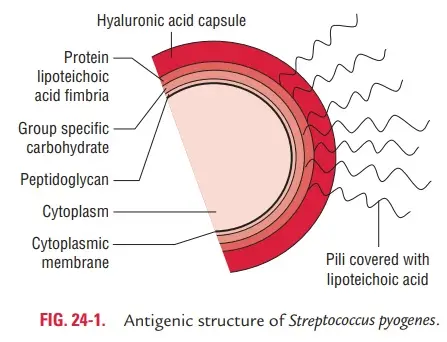
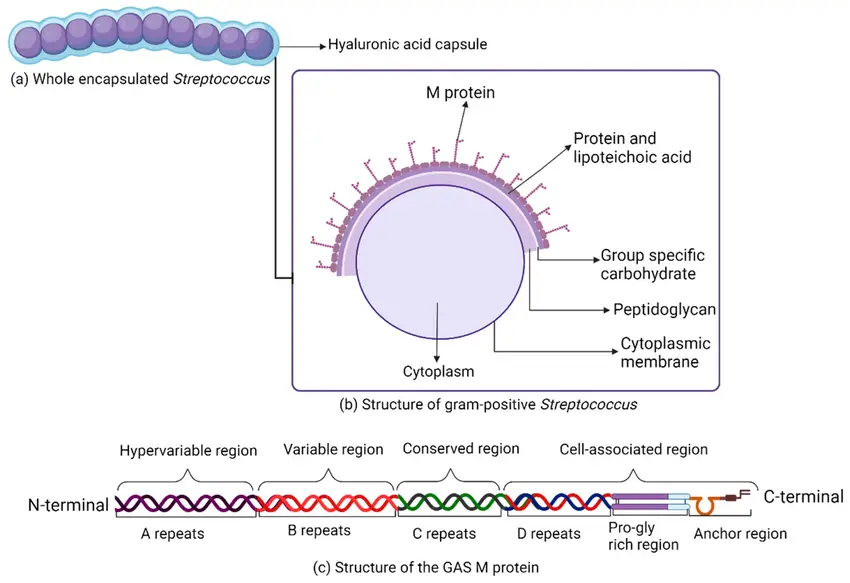
The cell wall of Streptococcus pyogenes is made up of various components that play essential roles in its structure, virulence, and identification. Here’s an in-depth breakdown of these elements:
Group-Specific Carbohydrate
- The cell wall contains a group-specific polysaccharide, which forms about 10% of the cell’s dry weight.
- This carbohydrate is composed of N-acetylglucosamine and rhamnose, and is nontoxic in rabbits, acting as a hapten.
- Based on the group-specific carbohydrate (C) antigen, S. pyogenes is divided into 21 groups (A–W, excluding I and J), referred to as Lancefield groups.
- The C antigen can be extracted using various methods:
- Acid extraction with hydrochloric acid (Lancefield method)
- Formamide extraction at 150°C (Fuller’s method)
- Autoclaving (Rantz and Randall’s method)
- Enzyme extraction (Maxted’s method)
- After extraction, the carbohydrate is treated with type-specific antiserum for precipitation reactions or immunofluorescence to group S. pyogenes isolates.
Type-Specific Proteins
Three major proteins in the cell wall play significant roles in S. pyogenes‘ serologic typing and virulence:
- M Protein:
- M protein is the primary virulence factor of S. pyogenes.
- It is acid- and heat-stable, but trypsin-sensitive.
- M protein helps the bacteria evade phagocytosis and aids in attachment to epithelial cells.
- The protein has a complex alpha-helix structure with two parts:
- The carboxyl terminus binds to the cytoplasmic membrane and is highly conserved.
- The amino terminus extends through the cell wall to the surface and is highly variable.
- The variability in the amino terminus creates antigenic diversity, leading to over 80 serotypes (1–60).
- Class I M proteins: Antibodies formed against the conserved region are linked to rheumatic fever pathogenesis.
- Class II M proteins: These do not trigger the production of antibodies.
- T Protein:
- T proteins are trypsin-resistant and heat-labile.
- Useful for epidemiological surveillance, T typing helps track strains involved in infections but is less important for understanding virulence.
- R Protein:
- R proteins are pepsin-sensitive but trypsin-resistant.
- These proteins don’t have a role in strain typing but may play other minor functions.
Other Cell Surface Components
- Peptidoglycan:
- Peptidoglycan provides rigidity to the cell wall.
- It also contributes to the fever response and can cause dermal and cardiac necrosis in animals.
- Peptidoglycan plays a role in the lysis of erythrocytes.
- Lipoteichoic Acid:
- This component contributes to the adhesion of S. pyogenes to host tissues.
- F Proteins:
- F proteins are involved in attachment to host cells, helping the bacteria establish infection.
Virulence Factors of Streptococcus pyogenes
Streptococcus pyogenes employs a variety of virulence factors that enable it to infect the host, evade the immune system, and cause disease. These factors include cell wall-associated proteins and polymers, enzymes, and toxins.
Cell Wall-Associated Proteins and Polymers
- Capsule:
- The capsule surrounding S. pyogenes is nonantigenic and only weakly antiphagocytic.
- It forms a physical barrier, preventing complement proteins from binding to the bacteria and stopping phagocytosis.
- Strains with a capsule rich in M proteins are more pathogenic.
- Teichoic Acid:
- Teichoic acid plays a role in binding the bacteria to epithelial cells.
- It helps S. pyogenes adhere to surfaces in the body.
- M Protein:
- M protein is one of the most crucial virulence factors.
- It acts as both an adhesin and antiphagocytic agent, helping the bacteria stick to cells while also inhibiting phagocytosis.
- M protein inactivates C3b, a critical complement factor, which would otherwise tag the bacteria for destruction.
- Strains abundant in M protein are resistant to phagocytosis and intracellular killing by polymorphonuclear leukocytes (PMNs).
- M protein interferes with opsonization via the alternative complement pathway and helps in epithelial attachment.
- F Protein:
- F proteins mediate binding to fibronectin, which is present on the host cell surface.
- This is another way S. pyogenes facilitates attachment to host tissues.
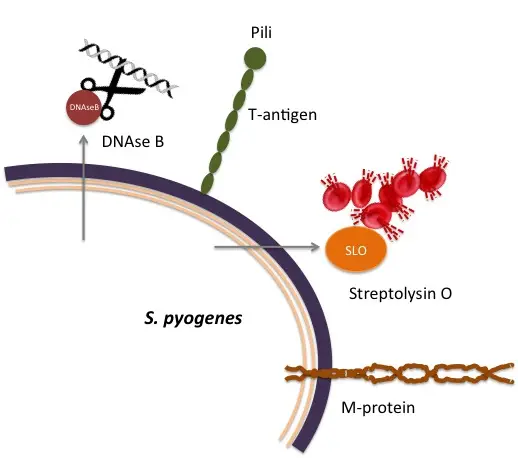
Enzymes
- Streptokinase:
- This enzyme activates plasminogen, converting it into plasmin.
- Plasmin breaks down the fibrin barrier around an infected site, helping the bacteria spread.
- Streptokinase also has therapeutic use in treating myocardial infarction, where it dissolves blood clots.
- Antibodies to streptokinase (types A and B) appear during infection and can be used diagnostically.
- Deoxyribonucleases:
- S. pyogenes produces four types of deoxyribonucleases (A, B, C, and D).
- These enzymes depolymerize free DNA present in pus, reducing its viscosity and aiding infection spread.
- Antibodies against deoxyribonuclease B are diagnostic of infections, particularly skin infections.
- Hyaluronidase:
- This enzyme breaks down hyaluronic acid, a component of the extracellular matrix in host connective tissue.
- It allows S. pyogenes to spread through tissues.
- Like other enzymes, hyaluronidase is antigenic and contributes to tissue damage.
- Serum Opacity Factor (SOP):
- Produced by certain M types, this lipoproteinase produces opacity when applied to agar gel containing swine or horse serum.
- SOP is antigenic and helps in bacterial identification.
- Other Enzymes:
- S. pyogenes also produces neuraminidase, amylase, esterase, lipase, and beta-glucuronidase, each playing minor roles in pathogenesis.
Toxins
- Streptococcal Pyrogenic Exotoxins (SPEs):
- These erythrogenic toxins (A, B, and C) are superantigens that trigger excessive immune responses.
- They are responsible for diseases like scarlet fever and streptococcal toxic shock syndrome.
- SPEs are antigenic, and their production is regulated by temperate phages in the bacterial genome.
- Hemolysins:
- S. pyogenes produces two types of hemolysins:
- Streptolysin O (SLO): Oxygen-labile and heat-labile, SLO causes beta-hemolysis when grown under the surface of blood agar.
- It is antigenic, and antibodies to SLO (ASLO) are useful in diagnosing recent group A streptococcal infections.
- SLO cross-reacts with similar toxins from other bacteria.
- Streptolysin S (SLS): Oxygen-stable and serum-soluble, SLS is a small protein that causes hemolysis on the surface of blood agar.
- It inhibits chemotaxis, is antiphagocytic, and does not trigger an antibody response.
- Streptolysin O (SLO): Oxygen-labile and heat-labile, SLO causes beta-hemolysis when grown under the surface of blood agar.
- S. pyogenes produces two types of hemolysins:
- Pyrogenic Exotoxins A and B:
- Pyrogenic exotoxin A is similar to staphylococcal toxic shock syndrome toxin (TSST) and acts by releasing cytokines from helper T cells and macrophages.
- Pyrogenic exotoxin B is a protease that rapidly destroys tissues and is produced in large amounts by S. pyogenes.
Pathogenesis of Streptococcal Infections
Streptococcus pyogenes causes a range of infections, from mild throat infections to severe diseases. The pathogenesis of these infections relies on a combination of mechanisms that help the bacteria invade, evade the immune system, and spread within the body.
- Adherence to Host Cells
- The first step in the infection process is the bacteria’s ability to stick to the host’s surface.
- S. pyogenes uses pili, lipoteichoic acid, M proteins, and F proteins to attach to epithelial cells in the pharynx and other tissues.
- Initially, lipoteichoic acid interacts weakly with host cell fibronectin, but the attachment strengthens through M protein and F protein.
- These interactions ensure a firm adhesion to the host, setting the stage for invasion.
- Invasion into Host Cells
- Once adhered, S. pyogenes invades host cells, particularly in the pharynx during conditions like streptococcal pharyngitis.
- This invasion is facilitated by M protein, F protein, and other bacterial factors, which help the bacteria penetrate deeper into tissues.
- The hyaluronic acid capsule also plays a crucial role in preventing immune clearance by blocking phagocytosis.
- The M protein’s ability to inactivate C3b, a critical component of the immune system’s ability to recognize and destroy bacteria, makes the pathogen more resistant to immune attack.
- By binding to fibrinogen and disrupting complement activation, the M protein limits the production of C3b, further aiding in evading immune responses.
- Additionally, C5a peptidase inactivates C5a, a complement component responsible for attracting immune cells like neutrophils, thus reducing the recruitment of immune cells to the infection site.
- Production of Toxins and Enzymes
- Once inside the host, S. pyogenes produces a variety of toxins and enzymes that promote its survival and further damage the host.
- These toxins can destroy host tissue, provoke excessive immune responses, and aid in bacterial spread.
- The presence of these virulence factors is a major contributor to the severity of streptococcal diseases.
Clinical Syndromes of Streptococcus pyogenes
Streptococcus pyogenes can cause a wide array of clinical conditions. These can be broadly categorized into three groups: suppurative streptococcal diseases, toxin-mediated diseases, and nonsuppurative streptococcal diseases. Each group presents distinct clinical manifestations, and understanding these is crucial for diagnosis and treatment.
Suppurative Streptococcal Diseases
- Respiratory Infections
- Pharyngitis is the most common infection caused by S. pyogenes, often referred to as a sore throat.
- Symptoms include inflammation of the pharyngeal mucosa, exudate formation, swollen cervical lymph nodes, fever, and leukocytosis.
- This infection is most common in children and spreads through respiratory droplets.
- The incubation period ranges from 1 to 4 days, with most cases resolving within 3 to 5 days without complications.
- Skin and Soft Tissue Infections
- Pyoderma (Impetigo) is a superficial skin infection, primarily affecting exposed areas such as the face, arms, and legs.
- It spreads through direct contact or fomites, commonly affecting young children. Certain serotypes of S. pyogenes, such as types 49 and 53–55, are involved.
- Erysipelas is an acute skin infection that affects the superficial lymphatics, presenting with red, swollen skin with well-defined borders.
- This condition often affects the face and legs, occurring more commonly in young children or older adults.
- Cellulitis is a deeper skin and subcutaneous tissue infection that causes swelling, tenderness, fever, and systemic symptoms like headache and malaise.
- The infection may spread without an apparent primary infection site.
- Necrotizing Fasciitis is a rapidly progressing infection of the fascia, caused by certain strains of S. pyogenes, particularly M types 1 and 3.
- It results in extensive tissue destruction and is associated with toxic shock-like syndrome, leading to multiorgan failure.
Toxin-Mediated Diseases
- Scarlet Fever occurs as a complication of streptococcal pharyngitis caused by specific strains of S. pyogenes that produce pyrogenic exotoxins.
- Symptoms include fever, pharyngitis, and a characteristic rash followed by desquamation.
- Scarlet fever has become rarer with the use of antibiotics.
- Streptococcal Toxic Shock Syndrome (STSS) is caused by certain S. pyogenes strains, particularly M serotypes 1 and 3.
- It initially presents as localized pain at the infection site, along with nonspecific symptoms like fever, nausea, vomiting, and diarrhea.
- The condition progresses rapidly to multiorgan failure and shock.
- It is most common in patients with pre-existing conditions like HIV, varicella, diabetes, or heart disease.
- Other Pyogenic Infections
- Lymphangitis and puerperal sepsis are additional conditions caused by S. pyogenes.
- Infections can also occur in internal organs like the liver, lungs, kidneys, and brain, often leading to abscesses.
- Bacteremia can result from invasive infections and may lead to systemic spread.
Nonsuppurative Streptococcal Diseases
- Acute Glomerulonephritis (AGN) is a nonsuppurative complication that follows S. pyogenes infections, typically 2–3 weeks after pharyngitis or skin infections.
- Certain M protein types, such as types 1, 12, and 49, are commonly implicated.
- The disease results from the deposition of antigen–antibody complexes on the glomerular basement membrane, causing inflammation and damage.
- Symptoms include hypertension, edema, hematuria, and proteinuria. The prognosis is generally good, with most young patients recovering fully.
- Rheumatic Fever is an immunologically mediated disease that develops 2–4 weeks after a streptococcal infection.
- It affects multiple organs, including the heart, joints, skin, and brain.
- Symptoms include fever, migrating polyarthritis, carditis, and subcutaneous nodules. Damage to the heart valves may occur, leading to long-term complications.
Reservoir, Source, and Transmission of Infection
Streptococcus pyogenes primarily thrives in infected humans, making them the main reservoir of the bacteria. The transmission routes are varied, but most of the infection spread occurs through direct contact and respiratory droplets. The bacterium can also survive in the environment, adding to its ability to spread in different settings.
Reservoir and Source of Infection
- Infected Humans: The primary reservoir for S. pyogenes is humans who are actively infected. These individuals harbor the bacterium and can spread it to others.
- Respiratory Droplets: One of the most common sources of S. pyogenes is respiratory and salivary secretions. These are expelled when an infected person coughs or sneezes, releasing the bacteria into the air.
- Contaminated Fomites: Infected surfaces, or fomites, can also harbor the bacteria. These objects can transfer the infection when touched by an individual who then touches their mouth, nose, or eyes.
- Carrier State: A significant proportion of individuals—about 20–40%—can act as carriers of S. pyogenes. These individuals often have chronic, asymptomatic colonization in their pharynx or nasopharynx. While they may carry the bacteria, they usually do not spread disease, as the bacteria they harbor are often avirulent.
Transmission Routes
- Person-to-Person Spread: The primary mode of transmission for S. pyogenes is person-to-person. It is spread through respiratory droplets when an infected individual coughs or sneezes, passing the bacteria into the air.
- Direct Contact: The infection can also spread through direct contact with an infected person, especially if there are breaks in the skin. This can happen through touch or interaction with contaminated objects or surfaces.
- Arthropod Vectors: Though less common, arthropod vectors, such as insects, can sometimes contribute to the spread of the bacteria by transferring it from one individual to another.
- Children and Infected Secretions: Children, particularly those with untreated infections, are key transmitters. They spread the infection through salivary droplets and nasal discharge, which makes them significant vectors in household and school environments.
Environmental Factors
- Overcrowding: Crowded conditions, such as those found in homes with limited space or in classrooms, increase the likelihood of transmission. Children living in such environments are at higher risk for both impetigo and pharyngitis due to the close contact and the spread of respiratory droplets.
- Poor Hygiene: The risk of infection is higher in areas with poor hygiene practices. Lack of proper handwashing and sanitation further aids in the spread of S. pyogenes.
Other Outbreaks
- Foodborne and Waterborne Outbreaks: Occasionally, there are reports of foodborne and waterborne outbreaks. Though these are not as common as respiratory or direct contact transmission, they still represent a potential route for infection.
Research and Epidemiology
- Bacteriocin and Phage Typing: Research into the spread and types of S. pyogenes infections often involves techniques like bacteriocin typing and phage typing. These methods help trace specific strains of the bacteria and study patterns of infection in populations.
Laboratory Diagnosis of Infection
Diagnosing a Streptococcus pyogenes infection requires multiple approaches, depending on the site and type of infection. Specimen collection, microscopy, culture, and a range of specific tests help confirm the presence of the bacterium.
Specimen Collection
The type of specimen collected depends on the manifestation of the infection. Common specimens include:
- Throat Swabs: For diagnosing pharyngitis or tonsillitis.
- Nasal Swabs: Often collected in cases of nasal or respiratory tract infections.
- Pus or Pus Swabs: For infections involving the skin or soft tissues.
- Vaginal Swabs: In cases of puerperal sepsis.
- Blood and Cerebrospinal Fluid: For suspected systemic infections.
- Joint Aspirates: In cases of septic arthritis.
- Skin Biopsy or Aspirates: Used in suspected skin infections like cellulitis or necrotizing fasciitis.
- Bronchoalveolar Lavage Fluid: For respiratory tract infections.
- Abscess Fluid: Collected from abscesses to identify the infection site.
In cases of suspected necrotizing fasciitis, a frozen section biopsy from the operating room may be necessary.
Microscopy
- Gram Staining: A rapid diagnostic method, particularly useful for skin and soft tissue infections. Pus or exudate from infected areas is stained with Gram stain. The presence of Gram-positive cocci in chains or pairs, along with leukocytes, suggests the presence of S. pyogenes.
- Limitations: For respiratory infections like pharyngitis, Gram staining is not reliable. This is because streptococci are part of the normal flora in the oropharynx, making it hard to differentiate from other harmless bacteria.
Culture
- Throat Swab Culture: The most specific diagnostic method for streptococcal pharyngitis. The swab should be collected from the tonsils and posterior pharynx, as these areas contain a higher number of bacteria. Once collected, the sample should be plated on 5% sheep blood agar and incubated at 37°C with 5-10% CO2 for 2-3 days.
- Beta-Hemolysis: On blood agar, S. pyogenes produces a clear zone of beta-hemolysis around small colonies, which is characteristic of the bacterium.
Identification of Bacteria
Several tests are employed to identify S. pyogenes:
- Bacitracin Sensitivity Test: S. pyogenes is highly sensitive to bacitracin, a key differentiator from other streptococcal groups. A 0.04 U bacitracin disc is placed on an inoculated blood agar plate. A zone of inhibition confirms the presence of S. pyogenes. This test is simple and highly effective in identifying group A streptococci.
- L-Pyrrolidonyl-beta-naphthylamide (PYR) Test: This test detects L-pyrrolidonyl-beta-naphthylamidase (PYRase), an enzyme produced by S. pyogenes. When a substrate disc is applied to an inoculated agar plate, it reacts with p-dimethylamino cinnamaldehyde to produce a red color, confirming the presence of S. pyogenes.
- Direct Antigen Detection Test: This method involves detecting the group-specific carbohydrate antigen A using a direct fluorescent antibody test on throat swabs. The results are obtained in 4 hours, offering a rapid and specific diagnosis, although it is less sensitive than culture.
Serodiagnosis
Serological tests are used to identify infections that have caused sequelae, such as acute glomerulonephritis (AGN) or rheumatic fever. These tests detect elevated antibody levels against several streptococcal antigens:
- Anti-Streptolysin O (ASO) Antibodies: The most commonly used for diagnosing rheumatic fever and AGN. These antibodies appear 3-4 weeks after infection. An ASO titer greater than 200 is considered indicative of streptococcal infection. Higher titers are found in acute rheumatic fever, while lower titers are seen in conditions like glomerulonephritis.
- Anti-DNase B, Anti-Hyaluronidase, Anti-Streptokinase: These antibodies are also measured and can aid in confirming streptococcal pharyngitis or pyoderma. Elevated levels of these antibodies suggest recent S. pyogenes infection.
Treatment of Streptococcus pyogenes Infection
The treatment for Streptococcus pyogenes infections primarily involves antibiotics, with penicillin being the most effective and preferred option. The choice of antibiotic can vary based on the clinical presentation and patient factors such as allergies or complications.
First-Line Treatment
- Penicillin:
- Penicillin remains the drug of choice for treating S. pyogenes infections.
- It is highly effective and no penicillin-resistant strains have been documented.
- For uncomplicated infections like pharyngitis, 250–500 mg of oral penicillin is typically administered twice daily for at least 10 days.
- The most common reason for treatment failure with penicillin is noncompliance, where patients often stop the medication too early, typically after 3-4 days when they feel better.
- Failure to Respond to Penicillin:
- In many cases, treatment failure occurs because the prescribed 10-day course is not completed.
- A common issue is that patients, particularly children, discontinue the medication too soon, often after the initial few days of feeling better.
- Another potential cause, though not fully proven, could be the presence of beta-lactamase-producing organisms in the mouth, which could inactivate the penicillin.
Alternative Treatments
- Erythromycin and Clindamycin:
- For individuals who are allergic to penicillin, erythromycin and clindamycin are the alternatives.
- However, erythromycin-resistant strains of S. pyogenes have been reported, making it less reliable in certain cases.
- Avoidance of Certain Antibiotics:
- Sulfonamides and tetracycline are not recommended for treating streptococcal infections due to poor efficacy against the bacteria.
Complicated or Invasive Infections
- For more complicated or invasive forms of infection, penicillin might still be used, but it could be combined with other treatments based on the severity and location of the infection.
Prevention and Control of Streptococcus pyogenes Infection
Preventing and controlling Streptococcus pyogenes infections is essential, especially for individuals at risk of complications like acute glomerulonephritis (AGN) or rheumatic fever. Prophylactic measures, including chemoprophylaxis, are key to minimizing the recurrence of infections and protecting against severe outcomes.
Chemoprophylaxis
- Penicillin Prophylaxis:
- Long-term penicillin use is recommended for individuals with a history of acute rheumatic fever to prevent reinfection.
- Rheumatic heart disease patients may require lifelong chemoprophylaxis to avoid streptococcal infections that can worsen heart damage.
- Penicillin is the antibiotic of choice for chemoprophylaxis, preventing further complications related to streptococcal infections.
- Household Contacts:
- The necessity of chemoprophylaxis for household contacts of individuals with acute streptococcal infections or nonsuppurative complications (like AGN or rheumatic fever) is still uncertain and under investigation.
General Prevention Measures
- Preventing the spread of S. pyogenes in communal settings, especially schools or households, involves good hygiene practices and avoiding close contact with infected individuals until they’ve completed appropriate antibiotic therapy.
- Kanwal S, Vaitla P. Streptococcus Pyogenes. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554528/
- https://www.sciencedirect.com/topics/medicine-and-dentistry/streptococcus-pyogenes
- https://emedicine.medscape.com/article/228936-overview
- https://www.nature.com/articles/s41579-023-00865-7
- https://www.ncbi.nlm.nih.gov/books/NBK343617/
- https://www.who.int/teams/immunization-vaccines-and-biologicals/diseases/streptococcus-pyrogenes
- https://www.cdc.gov/group-a-strep/hcp/clinical-guidance/index.html
- https://www.canada.ca/en/public-health/services/diseases/group-a-streptococcal-diseases.html
- https://en.wikipedia.org/wiki/Streptococcus_pyogenes
- https://www.brainkart.com/article/Cell-Wall-Components-and-Antigenic-Structure—Streptococcus-pyogenes_18018/