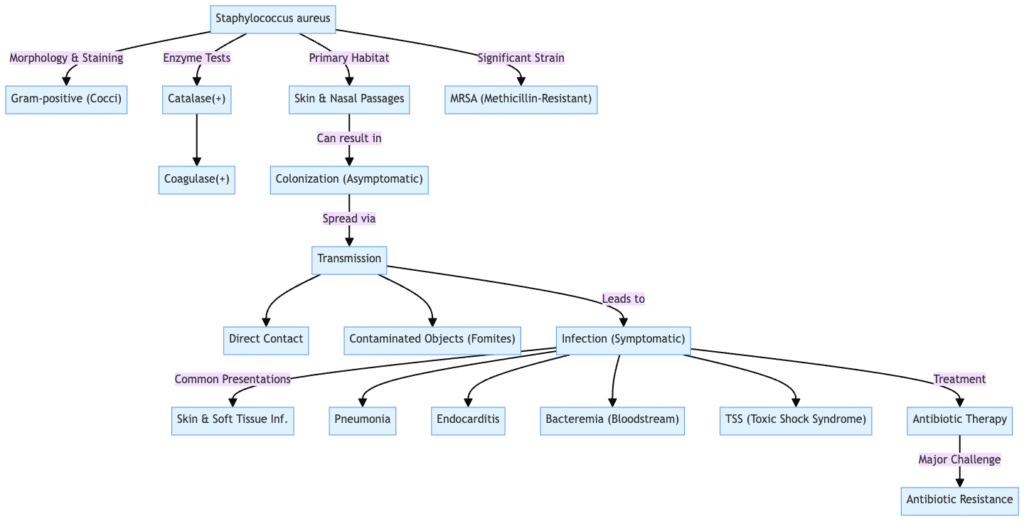
Staphylococcus aureus is a Gram‑positive, facultative anaerobic bacterium, usually found in clusters that resemble grapes and typically 0.5–1µm in diameter.
Harbor, as a commensal organism, in the human nasal passages, skin, and mucous membranes of 20–30% of people without causing disease
It is an opportunistic pathogen that can cause a wide range of infections—from simple skin lesions, such as pimples or boils, to serious diseases, such as pneumonia, osteomyelitis, endocarditis, sepsis and toxic shock syndrome
Expresses several virulence factors such as tissue adherence surface proteins, coagulase (to precipitate plasma), various toxins ( α-toxins, enterotoxins TSST-1), and enzymes like hyaluronidase and DNase
Famous for being antibiotic resistant, in particular methicillin‑resistant S aureus (MRSA) which was identified in the 1960s, that doesn’t appear to be susceptible to any of the antibiotics that are typically used in such an environment.
And a brief history:
- First discovered in 1880 by Sir Alexander Ogston in Aberdeen, Scotland; isolated from pus from surgical abscessesa; so called for its clustered (“staphylo–”) and golden (“aureus”) appearance.
- Rosenbach, in 1884, isolated S aureus from closely related species
- penicillins developed for treatment in 1940s, emergence of widespread penicillin resistance by late 1940s, MRSA by 1960
- S aureus is therefore a predominant commensal and a versatile pathogen of notable historical and medical importance.
| Domain: | Bacteria |
| Phylum: | Bacillota |
| Class: | Bacilli |
| Order: | Bacillales |
| Family: | Staphylococcaceae |
| Genus: | Staphylococcus |
| Species: | S. aureus |
What is Staphylococcus aureus?
- Staphylococcus aureus is a spherical, Gram-positive bacteria (coccus) that produces clusters that look like grapes.
- Facultative anaerobe: can grow in the presence or absence of oxygen
- Usually found on human skin and mucous membranes
- It can lead to a number of illnesses, such as pneumonia, skin infections, food poisoning, and toxic shock syndrome.
- MRSA (Methicillin-resistant Staphylococcus aureus) is a severe health problem because it is resistant to antibiotics.
- Sir Alexander Ogston found it in 1880 from infections in wounds.
- Makes poisons and enzymes that help it cause disease
- Important for investigations in clinical microbiology and infectious diseases
Key Takeaways
- Staphylococcus aureus is a widespread and adaptable bacteria that is very important in medicine. It is a round, Gram-positive, facultative anaerobic bacteria that usually grows in grape-like clusters. Cells are usually between 0.5 and 1 µm wide. It can’t move and doesn’t make spores.
- It can be both a commensal and an opportunistic pathogen. In 20–30% of humans, S. aureus lives in the nasal passages, skin, and mucous membranes without making them sick. But it is also an opportunistic pathogen that can cause a lot of other diseases.
- One big worry is that it is resistant to a lot of antibiotics, including MRSA. S. aureus is well-known for being resistant to antibiotics. Methicillin-resistant S. aureus (MRSA) was discovered in the 1960s. MRSA is a serious health hazard since it doesn’t respond to many antibiotics, which makes it harder to treat. Antibiotics can treat a lot of S. aureus infections, however MRSA needs different kinds of treatment.
- It can lead to many different kinds of infections. S. aureus can cause a wide range of disorders, from minor skin problems like pimples, boils (furuncles), carbuncles, cellulitis, and impetigo to more serious systemic diseases like pneumonia, osteomyelitis, endocarditis, sepsis (bacteremia), septic arthritis, and meningitis. It can also lead to toxin-mediated disorders including Staphylococcal Food Poisoning and Toxic Shock Syndrome (TSS).
- It can cause disease since it has a lot of virulence factors. S. aureus has a lot of virulence factors, such as adhesins (like Protein A and fibronectin-binding proteins that help it stick to tissues), toxins (like alpha-toxin, enterotoxins, and TSST-1 that can kill cells or cause a lot of cytokine release), and enzymes (like coagulase that makes plasma clots and helps the bacteria avoid the immune system, and hyaluronidase that helps it spread). It also makes biofilms, which make diseases last longer and make antibiotics less effective.
- It lives in a wide range of places outside people. S. aureus can be found in animals (especially livestock with infected udders), environmental reservoirs (soil, untreated water, and contaminated surfaces where it can survive on fomites for long periods of time), in the air (in hospitals, animal facilities, and public places), and it can also get into food and water.
- Different strains require different ways to find and cure them. Culture-based approaches (like Mannitol Salt Agar and CHROMagar™ Staph aureus), molecular methods (like PCR and qPCR), and immunological methods (like ELISA) are all used to find things. How to treat Methicillin-Susceptible For S. aureus (MSSA) infections, penicillinase-resistant penicillins or cephalosporins are usually used. For MRSA infections, vancomycin, daptomycin, or linezolid are usually used. Mupirocin and other topical medicines are used to treat localized infections or get rid of bacteria. For abscesses or infected tissues, surgery like drainage and debridement is usual.
- Good hygiene and infection control are very important for prevention. To avoid getting S. aureus infections, you should wash your hands often with soap and water or alcohol-based sanitizers, take care of your wounds properly (keeping cuts clean and covered), not share personal items, keep your environment clean (cleaning surfaces), and follow strict infection control rules in healthcare settings (contact precautions, single rooms, and decolonization strategies like mupirocin and chlorhexidine washes). There is no vaccination for S. aureus that you can buy right now, although research is still going on.
Discovery of Staphylococcus aureus
In 1880, Scottish surgeon Sir Alexander Ogston found Staphylococcus aureus in pus from surgical abscesses at the Aberdeen Royal Infirmary. He saw that it had clusters that looked like grapes and called it Staphylococcus.
In 1884, Friedrich Julius Rosenbach, a German scientist, used color and the ability to break down blood cells to tell S. aureus apart from S. epidermidis (previously S. albus).
In the early 1930s, coagulase testing made it easy to find S. aureus by finding its coagulase enzyme.
The discovery of penicillin in the 1940s was a big step forward in treating S. aureus infections, but by the end of the 1940s, penicillin resistance had started to show up.
Characteristics of Staphylococcus aureus
- Gram-positive -Gram-positive bacteria exhibit the ability to retain the crystal violet stain, resulting in a purple appearance when observed under a microscope.
- Cocci – Cocci are characterized by their spherical morphology, with a typical diameter ranging from 0.5 to 1.5 µm.
- Cluster formation – Cluster formation occurs when entities organize themselves into structures resembling clusters of grapes.
- Nonmotile – Characterized by the absence of flagella, this organism is classified as nonmotile.
- Non-spore-forming -Non-spore-forming organisms are characterized by their inability to produce spores.
- Facultative anaerobe – A facultative anaerobe is an organism capable of growth in both the presence and absence of oxygen.
- Catalase-positive -Catalase-positive organisms are characterized by their ability to produce the enzyme catalase.
- Coagulase-positive -Coagulase-positive organisms are characterized by their ability to produce the coagulase enzyme, which facilitates the process of blood clot formation.
- Salt-tolerant -Organisms exhibiting salt tolerance possess the ability to thrive in environments characterized by elevated concentrations of sodium chloride, with a tolerance threshold reaching up to 7.5% NaCl.
- Hemolytic -Hemolytic activity is characterized by the production of hemolysins, which induce the lysis of red blood cells.
- Pigmentation -The organism exhibits pigmentation, resulting in the formation of golden-yellow colonies on agar plates.
- Ferments mannitol – Ferments mannitol, resulting in the decolorization of mannitol salt agar to a yellow hue.
- Produces toxins -Generates a variety of toxins, which encompass alpha, beta, and delta toxins, as well as superantigens such as TSST-1.
- Forms biofilms -Biofilm formation is a significant factor in the persistence of chronic infections associated with medical devices.
- Antibiotic resistance -The phenomenon of antibiotic resistance, particularly in relation to methicillin-resistant strains of Staphylococcus aureus (MRSA), presents a significant challenge in contemporary medical practice.
Morphology Of Staphylococcus Aureus
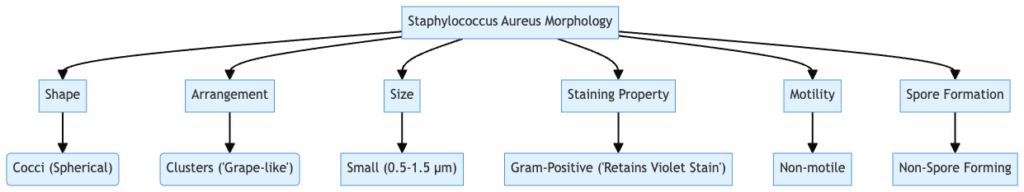
- Size – 0.5–1.5 µm in diameter
- Arrangement – Clusters resembling grape bunches
- Motility – Non-motile
- Spore Formation – Does not form spores
- Capsule – Present in some strains
- Gram Staining – Purple coloration due to thick peptidoglycan layer
- Catalase Test – Catalase-positive (bubbles when exposed to hydrogen peroxide)
- Coagulase Test – Coagulase-positive (clots plasma)
- Hemolysis on Blood Agar – Beta-hemolytic (clear zone around colonies)
- Pigmentation – Golden-yellow colonies due to carotenoid pigments
- Growth Conditions – Facultative anaerobe, grows in 10–42°C, pH 4.2–9.3
- Biofilm Formation – Can form biofilms, especially in the presence of plasma
Habitat of Staphylococcus aureus
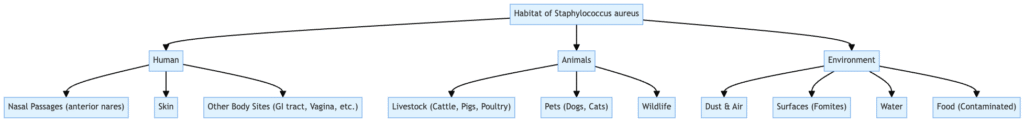
Humans
- Nasal passages, skin, mucous membranes (mouth, throat, axillae, groin, perineal area)
- Up to 50% of adults colonized; 15% persistently in anterior nares
- Higher prevalence in healthcare workers, diabetics, IV drug users, hospitalized, and immunocompromised individuals
Animals
- Livestock (pigs, cows), particularly with infected udders
- Detected in farm environments, including air and soil
- Zoonotic transmission possible through direct or indirect contact
Environmental Reservoirs
- Soil, untreated water, contaminated surfaces
- Survives on fomites for extended periods; up to 7 months under certain conditions
- Detected in recreational waters, especially post-storm runoff
Airborne Presence
- Found in hospital air, animal breeding facilities, wastewater treatment plants, and public spaces
- Can be transmitted via bioaerosols, posing occupational and public health risks
Food and Water
- Contaminates meat, dairy products, and seafood
- Associated with foodborne outbreaks due to enterotoxin production
Biochemical characteristics of Staphylococcus aureus
| Test | Observation |
| Catalase | Positive |
| Indole | Negative |
| Citrate | Positive |
| Methyl red | Positive |
| Voges-proskauer | Negative |
| Gelatin hydrolysis | Negative |
Fermentable sugar
| Fermentable sugar | Observation |
| Glucose | Acid production |
| Galactose | Acid production |
| Lactose | Acid production |
| Mannitol | |
| Maltose | Acid production |
| Sucrose | Acid production |
| Starch | No acid production |
Cultural Characteristics of Staphylococcus Aureus
- NAM (Nutrient Agar Medium):
- Circular shape,
- 2-4 mm in Size,
- Smooth Surface,
- Golden yellow color,
- Opaque Structure,
- Easily emulsifiable.
- MacConkey agar medium:
- Circular shape,
- 2-4 mm in Size,
- Smooth Surface,
- Pink,
- Opaque Structure,
- Easily emulsifiable.
- Blood Agar Medium:
- Circular shape,
- 1-4 mm in Size,
- Smooth Surface,
- Light golden yellow, surrounded by clear zone (beta hemolysis).
- Opaque Structure,
- Easily emulsifiable.
- Mannitol Salt Agar:
- Circular shape,
- 2-4 mm in Size,
- Smooth Surface,
- Yellow,
- Opaque Structure,
- Easily emulsifiable.
- Milk Agar:
- Circular shape,
- 3-5 mm in Size,
- Smooth Surface,
- Golden yellow (Pigment production enhanced).
- Opaque Structure,
- Easily emulsifiable.
- Brain heart infusion agar:
- Circular shape,
- 3-5 mm in Size,
- Smooth Surface,
- Yellow pigmented colonies.
- Opaque Structure,
- Easily emulsifiable.
- Tryptic Soy Agar: circular, convex, and entire margin.
- Tellurite-polymyxin-egg yolk: Egg yolk reaction, Black colonies.
- Phosphatase medium: Phosphatase production.
- DNAse medium: Deoxyribonuclease production.
- Polymyxin-coagulase-Mannitol: Coagulase reaction, Mannitol fermentation.
- Columbia CNA (Staph/Strep selective medium): Pigment Haemolysis.
- Egg yolk-azide: Egg yolk reaction.
- KRANEP: Mannitol fermentation, Egg yolk reaction, Pigment production
- Staph 4S: Egg yolk reaction, Grey/dark-grey colonies.
- Staph 110: Mannitol fermentation, Gelatin liquefaction, Pigment production, Egg yolk reaction.
- Improved Vogel and Johnson (PCVJ): Black colonies, Mannitol fermentation, DNAse production.
- Vogel and Johnson: Black colonies, Mannitol fermentation.
- Rabbit plasma-fibrinogen (RPF): Coagulase reaction, White or grey or black colonies.
Virulence factors of Staphylococcus aureus
- Adhesins
- Protein A – Binds Fc region of IgG, inhibiting opsonization and phagocytosis
- Fibronectin-binding proteins (FnBPA/B) – Facilitate attachment to host tissues and biofilm formation
- Clumping factor (ClfA/B) – Mediates binding to fibrinogen and platelets
- Collagen-binding protein – Promotes adherence to extracellular matrix components
- Toxins
- Alpha-toxin (α-hemolysin) – Forms heptameric pores in host cell membranes, causing cytolysis
- Beta-toxin (β-hemolysin) – Sphingomyelinase activity, leading to membrane disruption
- Delta-toxin (δ-hemolysin) – Detergent-like activity, lyses host cells non-specifically
- Panton–Valentine leukocidin (PVL) – Bicomponent toxin causing lysis of neutrophils and macrophages
- Exfoliative toxins (ETA/ETB) – Serine proteases cleaving desmoglein-1, leading to skin blistering
- Toxic shock syndrome toxin-1 (TSST-1) – Superantigen inducing massive cytokine release, causing shock
- Staphylococcal enterotoxins (SEA–SEZ) – Heat-stable toxins causing food poisoning
- Enzymes
- Coagulase – Converts fibrinogen to fibrin, promoting clot formation and immune evasion
- Hyaluronidase – Degrades hyaluronic acid in connective tissues, facilitating spread
- Staphylokinase – Dissolves fibrin clots, aiding in tissue invasion
- Lipases – Hydrolyze lipids, aiding in survival on skin and mucous membranes
- Nuclease – Degrades extracellular DNA, aiding in biofilm formation and evasion of neutrophil traps
- β-lactamase – Breaks down β-lactam antibiotics, conferring resistanceFrontiers
- Immune Evasion Factors
- Capsule – Polysaccharide layer inhibiting phagocytosis
- Protein A – Binds IgG Fc region, preventing opsonization
- Staphylococcal complement inhibitor (SCIN) – Inhibits complement activation
- Chemotaxis inhibitory protein of S. aureus (CHIPS) – Blocks neutrophil chemotaxis
- Phenol-soluble modulins (PSMs) – Induce inflammation and neutrophil recruitment; cytolytic activity
- Staphylococcal superantigen-like proteins (SSLs) – Modulate immune responses to enhance survival
- Biofilm Formation
- Polysaccharide intercellular adhesin (PIA) – Component of biofilm matrix
- Extracellular DNA (eDNA) – Structural component of biofilm
- Teichoic acids – Contribute to biofilm formation and antibiotic resistance
- Regulatory Systems
- Accessory gene regulator (agr) system – Quorum-sensing system regulating virulence factor expression
- Two-component systems – Regulate response to environmental stimuli and antibiotic stress
- Miscellaneous Factors
- Staphyloxanthin – Carotenoid pigment providing resistance to reactive oxygen species
- Type VII secretion system (T7SS) – Secretes effector proteins contributing to virulence and interbacterial competition
These multifaceted virulence factors enable Staphylococcus aureus to colonize host tissues, evade immune responses, and cause a wide range of infections.

Methods for Detection and Enumeration of S. aureus
Detection and Enumeration methods of Staphylococcus aureus;
- Culture-Based Methods
- Baird-Parker Agar
- Selective and differential medium
- Contains lithium chloride and potassium tellurite to inhibit non-staphylococcal organisms
- Coagulase-positive colonies appear black with a clear zone due to lecithinase activity
- Mannitol Salt Agar (MSA)
- Selective for staphylococci due to high salt concentration
- Differential for mannitol fermentation; S. aureus ferments mannitol, turning the medium yellow
- CHROMagar™ Staph aureus
- Chromogenic medium for direct detection
- S. aureus colonies appear pink to purple after 18–24 hours of incubation
- RAPID’Staph Medium
- Reduces incubation time to 24 hours
- Utilizes egg yolk tellurite emulsion for selective growth and differentiation
- Baird-Parker Agar
- Enumeration Techniques
- Direct Plate Count
- Suitable for foods with >100 S. aureus cells/g
- Involves serial dilution and plating on selective media
- Most Probable Number (MPN) Method
- Used for low bacterial counts
- Involves multiple tube dilutions and statistical estimation
- Optical Density (OD) Measurement
- Rapid but may be inaccurate due to bacterial aggregation
- Sonication can disperse aggregates for more accurate OD readings
- Petrifilm™ Plates
- Pre-prepared plates for rapid enumeration
- Useful for food industry applications
- Direct Plate Count
- Molecular Methods
- Polymerase Chain Reaction (PCR)
- Detects specific genes associated with S. aureus
- Allows for rapid and sensitive detection
- Quantitative PCR (qPCR)
- Quantifies S. aureus DNA
- Provides information on bacterial load
- Polymerase Chain Reaction (PCR)
- Immunological Methods
- Enzyme-Linked Immunosorbent Assay (ELISA)
- Detects enterotoxins produced by S. aureus
- Useful for determining the potential for foodborne illness
- Enzyme-Linked Immunosorbent Assay (ELISA)
- Rapid Detection Systems
- Aptamer-Based Impedimetric Sensors
- Utilize DNA aptamers for specific binding
- Offer rapid and sensitive detection
- Raman Spectroscopy with Deep Learning
- Provides rapid, label-free identification
- Capable of distinguishing between MRSA and MSSA
- Aptamer-Based Impedimetric Sensors
Staphylococcus Species Identification
Coagulase test
- Differentiates Staphylococcus aureus (coagulase-positive) from coagulase-negative staphylococci (SCN)
- Two methods:
- Tube coagulase test detects extracellular free coagulase converting fibrinogen to fibrin
- Slide coagulase test detects cell wall-bound coagulase (clumping factor) via agglutination
- Tube test procedure: large colony mixed with 0.5 ml rabbit plasma, incubated at 37°C for 4 hours, clot formation observed by tilting tube 90°
- Positive: any degree of coagulation excluding fibrous precipitates; negative: no clot after 18 hours
- False negatives possible with staphylokinase-producing strains (clot lysis after formation)
- Note: citrate plasma may cause false positives due to citrate metabolism by some bacteria (Enterococcus, Pseudomonas, Serratia, Streptococcus)
- Slide test procedure: suspension emulsified on slide with rabbit plasma, agglutination indicates bound coagulase
- Less sensitive and specific than tube test; control saline test required to exclude autoagglutination
- S. lugdunensis and S. schleiferi may test positive on slide test despite being SCN
Agglutination test
- Rapid identification of Staphylococcus aureus using antibodies against surface antigens
- Includes rapid latex and hemagglutination tests (e.g., Pastorex Staph-Plus, Slidex Staph Plus, Staphaurex Plus, Staphytect Plus)
- Uses monoclonal antibodies targeting common capsular polysaccharide serotypes (1, 5, 6, 8, 10)
- Visible agglutination indicates positive result
- Faster than conventional coagulase tests but must be interpreted cautiously due to possible false positives or negatives
DNase test
- Identifies bacteria producing deoxyribonuclease enzymes (notably S. aureus and S. schleiferi)
- Uses DNA agar medium where DNase activity hydrolyzes DNA, visible as clear halo after adding hydrochloric acid (which precipitates intact DNA)
- Clear halo around colonies indicates positive DNase activity
Novobiocin resistance test
- Differentiates S. saprophyticus (novobiocin-resistant) from other staphylococci (generally novobiocin-sensitive)
- Agar diffusion test on Mueller-Hinton agar with 5 µg novobiocin disc
- Inoculum matched to 0.5 McFarland standard, incubated at 35–37°C for 18–24 hours
- Resistance indicated by inhibition zone ≤16 mm diameter
Ornithine decarboxylase test
- Identifies S. lugdunensis among coagulase-negative staphylococci by ornithine decarboxylase activity
- Inoculation in decarboxylase medium with 1% ornithine, incubated overnight
- S. lugdunensis is positive at 8 hours, whereas S. epidermidis may be positive only at 24 hours, allowing differentiation
Complete identification of staphylococci
Biochemical Identification
- API Staph®
- Miniaturized test system for overnight identification of staphylococci and micrococci.
- Involves 20 microtubes with dehydrated substrates.
- Results interpreted based on color changes after incubation.
- Identifies various staphylococcal species through metabolic profiles.
- ID 32 Staph®
- Similar to API Staph® but includes 32 tests for enhanced identification.
- Suitable for clinical and veterinary applications.
- Provides rapid and accurate identification of staphylococci.
- RAPIDEC® Staph
- Rapid identification system for commonly occurring staphylococci.
- Results available in approximately 2 hours.
- Utilizes enzymatic reactions for species identification.
Nucleic Acid-Based Identification
- DNA Extraction
- Requires special cell lysis conditions.
- Enzymes like lysostaphin, lysozyme, proteinase K, and achromopeptidase may be used.
- Facilitates the release of nucleic acids for subsequent analysis.
- Universal Targets for Staphylococci
- 16S and 23S rRNA genes: Common targets for bacterial identification.
- tuf, gyrA, sodA, gap, HSP60/GroE genes: Alternative universal targets for staphylococci.
- Specific Targets for S. aureus
- nuc gene: Encodes thermostable nuclease; highly specific for S. aureus.
- clfA, coa, sodM, femA, femB genes: Additional targets for S. aureus identification.
- staphylococcal insertion element 431: Specific to methicillin-resistant S. aureus (MRSA).
Note: Misidentifications can occur, especially with fem-negative S. aureus and coagulase-negative staphylococci (CoNS) strains possessing femA-related genes.
Infections Caused by Staphylococcus aureus and Symptoms
- Skin and Soft Tissue Infections
- Boils (Furuncles) – Painful, pus-filled lumps arising from hair follicles.
- Carbuncles – Cluster of boils with interconnected abscesses.
- Cellulitis – Red, swollen, warm skin; may have blisters or pus.
- Impetigo – Contagious rash with honey-colored crusts; common in children.
- Bullous Impetigo – Large fluid-filled blisters; often in infants.
- Staphylococcal Scalded Skin Syndrome (SSSS) – Widespread redness, blisters, and peeling skin; affects infants and immunocompromised adults.
- Folliculitis – Inflammation of hair follicles; may form pustules.
- Systemic Infections
- Bacteremia – Fever, chills, hypotension; can lead to septic shock.
- Endocarditis – Fever, heart murmur, embolic phenomena (e.g., Osler nodes, Janeway lesions).
- Osteomyelitis – Bone pain, swelling, fever; often affects long bones in children and vertebrae in adults.
- Septic Arthritis – Joint pain, swelling, warmth; commonly affects knee and hip joints.
- Pneumonia – Cough, chest pain, fever, difficulty breathing; can lead to abscess formation.
- Meningitis – Headache, fever, neck stiffness; less common but severe.
- Orbital Cellulitis – Eye pain, swelling, fever; can lead to vision loss if untreated.
- Toxin-Mediated Syndromes
- Toxic Shock Syndrome (TSS) – High fever, hypotension, rash resembling sunburn, multi-organ failure; associated with tampon use or surgical wounds.
- Staphylococcal Food Poisoning – Rapid onset nausea, vomiting, abdominal cramps, diarrhea; symptoms usually resolve within 24 hours.
- Staphylococcal Enteritis – Abdominal pain, cramping, diarrhea, fever; caused by ingestion of enterotoxin-contaminated food.
- Other Infections
- Mastitis – Breast pain, swelling, redness; common in lactating women.
- Prosthetic Joint Infections – Pain, swelling, fever; often occurs after joint replacement surgery.
- Bacteriuria – Presence of bacteria in urine; may be asymptomatic or cause urinary tract symptoms.
Culture and Culture Environments of Staphylococcus
General Growth Conditions
- Facultative anaerobes- can grow with or without oxygen
- Temperature range- 18–40°C; optimal at 37°C
- pH -neutral to slightly alkaline environments
- Salt tolerance- can grow in up to 10% NaCl
- Catalase-positive, oxidase-negative
Common Culture Media
Common Culture Media used for Staphylococcus;
- Nutrient Agar/Broth
- Supports general growth of staphylococci
- Brain Heart Infusion (BHI) Broth
- Promotes rapid growth and is ideal for virulence factor expression
- Mannitol Salt Agar (MSA)
- Selective and differential medium
- High salt concentration (7.5%) inhibits non-halophilic organisms
- Mannitol fermentation by S. aureus lowers pH, turning the medium yellow
- Baird-Parker Agar
- Selective for coagulase-positive staphylococci
- Contains lithium chloride and tellurite to inhibit contaminants
- Colonies appear black with clear zones due to lecithinase activity
- Vogel–Johnson Agar
- Selective for coagulase-positive staphylococci
- Contains mannitol and lithium chloride
- Colonies appear black with a yellow halo due to mannitol fermentation
- CHROMagar™ Staph aureus
- Chromogenic medium for direct detection
- S. aureus colonies appear mauve
- Results in 18–24 hours at 35–37°C
- HiCrome MeReSa Agar
- Chromogenic medium for methicillin-resistant S. aureus (MRSA)
- S. aureus colonies appear bluish-green
Environmental Conditions for Cultivation
- Oxygen Requirements: Facultative anaerobes; grow in both aerobic and anaerobic conditions
- Temperature: Optimal growth at 37°C; can grow between 18–40°C
- pH: Prefer neutral to slightly alkaline conditions
- Salt Concentration: Tolerant to high salt concentrations, up to 10% NaCl
Specialized Media for Virulence Factor Expression
- Casein Hydrolysate Media
- Used to induce enterotoxin production in S. aureus
- Contains hydrolyzed casein as a source of amino acids and various minerals
Co-culture Considerations
- In mixed cultures, the growth medium can influence the interaction between S. aureus and other species like Pseudomonas aeruginosa
- The ratio of ATP to growth rate (absolute growth) can determine the final population composition in co-cultures
Storage and Stability of Media
- Prepared media should be stored according to manufacturer’s instructions to maintain efficacy
- Some media, like CHROMagar™ Staph aureus, are stable without the need for supplementation
Treatment of Staphylococcus aureus
Treatment of Staphylococcus aureus Infections
- Methicillin-Susceptible S. aureus (MSSA)
- First-line therapy:
- Penicillinase-resistant penicillins:
- Nafcillin
- Oxacillin
- Cephalosporins:
- Cefazolin
- Penicillinase-resistant penicillins:
- Alternative agents:
- Clindamycin
- Trimethoprim-sulfamethoxazole (TMP-SMX)
- Doxycycline
- Severe infections:
- Parenteral administration recommended
- Duration varies based on infection type
- First-line therapy:
- Methicillin-Resistant S. aureus (MRSA)
- First-line therapy:
- Vancomycin
- Daptomycin
- Linezolid
- Alternative agents:
- Clindamycin (if susceptible)
- TMP-SMX
- Doxycycline
- Ceftaroline
- Tedizolid
- Vancomycin-resistant strains (VRSA):
- Combination therapy with:
- Daptomycin
- Linezolid
- Quinupristin-dalfopristin
- Telavancin
- Combination therapy with:
- Vancomycin-intermediate strains (VISA):
- High-dose daptomycin
- Combination therapy with:
- Rifampin
- Gentamicin
- TMP-SMX
- First-line therapy:
- Topical Agents
- Mupirocin:
- Effective for localized skin infections
- Used for decolonization in nasal carriers
- Mupirocin:
- Surgical Interventions
- Drainage:
- Incision and drainage for abscesses
- Debridement:
- Removal of infected tissue in osteomyelitis or endocarditis
- Drainage:
- Duration of Therapy
- Uncomplicated infections:
- 7–14 days
- Complicated infections:
- 4–6 weeks
- Bloodstream infections:
- Minimum 14 days of intravenous therapy
- Consideration for oral step-down therapy after clinical improvement
- Uncomplicated infections:
- Adjunctive Therapies
- Rifampin:
- Used in combination for biofilm-associated infections
- Chlorhexidine washes:
- For skin decolonization
- Rifampin:
Prevention of Staphylococcus aureus Infection
These common sense precautions can reduce the risk of getting Staph infections, How to Keep Staphylococcus aureus from Getting In
- Hygiene for Yourself
- Use soap and water to wash your hands often.
- When you can’t get soap and water, use hand sanitizers that are made with alcohol.
- Before sharing, clean and disinfect things like razors and towels.
- Don’t share things like razors, towels, and needles that belong to you.
- Taking care of wounds
- Until they heal, keep cuts, scrapes, and wounds clean and covered with bandages.
- Follow your healthcare provider’s advice for how to care for your wound.
- Don’t pick at or pop sores.
- Throw away tape and bandages with the ordinary trash.
- Hygiene in the Environment
- Wipe down and clean doorknobs, light switches, and gym equipment often.
- Follow the manufacturer’s recommendations for using disinfectants, including how long they should be in contact with the surface.
- Don’t spray or fog rooms with disinfectants; cleaning specific areas is more effective.
- Places of Health Care
- Use contact precautions, such gowns and gloves, for patients who have MRSA or are colonized with it.
- If you can, put patients in single rooms. If you can’t, keep at least three feet between them.
- Teach healthcare workers how to prevent MRSA and follow infection control rules.
- Ways to Decolonize
- If a patient has MRSA, think about nasal decolonization with mupirocin and daily body washes with chlorhexidine in high-risk hospital settings.
- Universal decolonization has been found to lower the number of infections, but it may also make people more resistant. Targeted techniques are being tested.
- Community Settings
- Make sure to wash your hands well, especially after working out.
- Don’t share things like razors and towels that are personal to you.
- Cover and clean wounds.
- Be careful in places like gyms and locker rooms where people often touch each other’s skin.
- Safety with Food
- Before and after you handle food, wash your hands.
- Make sure to cook meat to safe temperatures.
- Put leftovers in the fridge right away.
- To keep things from getting dirty, clean the kitchen surfaces and tools often.
Antibiotic sensitivity of Staphylococcus aureus
- Penicillin-sensitive strains – Rare today; historically sensitive, but most now produce β-lactamase.
- Penicillin-resistant strains – Most strains produce penicillinase (a type of β-lactamase) that inactivates penicillin.
- Methicillin-sensitive S. aureus (MSSA) – Sensitive to methicillin, oxacillin, nafcillin, cloxacillin, dicloxacillin.
- Methicillin-resistant S. aureus (MRSA) – Resistant to all β-lactam antibiotics (penicillins + cephalosporins) due to mecA gene encoding altered penicillin-binding protein (PBP2a).
- MRSA treatment options –
- Vancomycin
- Teicoplanin
- Linezolid
- Daptomycin
- Clindamycin (if D-test negative)
- Trimethoprim-sulfamethoxazole (TMP-SMX)
- Doxycycline or minocycline
- Vancomycin-intermediate S. aureus (VISA) – Reduced sensitivity to vancomycin (MIC 4–8 µg/mL); thickened cell wall.
- Vancomycin-resistant S. aureus (VRSA) – Rare, true resistance (MIC ≥16 µg/mL); carries vanA gene from Enterococcus.
- Multidrug-resistant S. aureus – Some strains show resistance to fluoroquinolones, macrolides, aminoglycosides.
- Antibiotic susceptibility testing – Done via disk diffusion (Kirby-Bauer), MIC testing, or automated systems like VITEK.
- Treatment note – Always guided by antibiotic sensitivity pattern due to evolving resistance.
Quiz
What is the characteristic shape of Staphylococcus aureus cells?
a) Rod-shaped
b) Spiral
c) Square
d) Spherical (cocci)
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: d) Spherical (cocci) [/expand]
Which of the following describes the arrangement of Staphylococcus aureus cells under a microscope?
a) Chains
b) Grape-like clusters
c) Pairs
d) Single
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: b) Grape-like clusters [/expand]
What is the size of an individual Staphylococcus aureus cell?
a) 0.5 microns
b) 2 microns
c) 1 micron
d) 3 microns
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: c) 1 micron [/expand]
Is Staphylococcus aureus motile?
a) Yes
b) No
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: b) No [/expand]
Which of the following is true regarding the flagellation of Staphylococcus aureus?
a) Flagellated
b) Non-flagellated
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: b) Non-flagellated [/expand]
Does Staphylococcus aureus produce spores?
a) Yes
b) No
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: b) No [/expand]
Which strains of Staphylococcus aureus possess a capsule?
a) All strains
b) No strains
c) Some strains
d) Only virulent strains
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: c) Some strains [/expand]
What is the result of a Gram stain test for Staphylococcus aureus?
a) Gram-negative
b) Gram-positive
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: b) Gram-positive [/expand]
Which of the following diseases is NOT associated with Staphylococcus aureus?
a) Tuberculosis
b) Food poisoning
c) Skin infections
d) Pneumonia
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: a) Tuberculosis [/expand]
Which of the following is a common site for Staphylococcus aureus colonization in humans?
a) Stomach
b) Nasal passages
c) Lungs
d) Kidneys
[expand title=”Show answer” swaptitle=”Hide answer”] Answer: b) Nasal passages [/expand]
FAQ
What is Staphylococcus aureus?
Staphylococcus aureus is a type of bacteria commonly found on the skin and in the nasal passages of healthy individuals. It can cause a range of illnesses, from minor skin infections to severe diseases.
How is Staphylococcus aureus transmitted?
Staphylococcus aureus can be transmitted through direct skin-to-skin contact, contact with contaminated surfaces, or by inhaling airborne droplets from an infected person.
What types of infections can Staphylococcus aureus cause?
Staphylococcus aureus can cause various infections, including skin infections, pneumonia, food poisoning, bloodstream infections, and more.
Is Staphylococcus aureus the same as MRSA?
No, MRSA (Methicillin-resistant Staphylococcus aureus) is a strain of Staphylococcus aureus that is resistant to many antibiotics, making it more challenging to treat.
How can Staphylococcus aureus infections be prevented?
Good hygiene practices, including regular hand washing, keeping wounds clean and covered, and avoiding contact with infected individuals, can help prevent the spread of Staphylococcus aureus.
Are Staphylococcus aureus infections treatable?
Yes, many Staphylococcus aureus infections can be treated with antibiotics. However, some strains, like MRSA, are resistant to certain antibiotics and may require alternative treatments.
Can Staphylococcus aureus cause food poisoning?
Yes, Staphylococcus aureus can produce toxins in improperly stored food, leading to food poisoning symptoms like nausea, vomiting, and diarrhea.
Why is MRSA a concern in hospitals?
MRSA is of particular concern in hospitals because it is resistant to many antibiotics, can spread easily in healthcare settings, and can cause severe infections in already vulnerable patients.
Can Staphylococcus aureus infections recur?
Yes, individuals can get re-infected with Staphylococcus aureus, especially if they are in environments where the bacteria are prevalent or if they have weakened immune systems.
Is there a vaccine for Staphylococcus aureus?
As of now, there is no commercially available vaccine for Staphylococcus aureus, but research is ongoing in this area.
- Leung, Y.L. (2014). Encyclopedia of Toxicology || Staphylococcus aureus. , (), 379–380. doi:10.1016/b978-0-12-386454-3.00539-x
- Martin, E. (2014). Encyclopedia of Food Microbiology || STAPHYLOCOCCUS | Staphylococcus aureus. , (), 501–507. doi:10.1016/b978-0-12-384730-0.00317-7
- Bose, J.L. (2013). Brenner’s Encyclopedia of Genetics || Staphylococcus aureus. , (), 553–555. doi:10.1016/b978-0-12-374984-0.01473-x
- Foster, Timothy J. (2015). Molecular Medical Microbiology || Staphylococcus aureus. , (), 655–674. doi:10.1016/B978-0-12-397169-2.00037-8
- Adejuwon, Adekunle Odunayo & Ogunkanmbi, David & Adejumoke, Mary & Bisi-Johnson, Mary & Fadeyi, Bridget & Agboola, Oyinade & Adejuwon, Adebanke. (2011). Staphylococcus aureus isolated from septic caesaerean wound at Ile Ife Nigeria: Antibiotics susceptibility patterns. International Journal of Medicine and Medical Sciences. 3. 149-154.
- Amit Karmakar, Parimal Dua, Chandradipa Ghosh, “Biochemical and Molecular Analysis of Staphylococcus aureus Clinical Isolates from Hospitalized Patients”, Canadian Journal of Infectious Diseases and Medical Microbiology, vol. 2016, Article ID 9041636, 7 pages, 2016. https://doi.org/10.1155/2016/9041636
- Silva, Wladimir Padilha da et al. Biochemical characteristics of typical and atypical Staphylococcus aureus in mastitic milk and environmental samples of Brazilian dairy farms.
- Brazilian Journal of Microbiology [online]. 2000, v. 31, n. 2 [Accessed 19 March 2022] , pp. 103-106. Available from: <https://doi.org/10.1590/S1517-83822000000200008>. Epub 04 Oct 2000. ISSN 1678-4405. https://doi.org/10.1590/S1517-83822000000200008.
- Adejuwon, Adekunle Odunayo & Ajayi, Adesola & Akintunde, O & Olutiola, Patrick. (2022). Antibiotics resistance and susceptibility pattern of a strain of Staphylococus aureus associated with acne.
- Oogai Y, Matsuo M, Hashimoto M, Kato F, Sugai M, Komatsuzawa H. Expression of virulence factors by Staphylococcus aureus grown in serum. Appl Environ Microbiol. 2011;77(22):8097-8105. doi:10.1128/AEM.05316-11
- Cheung GYC, Bae JS, Otto M. Pathogenicity and virulence of Staphylococcus aureus. Virulence. 2021;12(1):547-569. doi:10.1080/21505594.2021.1878688
- https://www.pasteur.fr/en/medical-center/disease-sheets/staphylococci
- https://www.mayoclinic.org/diseases-conditions/staph-infections/symptoms-causes/syc-20356221
- https://apic.org/monthly_alerts/staphylococcus-aureus/
- https://www.news-medical.net/health/What-is-Staphylococcus-Aureus.aspx
- https://www.health.state.mn.us/diseases/staph/basics.html
- https://www.cdc.gov/hai/organisms/staph.html
- https://www.msdmanuals.com/en-in/home/infections/bacterial-infections-gram-positive-bacteria/staphylococcus-aureus-infections
- https://www.news-medical.net/health/Staphylococcus-Aureus-Virulence-Factors.aspx
- https://www.ncbi.nlm.nih.gov/books/NBK441868/
- https://en.wikipedia.org/wiki/Staphylococcus_aureus
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2218046/pdf/jhyg00140-0078.pdf
- https://paramedicsworld.com/staphylococcus-aureus/morphology-culture-characteristics-staphylococcus-aureus/medical-paramedical-studynotes