What is Skin?
- The skin is the body’s largest organ, forming a protective outer layer that covers the entire body and is essential to human health. Composed of multiple layers of ectodermal tissue, the skin shields underlying muscles, bones, ligaments, and internal organs from external harm. In humans, skin resembles that of many mammals, particularly pig skin, and while most areas of human skin contain hair follicles, it may appear hairless in places. Broadly, skin is classified into two types: hairy and glabrous (hairless) skin. The term “cutaneous” specifically refers to the skin, derived from the Latin word cutis.
- One of the skin’s primary roles is to act as a protective barrier. It defends the body against pathogens and helps prevent excessive water loss. Additionally, the skin provides insulation, regulates body temperature, and allows for sensory perception of touch, heat, and cold. It also synthesizes essential vitamins, including vitamin D, and protects vitamin B folates. When damaged, the skin attempts to heal itself, often forming scar tissue, which may differ in color and pigmentation from surrounding areas.
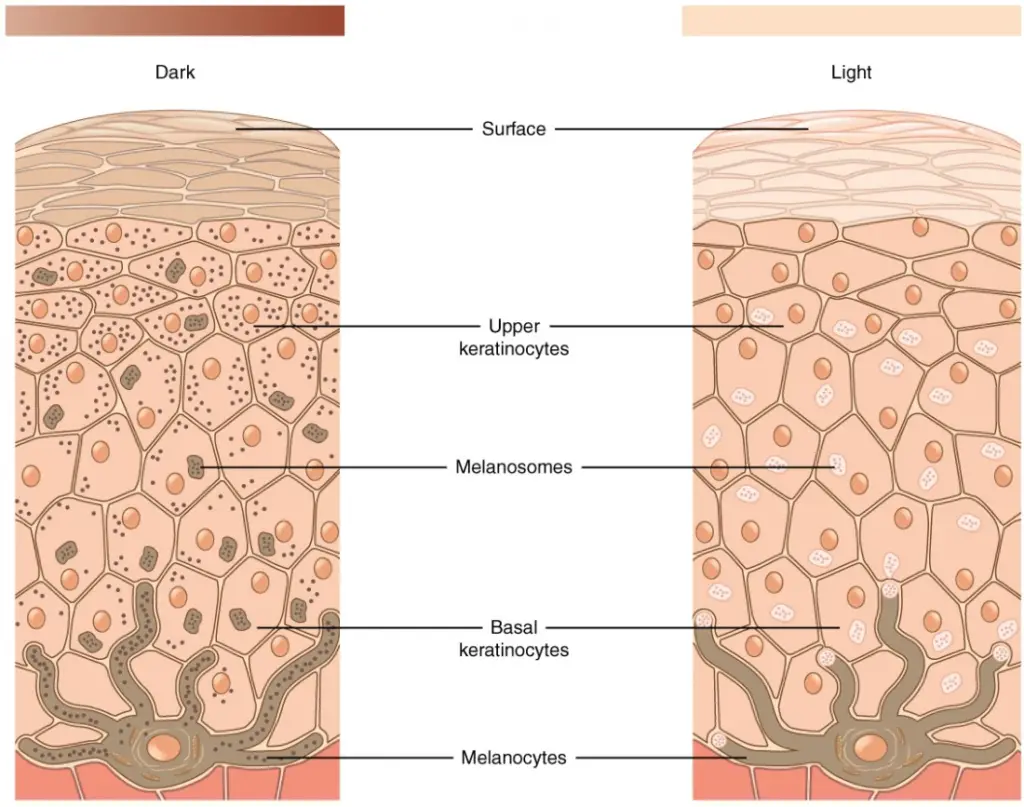
- Skin characteristics, such as pigmentation and texture, vary widely across individuals and populations. Pigmentation is largely influenced by melanin levels, leading to a range of skin tones. Skin also varies in terms of moisture and oil levels, ranging from dry to oily. This diversity creates a unique environment that supports approximately a thousand bacterial species from nineteen different phyla.
- In terms of structure, the skin consists of layers that vary in thickness depending on location. For instance, the skin beneath the eyes is thin and delicate, while the skin on the palms and soles is much thicker to withstand regular impact and friction. Spanning roughly 20 square feet, the skin acts as an interface between the body and the external environment, protecting vital organs, muscles, and bones from potential hazards.
- Overall, the skin is an intricate and dynamic organ, performing a wide array of critical functions to maintain bodily health and resilience.
Definition of Skin
Skin is the body’s largest organ, serving as a protective outer layer that covers and shields internal organs, muscles, and bones. It regulates body temperature, enables sensory perception, synthesizes vitamins, and acts as a barrier against pathogens and environmental damage.
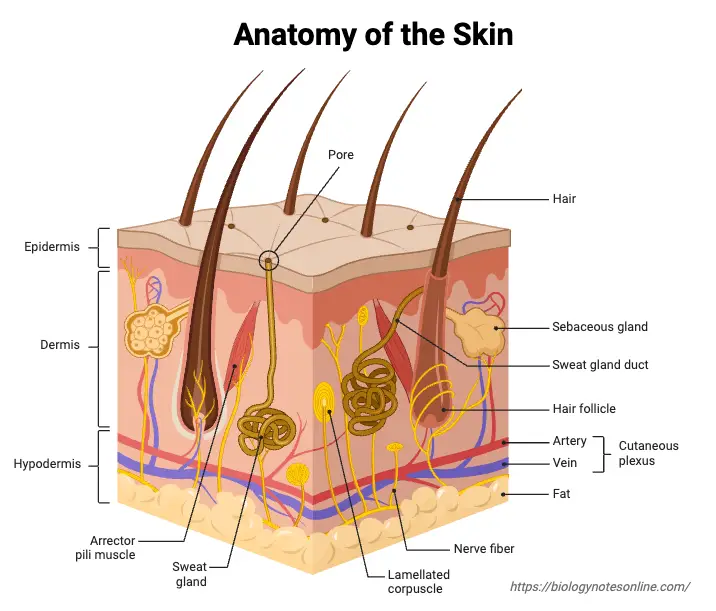
Gross Structure of Skin
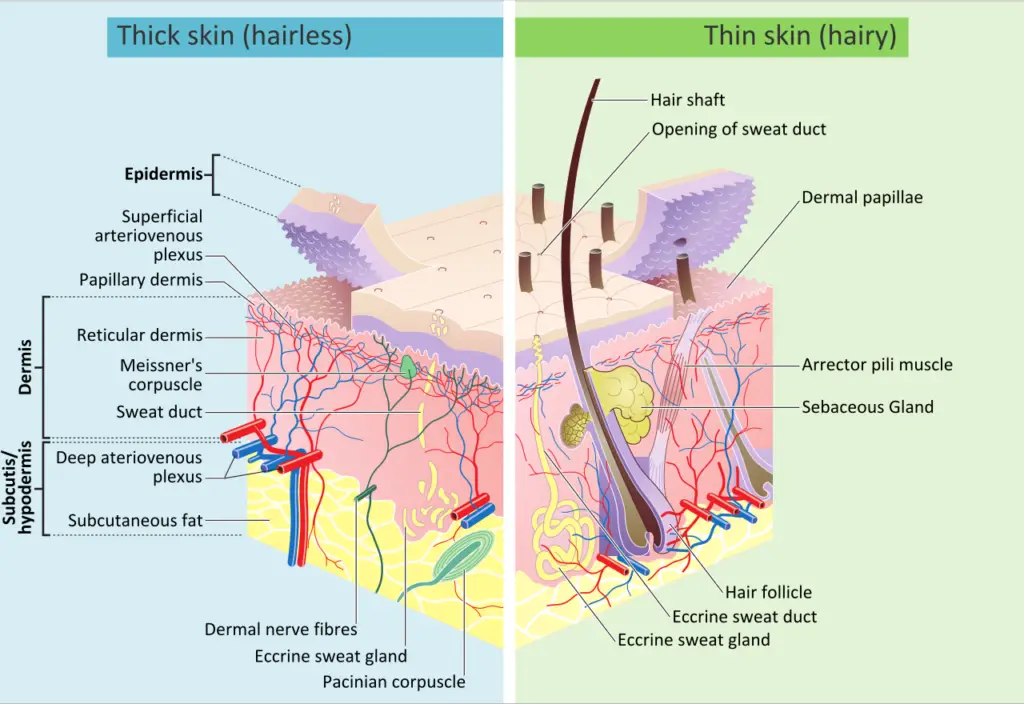
The skin’s composition varies across different parts of the body, adapting its structure and thickness based on location and function. It may be thin and hairy or thick and hairless. For example, glabrous skin—thicker, hairless skin—is found on the palms, soles, and the flexor surfaces of the fingers to enhance protection and grip. In general, the skin comprises three main layers: the epidermis, dermis, and hypodermis. Each layer performs distinct roles essential for the skin’s protective, sensory, and regulatory functions.
- Epidermis: This is the outermost layer of the skin, providing a direct barrier against the environment. It consists of tightly packed cells, which make it highly effective at shielding internal structures from pathogens, chemicals, and physical impacts. The epidermis continuously renews itself as old cells are shed and replaced by new cells produced in its basal layer, helping maintain the skin’s integrity and resilience. This layer also plays a significant role in water retention and is the site where skin pigmentation, influenced by melanin, occurs.
- Dermis: Situated beneath the epidermis, the dermis provides structural strength and elasticity to the skin. It contains connective tissues composed of collagen and elastin fibers, which give the skin flexibility and durability. Besides its supportive role, the dermis houses various vital components, including blood vessels, nerve endings, sweat glands, and hair follicles. These structures enable the skin to sense touch, temperature, and pain, regulate body temperature through sweat production, and maintain hair growth. Additionally, the dermal blood vessels supply nutrients and oxygen to both the dermis and epidermis, fostering skin health.
- Hypodermis (also known as the subcutaneous layer): The deepest layer, the hypodermis, primarily consists of fat and connective tissue. It serves as insulation, conserving body heat, and acts as a cushion to absorb external shocks and protect underlying muscles and bones. The fat cells in the hypodermis also store energy, which the body can access when needed. This layer anchors the skin to underlying tissues, ensuring stability and flexibility.
Ultrastructure of Skin – Layers of the Skin
The skin comprises three primary layers, each with specific structures and cells that contribute to its protective, regulatory, and sensory functions. These layers work together to maintain skin integrity and respond to external stimuli.
- Epidermis: This is the skin’s outermost layer and serves as the primary barrier against environmental hazards. The thickness of the epidermis varies significantly depending on the body area, from as thin as 0.05 mm on the eyelids to about 1.5 mm on the palms and soles. Within the epidermis, specialized cells and structures provide pigmentation, immunity, and sensation. The epidermis itself is divided into five sublayers:
- Basal Cell Layer: Also known as the stratum germinativum, this innermost layer of the epidermis is responsible for constant cell regeneration. Basal cells divide continuously, pushing older cells toward the surface, where they are eventually shed. This layer contains melanocytes, which produce melanin to protect deeper skin layers from UV damage, as well as Merkel cells, which are tactile cells involved in sensory functions.
- Squamous Cell Layer: Located above the basal layer, this layer, or stratum spinosum, is the thickest part of the epidermis. Cells from the basal layer mature here into keratinocytes, which produce keratin, a protein that provides strength to the skin, hair, and nails. Langerhans cells are also present here, identifying and responding to pathogens that invade the skin.
- Stratum Granulosum and Stratum Lucidum: These are two thin layers through which keratinocytes pass as they move towards the skin surface. Here, cells become larger, flatter, and eventually die, forming a tough, cohesive layer as they bind together, which enhances the skin’s durability.
- Stratum Corneum: This outermost layer, known as the horny layer, is made of dead keratinocytes. It provides a resilient barrier and is constantly renewed by underlying cells. In young adults, this turnover occurs every 28-30 days, slowing to about 45-50 days with age.
- Dermis: Located below the epidermis, the dermis is the thickest skin layer, making up approximately 90% of skin’s thickness, ranging from 1.5 to 4 mm. It regulates temperature and supplies the epidermis with nutrient-rich blood. This layer also houses numerous specialized cells and structures:
- Blood Vessels: Blood vessels transport oxygen and nutrients to skin cells, remove waste, and distribute vitamin D produced in the skin to the body.
- Lymph Vessels: Lymph vessels circulate lymph, which contains immune cells that help defend the skin from infection.
- Hair Follicles: These sheath-like structures support and nourish hair growth, anchoring hair within the skin.
- Sweat Glands: There are two types of sweat glands in the dermis:
- Apocrine glands are found in the armpits and pubic region, secreting a milky sweat that promotes bacterial growth, leading to body odor.
- Eccrine glands are located throughout the body and regulate temperature by releasing sweat, which evaporates to cool the skin.
- Sebaceous Glands: These glands produce oil, or sebum, that helps to waterproof and protect the skin, keeping it supple and defending against bacterial growth.
- Nerve Endings: Pain and touch receptors in the dermis transmit sensory information, allowing the skin to detect temperature, pressure, and pain.
- Collagen and Elastin: The dermis is held together by collagen, produced by fibroblasts, providing skin with strength and resilience. Elastin allows the skin to stretch and return to its original shape.
- The dermis is divided into two sublayers:
- Papillary Layer: This upper layer contains thin collagen fibers and a vascular network that provides nutrients to the epidermis and aids in temperature regulation by controlling blood flow.
- Reticular Layer: Thicker and denser than the papillary layer, the reticular layer contains parallel collagen fibers that add strength and elasticity to the skin, supporting structures like hair follicles, sweat glands, and sebaceous glands.
- Subcutis (Hypodermis): The subcutis, also known as the hypodermis or subcutaneous layer, is the innermost skin layer and consists of fat and collagen cells. This layer serves as an insulator to conserve body heat and a shock absorber to protect internal organs. It also stores fat as an energy reserve and contains blood vessels, nerves, and lymph vessels that pass through to connect the skin with underlying tissues. The thickness of this layer varies by body part and individual.

Specialized Cells and Structures of the Skin
The skin contains an array of specialized cells and structures that play crucial roles in protection, sensation, and regulation. Each component contributes to the skin’s complex functions, from immune response to temperature control.
- Basket Cells: Located around the base of hair follicles, basket cells are pressure-sensitive. Their health and functionality are assessed when evaluating nerve integrity and response, as they are crucial for detecting tactile stimuli.
- Blood Vessels: Blood vessels in the skin deliver oxygen and nutrients essential for cellular health and carry away waste products. They provide the necessary support for skin layers to function effectively and are vital for healing and maintaining skin integrity.
- Arrector Pili Muscle (Hair Erector Muscle): This small muscle attaches to hair follicles and contracts in response to stimuli, such as cold or emotional stress, causing the hair to stand up and producing “goosebumps.” This reaction is part of the body’s attempt to regulate temperature and heighten sensitivity.
- Hair Follicle: Hair follicles are tube-like structures that anchor the hair and provide nourishment. Located in both the epidermis and dermis, they support hair growth and are essential for maintaining the health of hair as it emerges from the scalp or other skin surfaces.
- Hair Shaft: The hair shaft is the visible part of the hair above the skin surface. Composed of keratin, it protects the underlying skin and aids in regulating body temperature.
- Langerhans Cells: Found in the epidermis, Langerhans cells serve an immune function by identifying foreign antigens. When the skin is compromised, these cells attach to antigens, signaling the immune system to mount a response.
- Melanocytes: Located in the basal layer of the epidermis, melanocytes produce melanin, the pigment responsible for skin color. Melanin protects against ultraviolet (UV) damage, which makes melanocytes essential for skin health, especially in sun-exposed areas.
- Merkel Cells: These neuroectodermal tactile cells are situated in the basal epidermal layer. Merkel cells play a role in the sensation of light touch and contribute to the skin’s tactile acuity, helping detect fine details through mechanoreception.
- Pacinian Corpuscles: Located in the subcutaneous fatty tissue, Pacinian corpuscles are nerve receptors that respond to pressure and vibration. These specialized structures are critical for detecting changes in pressure, enhancing the body’s ability to respond to environmental stimuli.
- Sebaceous Glands: Positioned in the dermis, sebaceous glands secrete an oily substance onto hair follicles, providing a protective coating for the hair shaft. This oil, known as sebum, prevents hair from becoming brittle and also helps maintain the skin’s moisture barrier.
- Sensory Nerves: The epidermis is rich in sensory nerves that detect and transmit information about heat, pain, and other potentially harmful sensations. Malfunctioning sensory nerves can lead to sensations such as numbness, tingling, or burning. In skin biopsies, sensory nerve health is assessed by examining characteristics like branching, swelling, and overall integrity.
- Stratum Corneum: As the outermost layer of the epidermis, the stratum corneum is composed of dead cells that provide a tough barrier against environmental elements. It plays a significant role in protecting underlying tissues and is also used in diagnostic processes, as its thickness can indicate certain skin conditions.
- Sweat Glands (Sudoriferous Glands): Located in the epidermis, sweat glands produce moisture that is secreted through ducts onto the skin surface. Sweat evaporation is a key mechanism for thermoregulation, cooling the skin and maintaining optimal body temperature.
Nerves, Blood Supply, and Lymphatics of the Skin
The skin’s complex network of nerves, blood vessels, and lymphatic vessels supports its diverse functions, from sensation to temperature regulation. These components work together to maintain homeostasis, enabling the skin to interact with the external environment and respond to internal physiological needs.
- Blood Supply: Blood supply within the skin is organized into two main vascular plexuses that ensure efficient circulation and temperature control. One plexus lies between the papillary and reticular dermal layers, while the other is located between the dermis and subcutaneous tissue. The epidermis receives blood indirectly through the superficial arteriovenous plexus, or subepidermal/papillary plexus, which supports temperature regulation and nutrient distribution to the skin’s surface layers.
- Temperature Regulation through Blood Flow: Blood vessels within the skin play an essential role in regulating body temperature. When the body needs to dissipate heat, the autonomic nervous system triggers vasodilation, expanding blood vessels to increase blood flow near the skin’s surface, allowing heat to escape. Conversely, when the body needs to conserve heat, the sympathetic nervous system induces vasoconstriction, narrowing blood vessels to retain warmth. These adjustments are controlled by centers in the posterior hypothalamus, which respond to internal temperature changes to modulate blood vessel dilation or constriction.
- Nerve Supply: Skin contains an intricate network of nerves that includes both somatic and autonomic components. This nerve supply supports sensation and autonomic functions, such as sweating and hair movement.
- Somatic Sensory Nerves: Somatic nerves in the skin transmit sensory information to the central nervous system, including pain (nociception), temperature, touch (both light and discriminative), vibration, pressure, and proprioception. Specialized cutaneous receptors and end organs in the skin mediate these sensations, with each type of receptor responding to specific stimuli:
- Merkel Disks: Found in the stratum basale, these disks are sensitive to light touch, allowing the skin to detect fine details.
- Free Nerve Endings: Extending into the epidermis, these endings are critical for sensing pain, heat, and cold, and are particularly dense within the stratum granulosum and around hair follicles.
- Pacinian Corpuscles: Located in the deeper layers of the skin, these corpuscles respond to deep pressure and vibration, alerting the body to more intense stimuli.
- Meissner Corpuscles: Situated in the dermal papillae, these receptors are sensitive to low-frequency stimuli, enabling the skin to detect light touches and subtle movements.
- Ruffini Corpuscles: Found deeper in the skin, these corpuscles respond to sustained pressure, contributing to the sense of touch over broader areas.
- Autonomic Nerves: Autonomic innervation in the skin governs several essential functions, such as controlling vascular tone, stimulating hair root muscles (pilomotor function), and regulating sweat production. Through these mechanisms, the autonomic nervous system helps maintain thermoregulation and skin hydration while also contributing to emotional responses, like goosebumps.
- Somatic Sensory Nerves: Somatic nerves in the skin transmit sensory information to the central nervous system, including pain (nociception), temperature, touch (both light and discriminative), vibration, pressure, and proprioception. Specialized cutaneous receptors and end organs in the skin mediate these sensations, with each type of receptor responding to specific stimuli:
- Lymphatic Vessels: Lymphatic vessels, located within the dermal layer, play a supportive role in maintaining skin health by draining excess interstitial fluid, filtering out waste products, and facilitating immune responses. The lymphatic system also aids in transporting immune cells to areas of infection or injury, reinforcing the skin’s role as a protective barrier against pathogens.
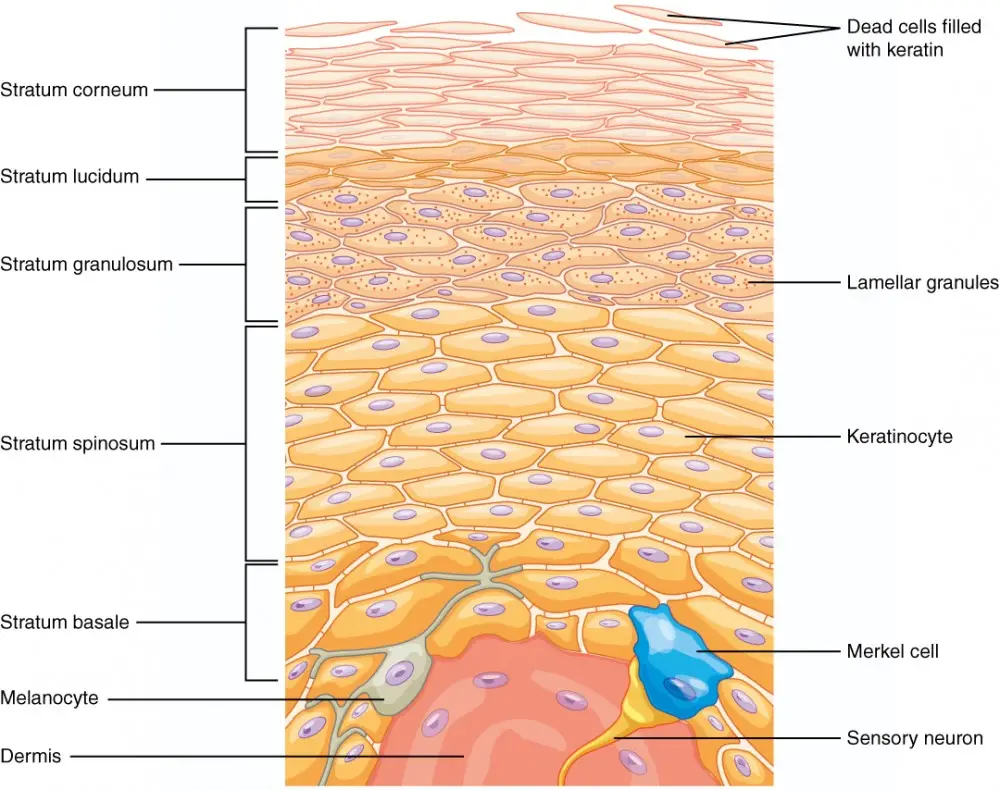
The Epidermis
The epidermis is the outermost layer of skin, providing a protective barrier against the environment. Composed of keratinized, stratified squamous epithelium, it consists of four to five distinct layers, depending on its location on the body. This structure allows for both durability and flexibility while keeping the body shielded from external elements. Below is a detailed look at the individual layers of the epidermis and their specific functions.
- Stratum Basale (Deepest Layer):
- The stratum basale, also called the stratum germinativum, is the deepest layer and attaches the epidermis to the basal lamina, which separates it from the dermis beneath.
- Cells in the stratum basale are bonded to the dermis by intertwining collagen fibers, creating a strong connection. Finger-like projections known as dermal papillae enhance this connection by increasing surface contact.
- This layer primarily consists of basal cells, cuboidal-shaped stem cells responsible for producing new keratinocytes through constant mitosis.
- Key cell types include Merkel cells, which respond to touch by stimulating sensory nerves, and melanocytes, which produce melanin, the pigment that protects cells from UV radiation and gives skin its color.
- Unique to each individual, fingerprints form in this layer as a result of the interaction between the stratum basale and the dermal papillae, creating the characteristic ridges used in personal identification.
- Stratum Spinosum (Spiny Layer):
- This layer, named for its spiny appearance, consists of 8-10 layers of keratinocytes that develop as cells divide in the stratum basale and move outward.
- The cells are interconnected by desmosomes, interlocking structures that provide strength and stability.
- The “spiny” appearance is a result of the staining process, which enhances the interlocked desmosomes.
- Langerhans cells are also present here, functioning as macrophages that ingest foreign particles and damaged cells, adding an immune defense component.
- Keratin synthesis begins in the stratum spinosum, with keratinocytes producing a water-repelling glycolipid, helping to prevent water loss and increase the skin’s resilience.
- Stratum Granulosum (Granular Layer):
- The stratum granulosum is three to five cell layers thick and appears grainy due to the accumulation of keratin and keratohyalin in the cells.
- As keratinocytes transition from the stratum spinosum to the stratum granulosum, they flatten, their cell membranes thicken, and they produce high amounts of keratin and keratohyalin, which contributes to the grainy texture.
- These cells undergo structural changes, including disintegration of nuclei and organelles, as they prepare to move to the outer layers.
- The layer’s lamellar granules contain lipids that are released to form a barrier, preventing water loss and helping to protect the body from environmental damage.
- Stratum Lucidum (Only in Thick Skin):
- This layer is found only in areas of thick skin, such as the palms, soles, and digits, appearing as a translucent layer between the stratum granulosum and the stratum corneum.
- Composed of dead and flattened keratinocytes, this layer’s transparency comes from eleiden, a lipid-rich protein derived from keratohyalin.
- The stratum lucidum serves as an additional water barrier and contributes to the thickness and toughness of skin in high-abrasion areas.
- Stratum Corneum (Outermost Layer):
- The stratum corneum is the outermost and thickest layer of the epidermis, made up of 15 to 30 layers of keratinized, dead cells.
- This layer is characterized by cells that are completely keratinized, a process also called cornification, which gives the skin its toughness and resistance to wear.
- These dead cells are continuously sloughed off and replaced by cells migrating from deeper layers, maintaining a barrier that protects against microbial invasion, prevents dehydration, and resists physical abrasion.
- This layer is replaced approximately every four weeks, and cosmetic procedures, like microdermabrasion, can assist in removing its outermost layers to promote skin renewal and maintain a healthier appearance.
Each layer of the epidermis has a distinct structure and function, working together to form a protective, resilient, and self-renewing barrier essential for skin health and overall bodily protection.
Clinical Significance of Skin
The skin’s clinical significance spans a wide range of medical conditions and diagnostic indicators, affecting virtually all medical disciplines. Below are key conditions related to the skin, each highlighting the importance of understanding skin pathology for diagnosis and treatment.
- Dermatomes: Dermatomes represent skin segments associated with spinal nerve roots, numbered according to spinal vertebral levels. Comprising 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal nerve, dermatomes are essential in assessing spinal injuries and certain infections. Conditions like shingles, caused by the varicella-zoster virus, show characteristic rashes and pain patterns aligned with dermatomes, aiding in precise localization of nerve involvement.
- Squamous Cell Carcinoma: Squamous cell carcinoma originates from keratinocytes, usually due to UV exposure, and is more prevalent in individuals with type I or II skin types—those with fair skin, blue or green eyes, and light hair, who burn easily without tanning. Characterized by thick, scaly, red patches that may bleed or appear wart-like, this carcinoma can metastasize and often develops from actinic keratoses, premalignant lesions formed by prolonged UV damage.
- Basal Cell Carcinoma: Originating from the basal layers of the epidermis, basal cell carcinoma typically appears as pearly papules on sun-exposed areas like the face. It is distinguished by telangiectasias and a tendency to ulcerate, though it rarely metastasizes compared to squamous cell carcinoma.
- Melanoma: A highly invasive cancer of melanocytes, melanoma has a high metastatic potential influenced by lesion depth. Although rarer than other skin cancers, melanoma is particularly aggressive and can manifest anywhere on the body. Lesions are often irregularly pigmented but can also present without pigmentation (amelanotic), posing diagnostic challenges.
- Langerhans Cell Histiocytosis: This rare cancer involves the accumulation of Langerhans cells, forming granulomas, often within bones, leading to pain. In the skin, it may present as rashes or blisters. Langerhans cell histiocytosis can also affect the pituitary gland, causing hormone deficiencies that lead to conditions such as diabetes insipidus. Complications like pancytopenia may arise if Langerhans cells crowd the bone marrow, resulting in symptoms such as anemia, thrombocytopenia, and leukocytopenia.
- Merkel Cell Carcinoma: A rare neuroendocrine carcinoma, Merkel cell carcinoma typically presents as a painless, solitary skin nodule, often less than 20 mm in size, with rapid growth over several months. Nodules can appear red, pink, violet, blue, or skin-colored and may ulcerate or form satellite lesions. This carcinoma is aggressive and often difficult to treat due to its rapid progression.
- Pemphigus Vulgaris: This autoimmune disease targets desmosomes, the cellular structures connecting keratinocytes, causing acantholysis and formation of fragile blisters within the epidermis. A key diagnostic feature is the positive Nikolsky sign, where the epidermis peels away when rubbed.
- Bullous Pemphigoid: Primarily affecting older adults, this autoimmune condition causes tense subepidermal blisters due to antibodies targeting hemidesmosomes at the dermal-epidermal junction. It is non-acantholytic and lacks a positive Nikolsky sign, differentiating it from pemphigus vulgaris.
- Scalded Skin Syndrome: Resulting from an exfoliative toxin produced by Staphylococcus aureus, this syndrome involves widespread skin exfoliation, fever, and an intensely red skin appearance. The condition also exhibits a positive Nikolsky sign, mimicking severe burn-like symptoms.
- Drug Reactions: Certain medications can lead to severe skin reactions such as erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis, and drug reaction with eosinophilia and systemic symptoms (DRESS). These reactions are commonly linked to sulfa drugs, NSAIDs, and antiepileptics, highlighting the importance of drug history in dermatologic assessments.
- Other Disorders of the Skin:
- Alopecia Areata: An autoimmune condition targeting hair follicles, leading to patches of hair loss.
- Vitiligo: Characterized by symmetrical depigmentation due to autoimmune destruction of melanocytes, with patches of lighter skin that are especially prominent in individuals with darker skin tones.
- Psoriasis: In psoriasis, keratinocyte mitosis in the stratum basale accelerates, thickening the stratum spinosum and creating “scaly” skin, typically appearing on the knees and elbows.
Functions of the Skin
Skin serves multiple essential functions that are critical to human survival and health. As the body’s largest organ, it provides protection, sensory input, temperature regulation, and more, utilizing its complex structure composed of the epidermis, dermis, and hypodermis.
- Protection from the Environment: The skin forms a primary barrier against external threats, such as mechanical injuries, pathogens, and harmful UV radiation. The outermost layer, stratum corneum, is composed of dead keratinocytes that shield against environmental dangers, while melanin, produced in the epidermis by melanocytes, further protects by absorbing UV light and preventing damage to underlying tissues.
- Water and Electrolyte Balance: A key function of the skin is to control water loss through a permeability barrier mainly formed by lipids in the stratum corneum. This lipid barrier retains moisture, reducing dehydration risk while allowing limited transdermal water absorption. Humans’ thicker skin also conserves water, a function that becomes crucial in dry environments.
- Sensation: The skin is a principal sensory organ, embedded with nerve receptors that detect touch, temperature changes, pressure, and pain. These signals are relayed to the brain, enabling appropriate responses to stimuli. Sensory capabilities are vital for detecting environmental hazards, as well as experiencing sensations like pleasure and discomfort.
- Temperature Regulation: Skin regulates body temperature through sweating and blood vessel adjustments. Sweat glands release perspiration, which cools the body as it evaporates from the skin’s surface. Additionally, blood vessels in the dermis constrict or dilate to either conserve heat or allow it to escape. This function is also visible in the phenomenon of “goosebumps,” where the skin’s arrector pili muscles contract, raising body hair and providing a minor insulating effect.
- Storage of Fats and Water: Skin tissues, particularly in the hypodermis, serve as storage for fat and water. Fat deposits provide insulation and serve as an energy reserve, especially critical in colder climates where animals often accumulate thick fat layers to stay warm. This stored fat also cushions and protects internal organs from physical impacts.
- Excretion of Scent Signals: Through sweat, the skin also excretes subtle chemical signals that communicate information to other organisms. In certain animals, glandular secretions in the skin allow them to mark territory, signaling information about identity, age, gender, and readiness for mating. Humans produce scents as well, which can subconsciously affect social interactions.
- Immune Defense: Skin contributes to immune defense through cells like Langerhans cells in the epidermis, which detect pathogens and stimulate immune responses. Additionally, the skin produces antimicrobial peptides that act as a defense mechanism against infection, ensuring a robust immune response.
- Vitamin D Synthesis: UV radiation exposure enables the skin to synthesize vitamin D, a nutrient essential for calcium absorption and bone health. This synthesis occurs in the deeper layers of the skin when exposed to sunlight, playing a crucial role in maintaining bone density and immune function.
- Aesthetic and Diagnostic Role: The skin’s appearance, including color, texture, and elasticity, often reflects overall health and can indicate underlying health issues. Changes in skin appearance, such as dryness, paleness, or discoloration, may signal medical conditions and are frequently assessed in medical examinations to help diagnose various health problems.
- Yousef H, Alhajj M, Fakoya AO, et al. Anatomy, Skin (Integument), Epidermis. [Updated 2024 Jun 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470464/
- Lopez-Ojeda W, Pandey A, Alhajj M, et al. Anatomy, Skin (Integument) [Updated 2022 Oct 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441980/
- https://teachmeanatomy.info/the-basics/ultrastructure/skin/
- https://byjus.com/biology/structure-and-functions-of-skin/
- https://training.seer.cancer.gov/melanoma/anatomy/
- https://en.wikipedia.org/wiki/Human_skin
- https://courses.lumenlearning.com/suny-ap1/chapter/layers-of-the-skin/