SARS-CoV is a type of coronavirus that caused a global outbreak of severe respiratory illness in 2002-2003. The virus was first identified in China and quickly spread to other countries, including Canada, where there was a significant outbreak.
The symptoms of SARS-CoV include fever, cough, and difficulty breathing. In severe cases, the illness can progress to pneumonia and acute respiratory distress syndrome (ARDS), which can be life-threatening.
SARS-CoV is spread through respiratory droplets when an infected person coughs or sneezes. The virus can also be transmitted by touching a surface contaminated with the virus and then touching the mouth, nose, or eyes.
To prevent the spread of SARS-CoV, it is important to practice good respiratory hygiene, such as covering your mouth and nose when coughing or sneezing, and washing your hands frequently. Quarantine measures and travel restrictions may also be implemented to prevent the spread of the virus.
While SARS-CoV is not currently a major public health concern, it remains a reminder of the potential for emerging infectious diseases to cause widespread illness and disruption.
Structure of Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV)
- SARS-CoV-2 possesses four major structural proteins, including spike (S) glycoprotein, small envelope (E) glycoprotein, membrane (M) glycoprotein, and nucleocapsid (N) protein, in addition to a number of ancillary proteins.
- The spike or S glycoprotein is a transmembrane protein with a molecular weight of approximately 150 kDa that is located in the virus’ outer membrane. S protein forms homotrimers protruding from the viral surface and facilitates the attachment of envelope viruses to host cells via attraction with angiotensin-converting enzyme 2 (ACE2) expressed in cells of the lower respiratory tract.
- This glycoprotein is cleaved into two subunits, S1 and S2, by the furin-like protease of the host cell. Part S1 is accountable for determining the host virus range and cellular tropism with the receptor binding domain structure, whereas S2 mediates virus fusion in transmitting host cells.
- The structural component of CoV localized in the endoplasmic reticulum-Golgi region and structurally bound to the nucleic acid material of the virus is the nucleocapsid known as N protein.
- The protein is involved in processes related to the viral genome, the viral replication cycle, and the cellular response of host cells to viral infections because it is bound to RNA. N protein is also highly phosphorylated, which may result in structural alterations that increase its affinity for viral RNA.
- The membrane or M protein, which is the most structurally structured protein and plays a role in determining the shape of the virus envelope, is another essential component of this virus.
- This protein is capable of binding to all structural proteins. Binding with M protein aids in the stabilization of nucleocapsids or N proteins and promotes viral assembly by stabilizing the N protein-RNA complex within the internal virion.
- The envelope or E protein, the smallest protein in the SARS-CoV structure, serves a role in the virus’s production and maturation.
- SARS-CoV2 binds to the ACE2 receptor, which is highly expressed in the lower respiratory tract, including type II alveolar cells (AT2) of the lungs, upper esophagus and stratified epithelial cells, and other cells including absorptive enterocytes from the ileum and colon, cholangiocytes, myocardial cells, kidney proximal tubular cells, and bladder urothelial cells.
- Patients infected with this virus experience not only respiratory problems such as pneumonia leading to Acute Respiratory Distress Syndrome (ARDS), but also cardiac, kidney, and digestive system disorders.

Genome of SARS-CoV
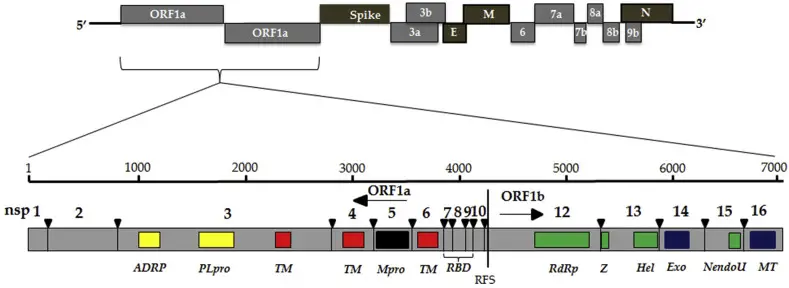
- The SARS Coronavirus genomes are 27 to 32 kb long, monopartite, single-stranded, positive-sense, polyadenylated, and capped RNAs.
- The replicase gene, which encodes multiple enzymatic activities, is located on a 20- to 22-kilobyte region of the 5′ end.
- The replicase gene products are encoded within two very large open reading frames, ORFs 1a and 1b, which are translated via a frameshifting mechanism into two large polypeptides, pp1a and pp1b.
- In the 3′ one-third of the genome, the structural proteins are encoded in the S-E-M-N order.
- Both the 5′ and 3′ extremities of the genome contain untranslated regions (UTRs), which are believed to interact with host and possibly viral proteins to regulate RNA replication, including the synthesis of positive- and negative-strand genomic-length RNA.
Replication of SARS-CoV

The coronavirus virion is composed of structural proteins, including the spike (S), envelope (E), membrane (M), nucleocapsid (N), and, for certain betacoronaviruses, haemagglutinin-esterase (not shown). N encapsulates the single-stranded, positive-sense RNA genome (+ssRNA), while M and E ensure its incorporation into the viral particle during the assembly process. S trimers protrude from the viral envelope derived from the host and confer specificity on cellular entry receptors.
- Coronavirus particles bind to cellular attachment factors, and specific S interactions with cellular receptors (such as angiotensin-converting enzyme 2), along with host factors (such as the cell surface serine protease TMPRSS2), promote viral uptake and fusion at the cellular or endosomal membrane.
- The immediate translation of two large open reading frames, ORF1a and ORF1b, occurs following the release and uncoating of inbound genomic RNA upon entry.
- The resulting polyproteins pp1a and pp1ab undergo co-translational and post-translational processing to generate the non-structural proteins (nsps) that comprise the viral replication and transcription complex.
- The biogenesis of viral replication organelles consisting of perinuclear double-membrane vesicles (DMVs), convoluted membranes (CMs), and small open double-membrane spherules (DMSs) creates a protective microenvironment for viral genomic RNA replication and transcription of subgenomic mRNAs (sg mRNAs) comprising the characteristic nested set of coronavirus mRNAs.
- Translated structural proteins translocate into endoplasmic reticulum (ER) membranes and transit through the ER-to-Golgi intermediate compartment (ERGIC), where interaction with N-encapsulated, newly synthesized genomic RNA causes branching into the lumen of secretory vesicular compartments.
- Virion production concludes with the exocytosis of infected cells. In red are highlighted the steps that are inhibited by compounds that are presently being validated and represent promising antiviral targets.
- An, 3′ polyA sequence; cap, 5′ cap structure; dsRNA, double-stranded RNA; L, leader sequence; RdRP, RNA-dependent RNA polymerase.
Pathogenesis of SARS-CoV
- Differentiated bronchial epithelial cells and alveolar epithelial cells of types 1 and 2 are the primary targets of SARS CoV infection in the lung.
- Acute respiratory distress syndrome (ARDS) is characterized histologically by the production of hyaline membranes inside the alveoli and extensive alveolar damage due to the desquamation of alveolar epithelial cells.
- Elevated levels of IL-6, IL-12, IL-8, CCL-2, and CXCL10 are found in the plasma of SARS patients.
- Lung pathology appears to progress through the second week of illness, despite the fact that viral load in the upper respiratory tract peaks between days 7 and 10 and then declines. This suggests that lung pathology continues to be driven by processes other than viral replication alone.
- The intestinal epithelium is also infected with SARS CoV, and virus is excreted in the stool.
- Direct infection of the digestive system may contribute to the diarrhea seen in SARS patients.
Epidemiology of SARS-CoV
- The SARS-CoV outbreak in 2002-2003 affected over 8,000 people in 29 countries, resulting in 774 deaths. The majority of cases occurred in China, Hong Kong, and Taiwan. The outbreak was declared over in July 2003, but sporadic cases continued to occur in some countries for several months afterward.
- The virus is believed to have originated in bats and then spread to civet cats, which were sold in Chinese markets as a delicacy. From there, the virus was transmitted to humans who came into contact with infected animals.
- SARS-CoV is primarily spread through respiratory droplets, which are released when an infected person coughs or sneezes. The virus can also be transmitted by touching a surface contaminated with the virus and then touching the mouth, nose, or eyes.
- One of the challenges in controlling the SARS-CoV outbreak was that the virus had a long incubation period of up to 10 days, during which an infected person could spread the virus without showing any symptoms.
- Public health measures, such as quarantine, isolation, and contact tracing, were effective in controlling the outbreak. However, the economic impact of the outbreak was significant, with travel and tourism severely affected in many countries.
- In conclusion, the SARS-CoV outbreak was a significant public health event that demonstrated the potential for emerging infectious diseases to cause widespread illness and disruption. The outbreak led to increased preparedness and surveillance efforts to prevent and control future outbreaks of similar viruses.
Clinical Manifestations of SARS
The estimated SARS incubation period ranges from 2 to 14 days. Symptoms include
- The symptoms of SARS (Severe Acute Respiratory Syndrome) typically start with a high fever (greater than 38°C/100.4°F), chills, headache, and muscle aches. These initial symptoms are often followed by a dry cough and shortness of breath. Some patients may also experience other symptoms such as fatigue, dizziness, and diarrhea.
- The fever associated with SARS is usually high and persistent, and may be accompanied by sweating and shivering. The cough associated with SARS is typically dry and non-productive, meaning that little or no phlegm is produced. Patients may also experience chest discomfort and difficulty breathing.
- In some cases, SARS can progress to pneumonia and acute respiratory distress syndrome (ARDS), which can be life-threatening. Patients with ARDS may require mechanical ventilation and intensive care support.
- It is important to note that the symptoms of SARS are similar to those of other respiratory illnesses, such as influenza and COVID-19. Therefore, it is important to seek medical care promptly if you develop symptoms of any respiratory illness, especially if you have been in
SARS manifested as a severe, progressive form of atypical pneumonia. SARS is characterized by elevated levels of multiple cytokines and chemokines in the peripheral circulation for approximately two weeks. Certain patients developed worsening tachypnea, oxygen desaturation, and respiratory distress syndrome. There is moderate hepatic dysfunction and significant lymphopenia present. Included among complications are liver failure and heart failure.
Lab Diagnosis of SARS-CoV
SARS-CoV is the virus responsible for Severe Acute Respiratory Syndrome (SARS). The laboratory diagnosis of SARS-CoV infection can be made using several methods:
- Nucleic Acid Amplification Tests (NAATs): These tests use Polymerase Chain Reaction (PCR) technology to detect viral RNA in respiratory specimens, such as throat swabs or sputum. NAATs have high sensitivity and specificity and are considered the gold standard for SARS-CoV diagnosis.
- Serological Tests: These tests detect antibodies against SARS-CoV in blood samples. However, serological tests are not useful for early diagnosis, as it takes time for antibodies to develop. They are more useful for identifying past infections and determining the prevalence of the virus in a population.
- Virus Isolation: This involves growing the virus in cell culture from respiratory specimens. Virus isolation is time-consuming and requires specialized facilities and expertise.
- Immunohistochemical Staining: This technique involves staining respiratory tissue samples with antibodies specific to SARS-CoV. This method is not commonly used for diagnosis, but can be useful in research settings.
Treatment of SARS
The treatment of Severe Acute Respiratory Syndrome (SARS) is primarily supportive care, as there is currently no specific antiviral therapy available for SARS. The treatment aims to relieve symptoms and prevent complications. The following are some of the treatments used in the management of SARS:
- Oxygen Therapy: Patients with severe respiratory distress may require oxygen therapy or mechanical ventilation to support breathing.
- Antipyretics: Medications such as acetaminophen can be used to lower fever and relieve discomfort.
- Corticosteroids: Corticosteroids such as prednisone may be used to reduce inflammation in the lungs. However, the use of corticosteroids is controversial, as they may delay the clearance of the virus and increase the risk of secondary infections.
- Immunomodulators: Drugs that modify the immune response, such as interferons, have been investigated for the treatment of SARS, but their effectiveness is unclear.
- Antibiotics: Antibiotics are not effective against viral infections, but they may be prescribed to prevent or treat secondary bacterial infections.
- Experimental Therapies: Various experimental therapies, such as convalescent plasma, monoclonal antibodies, and antiviral agents, have been studied for the treatment of SARS. However, their effectiveness is still uncertain, and they are not widely available.
- Supportive Care: Adequate hydration, nutrition, and rest are essential for the recovery of patients with SARS.
In summary, the treatment of SARS is primarily supportive care, with oxygen therapy, antipyretics, corticosteroids, immunomodulators, and antibiotics being used to manage symptoms and prevent complications. Experimental therapies are still under investigation and not widely available.v
Prevention and control of SARS
Prevention and control of Severe Acute Respiratory Syndrome (SARS) involves a combination of measures aimed at limiting the transmission of the virus and reducing the risk of infection. The following are some of the key strategies for the prevention and control of SARS:
- Infection Control Measures: Proper infection control measures, such as hand hygiene, use of personal protective equipment, and isolation of infected individuals, are critical to preventing the spread of SARS. Healthcare workers should follow strict infection control protocols when caring for patients with suspected or confirmed SARS.
- Travel Restrictions: Travel restrictions may be imposed to limit the spread of SARS. Travelers from areas with known SARS outbreaks may be screened for symptoms and isolated if necessary.
- Surveillance and Contact Tracing: Early detection and rapid response to SARS cases are critical to controlling outbreaks. Surveillance and contact tracing should be used to identify and isolate individuals who may have been exposed to the virus.
- Public Education: Public education campaigns can help raise awareness about SARS and promote prevention measures, such as hand hygiene, cough etiquette, and social distancing.
- Research and Development: Continued research and development of effective treatments and vaccines for SARS is critical to preventing future outbreaks.
FAQ
What is SARS-CoV?
SARS-CoV is a virus responsible for the outbreak of Severe Acute Respiratory Syndrome (SARS) in 2002-2003. It is a type of coronavirus that causes respiratory illness in humans.
How is SARS-CoV transmitted?
SARS-CoV is primarily transmitted through respiratory droplets from an infected person. It can also be spread through contact with contaminated surfaces.
What are the symptoms of SARS-CoV?
Symptoms of SARS-CoV include fever, cough, shortness of breath, and body aches. Some people may also experience diarrhea and respiratory distress.
How is SARS-CoV diagnosed?
SARS-CoV can be diagnosed through nucleic acid amplification tests (NAATs) that detect viral RNA in respiratory specimens or serological tests that detect antibodies against the virus in blood samples.
Is there a vaccine for SARS-CoV?
No, there is currently no approved vaccine for SARS-CoV.
How is SARS-CoV treated?
There is no specific antiviral treatment for SARS-CoV. Treatment is supportive care, which aims to relieve symptoms and prevent complications.
Can SARS-CoV be prevented?
Yes, SARS-CoV can be prevented through infection control measures, travel restrictions, surveillance and contact tracing, public education, and research and development.
Who is at risk of SARS-CoV?
Anyone can be infected with SARS-CoV, but those at higher risk include healthcare workers, close contacts of infected individuals, and people living in or traveling to areas with known outbreaks.
Can animals transmit SARS-CoV to humans?
Yes, SARS-CoV is believed to have originated from bats and was transmitted to humans through civet cats in the 2002-2003 outbreak. More recently, SARS-CoV-2 (the virus responsible for COVID-19) is believed to have originated from bats and was transmitted to humans through an intermediate animal (likely a pangolin).
Is there a risk of another SARS-CoV outbreak?
While there is no current outbreak of SARS-CoV, there is a risk of future outbreaks. Continued surveillance and research are needed to monitor and prevent the spread of the virus.
References
- Sharma A, Tiwari S, Deb MK, Marty JL. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2): a global pandemic and treatment strategies. Int J Antimicrob Agents. 2020 Aug;56(2):106054. doi: 10.1016/j.ijantimicag.2020.106054. Epub 2020 Jun 10. PMID: 32534188; PMCID: PMC7286265.
- Hodgens A, Gupta V. Severe Acute Respiratory Syndrome. [Updated 2022 Jul 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558977/
- Astuti I, Ysrafil. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): An overview of viral structure and host response. Diabetes Metab Syndr. 2020 Jul-Aug;14(4):407-412. doi: 10.1016/j.dsx.2020.04.020. Epub 2020 Apr 18. PMID: 32335367; PMCID: PMC7165108.
- Khan, Mujeeb & Syed, Farooq & Alkhathlan, Hamad & Tahir, Muhammad & Saif, Sadia & Khan, Merajuddin & Khan, Shams. (2020). COVID-19: A Global Challenge with Old History, Epidemiology and Progress So Far. Molecules. 26. 39. 10.3390/molecules26010039.
- Hu, B., Guo, H., Zhou, P. et al. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol 19, 141–154 (2021). https://doi.org/10.1038/s41579-020-00459-7
- V’kovski, P., Kratzel, A., Steiner, S. et al. Coronavirus biology and replication: implications for SARS-CoV-2. Nat Rev Microbiol 19, 155–170 (2021). https://doi.org/10.1038/s41579-020-00468-6
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.