Hemoglobin, often abbreviated as Hb, is a vital protein found in red blood cells (RBCs). Its primary role in the human body includes the transport of oxygen from the lungs to various tissues and the transfer of carbon dioxide from tissues back to the lungs. Additionally, hemoglobin plays a significant role in maintaining the pH balance of blood, contributing to the body’s overall homeostasis.
The structure of hemoglobin is complex and specialized. It is composed of four heme groups, each encased in a globin protein. This structure is critical for its function. The globin part of hemoglobin consists of two types of chains: alpha and non-alpha chains. In normal adult hemoglobin, there are variations in the non-alpha chains, leading to different forms of hemoglobin:
- Hemoglobin A (HbA): This is the most prevalent type in adults, accounting for about 96-98% of hemoglobin in the body. It is made up of two alpha and two beta globin chains.
- Hemoglobin A2 (HbA2): Making up about 1.5-3.5% of adult hemoglobin, this form consists of two alpha and two delta globin chains.
- Hemoglobin F (HbF): Present in less than 1% in adults, this type is primarily found in fetuses and newborns. It comprises two alpha and two gamma globin chains.
Hemoglobin’s ability to bind with various substances is central to its function. This binding can be normal, as in the case of oxyhemoglobin, where oxygen binds with hemoglobin. However, abnormal bindings can also occur, leading to different forms of hemoglobin:
- Carboxyhemoglobin: This form results when carbon monoxide binds with hemoglobin, which can be dangerous as it impedes oxygen transport.
- Carbaminohemoglobin: Here, carbon dioxide combines with hemoglobin, aiding in its transport from tissues to the lungs.
- Methemoglobin: This occurs when the iron in hemoglobin is oxidized from ferrous to ferric state, affecting oxygen transport.
- Sulfhemoglobin: In this rare form, sulfur binds with hemoglobin.
- Cyanmethemoglobin: This form involves the bonding of methemoglobin with cyanide ions.
Understanding hemoglobin and its various forms is crucial, as abnormalities in its structure or function can lead to a range of health issues, including different types of anemia and oxygen transport disorders. The study of hemoglobin is therefore important in both clinical and research settings, providing insights into many physiological and pathological processes.
Hemoglobin Estimation Methods
The estimation of hemoglobin levels is a fundamental procedure in medical diagnostics, offering insights into a patient’s oxygen-carrying capacity and overall blood health. Various methods have been developed for this purpose, each with its unique approach and degree of accuracy. Broadly, these methods can be categorized into visual, spectrophotometric, and other specific techniques.
- Visual Methods: These are traditional techniques that rely on the visual comparison of blood color to a standard. They include:
- Sahli’s Method: One of the oldest, it involves converting hemoglobin into a brownish compound, acid hematin, and comparing the color intensity with a standard scale.
- Dare Method: This method uses reflected light to compare the color of a blood sample against a standard.
- Haden Method: It is similar to the Sahli and Dare methods, focusing on color comparison.
- Wintrobe Method: Renowned for its use in determining red blood cell indices, this method also provides a way to estimate hemoglobin concentration.
- Tallqvist Method: Involves the use of a specially prepared paper chart to compare the color of blood.
- Spectrophotometric Methods: These are more precise methods that measure the absorption of light by hemoglobin at specific wavelengths.
- Oxyhemoglobin Method: This method measures the absorption of oxygenated hemoglobin.
- Cyanmethemoglobin Method: Widely used and considered a standard, this method involves converting hemoglobin into a stable compound, cyanmethemoglobin, which is then measured spectrophotometrically.
- Gasometric Method: A less common approach that measures the amount of oxygen hemoglobin can carry.
- Automated Hemoglobinometry: Modern laboratories use automated instruments that provide quick and accurate hemoglobin measurements, often through spectrophotometric methods.
- Other Methods: These include unique or less commonly used techniques such as:
- Alkaline-hematin Method: This method measures hemoglobin by converting it into alkaline hematin and assessing the absorbance.
- Specific Gravity Method: An older method that estimates hemoglobin based on the specific gravity of blood.
- Lovibond Comparator Method: Utilizes a comparator device for color matching and hemoglobin estimation.
Each of these methods has its advantages and limitations. Visual methods are simple and cost-effective but less accurate and more subjective. Spectrophotometric methods, particularly the cyanmethemoglobin method, offer greater precision and objectivity, making them the preferred choice in clinical settings. Automated systems further enhance accuracy and efficiency, making them ideal for high-volume testing. Understanding the various hemoglobin estimation methods is crucial for healthcare professionals in diagnosing and monitoring conditions like anemia and other blood disorders.
What is Sahli’s method for hemoglobin estimation?
- Sahli’s method, historically known as the acid hematin method, is a technique used for estimating hemoglobin levels in blood. This method falls under the category of visual comparator methods, which rely on the visual assessment of color intensity.
- The process involves converting hemoglobin in the blood sample into a form known as acid hematin. This conversion is achieved by treating the blood with an acid, which alters the hemoglobin’s color and opacity. Once this conversion takes place, the resulting color intensity of the acid hematin is compared visually to a standard color scale. The degree of similarity or difference in color between the sample and the standard is used to estimate the hemoglobin concentration in the blood sample.
- While Sahli’s method was widely used in the past due to its simplicity and the minimal requirement of laboratory equipment, it has some notable limitations. The primary issue is the reliance on visual comparison, which can lead to significant imprecision and inaccuracy. This subjectivity arises from individual differences in color perception and the quality of the color standards used for comparison.
- Due to these limitations, Sahli’s method is not commonly recommended in modern medical practices. Instead, spectrophotometric methods, such as the Cyanmethemoglobin method, are preferred. These methods offer greater precision and accuracy, as they rely on the measurement of light absorption rather than subjective visual comparison. Spectrophotometric techniques provide a more objective and reliable means of estimating hemoglobin levels, essential for diagnosing and monitoring various health conditions.
- In summary, while Sahli’s method played a significant role in the historical context of hemoglobin estimation, advancements in technology and a better understanding of the need for precision in medical diagnostics have led to the adoption of more accurate and reliable methods in contemporary medical practice.
Principle of Sahli’s Method
The principle of Sahli’s method, a traditional approach to hemoglobin estimation, is rooted in a chemical transformation process. This method relies on the principle that when blood is treated with a specific concentration of hydrochloric acid (HCl), a reaction occurs that leads to a noticeable color change, instrumental in estimating hemoglobin levels.
Upon the addition of dilute hydrochloric acid to the blood sample, the hemoglobin present in the red blood cells undergoes a chemical transformation. This reaction converts hemoglobin into a compound known as acid hematin, which has a distinct brown color. The intensity of this brown color is directly related to the concentration of hemoglobin in the blood.
Following this conversion, the acid hematin solution is methodically diluted. The objective of this dilution is to adjust the color intensity of the solution until it precisely matches a permanent standard. This standard is typically a brown glass, which serves as a reference for the desired color intensity. The comparison is made by direct visual observation, where the color of the diluted acid hematin solution is compared against the color of the standard brown glass.
The key to the Sahli’s method is the correlation between the amount of dilution required to match the standard and the original hemoglobin concentration in the blood. Essentially, the more the solution needs to be diluted to match the standard color, the higher the concentration of hemoglobin in the original sample.
It’s important to note that while the principle behind Sahli’s method is straightforward, the reliance on visual comparison for color matching introduces a degree of subjectivity. This can lead to variations in results due to differences in individual perception and lighting conditions. Consequently, although historically significant, Sahli’s method has largely been superseded by more objective and precise techniques in modern clinical practice, such as spectrophotometric methods. These advanced methods reduce subjectivity and provide more reliable and accurate measurements of hemoglobin levels.
Requirements for Sahli’s Method
For conducting the Sahli’s method of hemoglobin estimation, a specific set of requirements must be met to ensure accurate and reliable results. This method involves both a blood specimen and a range of instruments and reagents.
Specimen Requirements:
- Type of Blood: Sahli’s method can be performed using either capillary or venous blood. However, if venous blood is used, it must be anticoagulated to prevent clotting. This is typically achieved by adding 1.5 to 1.8 mg of EDTA (Ethylenediaminetetraacetic acid) per milliliter of blood, and the mixture should be thoroughly combined immediately after collection.
Instrument Requirements:
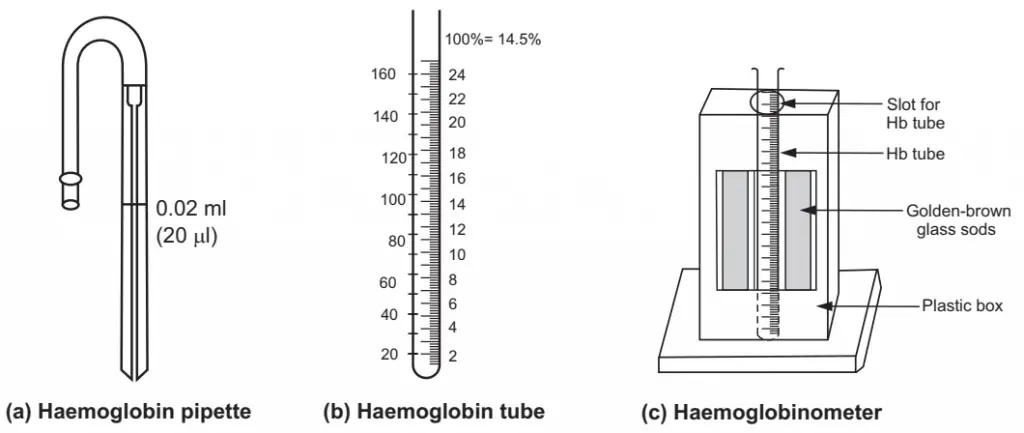
- Sahli’s Hemoglobinometer: This is a specialized set that includes several components:
- Comparator: This is a rectangular plastic box featuring a central slot to accommodate a hemoglobin tube. On either side of this slot, brown standard glasses are placed for color matching. At the back, there’s a white opaque glass to ensure uniform illumination during the comparison process.
- Hemoglobin Tube (Sahli-Adams Tube): This tube is marked with graduations. On one side, it is graded in gram percentage (g%) ranging from 2 to 24, and on the other side, it is marked in percentage (%) from 20 to 140.
- Sahli’s Pipette (Hemoglobin Pipette): This pipette, marked only at 20μl (0.02ml), is used for measuring the blood sample. Unlike pipettes used for white blood cell (WBC) and red blood cell (RBC) counts, it does not have a bulb.
- Stirrer: A thin glass rod, this is used to stir the mixture inside the hemoglobin tube.
Reagent Requirements:
- N/10 Hydrochloric Acid (HCl): This reagent is critical for the chemical conversion of hemoglobin into acid hematin. To prepare N/10 HCl, one can dissolve 36 grams of HCl in distilled water to make up 1 liter, which constitutes 1 N HCl. This solution is then diluted 10 times to achieve the required N/10 concentration.
- Distilled Water: Used for diluting the acid hematin solution during the process to match the color intensity with the standard.
Step-by-Step Procedure of Sahli’s Method
- Preparation:
- Begin by confirming that the hemoglobinometer tubes and Sahli’s pipette are clean and dry. Any residue or moisture can interfere with the accuracy of the test.
- Adding Hydrochloric Acid:
- Fill the hemoglobinometer tube with N/10 Hydrochloric Acid (HCl) up to its lowest graduation mark. This mark is typically labeled as 2 g% or 10%. Use a dropper for precise measurement and to avoid spillage.
- Collecting and Adding the Blood Sample:
- Draw blood into the Sahli’s pipette until the 20 μl mark. Carefully wipe off any excess blood from the outside of the pipette. This step is crucial to ensure the accuracy of the volume of the blood sample.
- Gently deliver the blood from the pipette into the N/10 HCl in the hemoglobin tube. This combination initiates the chemical reaction needed for the test.
- Chemical Reaction Time:
- Mix the blood and HCl solution thoroughly using the stirrer.
- Leave the mixture undisturbed for about 10 minutes. This waiting period allows for complete conversion of hemoglobin into acid hematin, which is necessary for accurate estimation.
- Color Matching:
- Gradually add distilled water to the tube, drop by drop, stirring continuously. The aim is to dilute the solution until its color matches precisely with the standard brown glass in the comparator. This step requires careful observation and gradual adjustment.
- Reading the Result:
- Once the color of the solution in the hemoglobinometer tube matches the standard, take the reading at the lower meniscus of the liquid in the tube.
- The reading directly indicates the hemoglobin concentration in grams per 100 ml of blood. This is read off the graduated scale on the tube.
Advantages of Sahli’s method
- Ease of Performance and Convenience:
- One of the most significant advantages of Sahli’s method is its simplicity. It does not require extensive training or sophisticated skills, making it accessible to a wide range of healthcare providers, including those in low-resource settings.
- Time Efficiency:
- The procedure can be completed relatively quickly. The total time from the collection of the blood sample to the final reading usually does not exceed 15 minutes. This rapid turnaround is beneficial in situations where quick results are necessary.
- Affordability of Equipment and Reagents:
- The apparatus required for Sahli’s method, such as the hemoglobinometer tube and Sahli’s pipette, along with the reagents like N/10 Hydrochloric Acid, are relatively inexpensive. This cost-effectiveness is particularly advantageous in settings with limited funding for medical equipment.
- Availability and Safety of Reagents:
- The reagents used in Sahli’s method are easily obtainable and pose less harm in terms of chemical safety compared to some reagents used in other hemoglobin estimation methods. This aspect makes it a safer choice in less controlled environments.
- Suitability for Mass Surveys:
- Given its simplicity, minimal equipment requirements, and the fact that it doesn’t rely on electricity, Sahli’s method is particularly well-suited for mass surveys and fieldwork, especially in remote areas where access to electricity and advanced laboratory facilities is limited.
Disadvantages of Sahli’s method
- Nature of Acid Hematin:
- In Sahli’s method, hemoglobin is converted into acid hematin, which is a suspension rather than a true solution. This can lead to turbidity or cloudiness in the sample, potentially affecting the accuracy of the visual comparison and the final results.
- Limited Scope of Hemoglobin Estimation:
- The method primarily estimates oxyhemoglobin and reduced hemoglobins. However, it does not effectively measure other forms of hemoglobin, such as carboxyhemoglobin, methemoglobin, and sulfhemoglobin, which can constitute approximately 2-12% of total hemoglobin. This limitation means that the method might not provide a complete picture of the hemoglobin profile.
- Ineffectiveness for Fetal Hemoglobin (HbF):
- Sahli’s method is not suitable for measuring hemoglobin in infants up to 3 months old because HbF (fetal hemoglobin) does not convert to acid hematin. This limits the method’s applicability in neonatal and pediatric settings.
- Influence of High White Blood Cell (WBC) Counts:
- In cases where the WBC count is extremely high (over 100,000/cumm), the resulting solution of acid hematin can become turbid. This turbidity can falsely elevate the estimated hemoglobin levels by 5-10%.
- High Risk of Visual Errors:
- The method relies heavily on the visual comparison of colors, which introduces a significant subjective element. The accuracy of this comparison can be influenced by the observer’s perception, ambient lighting, and even the gradual fading of the acid hematin’s color over time.
- Fading of Glass Standards:
- The brown glass standards used for color comparison may fade with time, leading to inaccurate calibrations and, consequently, erroneous hemoglobin estimations.