Radiation is used to sterilize and decontaminate medical supplies (surgeon supplies, vaccines and drugs) as well as the food and beverage industries. There are two types of radiations available: ionizing or non-ionizing.
Radiation sterilization isn’t widely used in the food industry because of concerns about radioactive contamination, toxic or carcinogenic products production, taste alteration, and change in nutritional value.
What is Radiation Sterilization?
Radiation sterilization has been available since the 1950s. It has seen a tremendous increase in popularity over the past 60 years. Radiation sterilization uses ionizing radiation (primarily gamma or X-ray radiation) to kill microorganisms like bacteria, viruses, fungi and spores. This method has many advantages over chemical- or heat-based sterilization methods. It is especially attractive for healthcare and medicine. Radiation sterilization can be used for example during tissue allograft preparation and pharmaceutical packaging.
Process and Dosage of Radiation Sterilization
Radiation can cause genetic damage and chemical modifications in biological macromolecules that can lead to death in biological organisms. Sterilization treatment involves bombarding the sample with high-energy electrons or electromagnetic radiation. This causes the formation of highly unstable free radicals, molecular and secondary electrons, as well as molecular ions, and other ionizing radiation. These radiation products react with nearby molecules to alter and fracture chemical bonds. Particularly DNA is sensitive to radiation damage and can be damaged by ionizing radiation. The failure to repair DNA damage will eventually lead to cell death and loss of genetic information. Radiation can be used to sterilize cells and kill microorganisms.
The decimal reduction dose (D10) is the radiation dose that results in a 10-fold decrease in the population of microorganisms. This indicates the biological organism’s sensitivity to radiation. To be effective sterilization must take into account the D10 values of microorganisms, the initial level and diversity of bioburden. The optimal radiation dose is determined by the desired sterilization assurance level (SAL), which determines the likelihood that a microorganism can survive the sterilization process. A minimum SAL of 10-6 is desirable. A standard dose of 25 kGy would be sufficient to treat a product contaminated by Vibrio cholerae or Salmonella typhimurim (D10=0.3 kGy), but a dose of the same amount applied to a sample contaminated by HIV (D10=4.0 – 8.4kGy) would produce a SAL of only 10-3 to 10-6. Radiation dosage must be adjusted to the specific properties of the sample and the degree of sterility.
Ionizing radiations
Ionizing radiation is an excellent agent for sterilization/disinfection, it kills organisms without increasing the temperature; so aptly called cold sterilization. It kills both prokaryotic and eukaryotic bacterial endospores and vegetative cells. However, it is not always effective against viruses.
Mechanism of Sterilization by Ionizing Radiations
Ionizing radiation collides particles with electrons (e) and other reactive molecules like hydroxyl radicals, hydride radicals, and *OH. Each of these reactive molecules can alter or degrade biopolymers like DNA and protein. The death of irradiated cell can be caused by the destruction of DNA or enzymes.
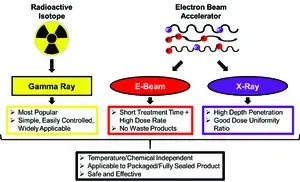
There are many sources of ionizing radiation available. These include X-ray machines (eletron-beam radiation), cathode-ray tubes (eletron-beam radiation) and radioactive nuclides.
X-Rays
X-rays can be fatal to microorganisms, higher life forms, and are not used for sterilization. Their production is costly and their efficient utilization difficult. Radiations are scattered in all directions away from the origin.
Gamma Rays
Gamma radiations, which are high-energy radiations that are emitted by certain radioisotopes like Caesium137 (137Cs), and Cobalt-60 (660Co), are both low-cost bioproducts from nuclear fission. Gamma rays have a similar wavelength to x-rays, but they are shorter in energy and of a higher energy. They can penetrate deep into matter and are deadly to all living things, even microorganisms. Gamma radiations can be used to sterilize materials with a large thickness or volume.
Cathode Rays (Electron-Beam Radiation)
With a short exposure, cathode radiations or electron beams can sterilize at room temperature. They are useful for sterilizing surgical supplies, drugs, or other materials.
Application of Ionizing Radiations
Gamma radiation is the most common method for radiation sterilization. The sterilization of is done using gamma radiation
- Disposables like infusion sets, plastic syringes and catheters.
- Bone, tissue, grafts and antibiotics.
- Radiation of food (permitted by some countries).
Advantages of Ionizing Radiations
- High penetration power: Products can be sealed in their final packaging to reduce the chance of contamination after sterilization.
- Rapidity of action: Saves time and effort
- Temperature is not raised: compatible with temperature-sensitive materials, such as pharmaceuticals and biological samples.
- Flexibility: Products can be sterilized in any phase (liquid, gaseous, or solid), density, size or thickness.
Disadvantages of Ionizing Radiations
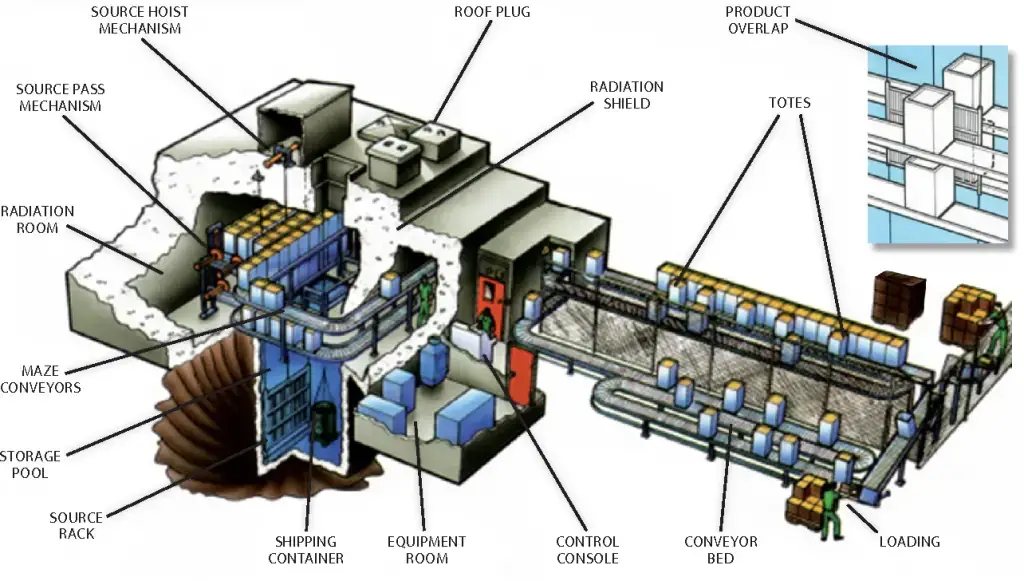
- High capital costs mean that specialized facilities, such as gamma irradiation units, are often required. for gamma irradiation
- Gamma radiation can only be used if radioactive material is handled and disposed of.
- Some materials may not be compatible. This can lead to product and packaging material breakdown. For example, Common plastics such as polyvinyl chloride (PVC), acetal, and polytetrafluoroethylene (PTFE) are sensitive to gamma radiation.
Sterilization/disinfection control: Efficacy of ionzing radiation is tested by using Bacillus pumilus.
Non-ionizing Radiation
Non-ionizing radiations can be quite deadly but they do not penetrate glass, dirt or films. They are therefore restricted to disinfection of clean surfaces in operation theatres, laminar flowhoods and water treatment. For 30 minutes, the recommended dose is between 250-300 nm wavelength.
Infra-Red Radiation
Infra red rays are low-energy electromagnetic rays that have wavelengths longer than visible light. They cause the oxidation of molecules to kill microorganisms. For rapid sterilization of catheters and syringes, infra-red radiation is used.
Ultraviolet Light (UV) Sterilization
While sunlight may be partly made up of UV light, the ozone layer filters out shorter wavelengths of sunlight. There are three types UV radiation: UVA, UVB and UVC. They are classified according to the wavelength they emit. The most harmful type of UV radiation is short-wavelength UVC.
Mechanisms of UV Sterilization
Many cell materials, including nucleic acids, absorb ultraviolet light. It results in the formation of pyrimidine dimers, which inhibits DNA replication. This can cause mutation and death in exposed organisms.
Uses of UV Sterilization
For disinfecting surfaces, water, and air that are not susceptible to UV rays, UV lights can be used. Some UV lights are capable of killing the flu virus (influenza). Ultraviolet radiation can be used to disinfect enclosed areas like nurseries, bacterial laboratories, inoculation booths, laminar flow and operation theatres. To disinfect the surface of laboratory biological cabinets, a UV light is provided to “germicidal”, which can be used after each use.
The UV sterilization process is ongoing. However, it is important to close the area and turn off UV lamps immediately after using.
Effects of UV light in SARS-CoV-2 (COVID-19)
UV radiation is used to kill viruses by chemically altering their genetic material, DNA and RNA. The UVC spectrum is the most effective for inactivation. Its wavelength of 260 nm is the most powerful. Although we don’t know much about the effects of UVC on SARS-CoV-2 (CoV-2), concentrated UVC is a key weapon in the fight against COVID-19. UVC light can be used to sterilize buses and UVC-emitting robotics to sterilize hospitals floors. Banks also use UV light to disinfect their money.
Disadvantages of Non-ionizing Radiation
- Eyes and skin damage: UV light from the sun can damage and penetrate skin, and cause cataracts.
- It does not penetrate paper, glass, or cloth.
Advantages of Radiation Sterilization
Radiation-based sterilization offers many advantages over heat-based or chemical sterilization.
- Terminal Processing: Products can be processed in fully sealed final packaging due to the penetration depth of the ionizing radiation. This reduces the risk of contamination after sterilization.
- Cold Method/Temperature Independence: Treatments are performed at a low temperature. Radiation sterilization is heat-independent and works at both ambient and sub-zero temperatures. It can be used with temperature sensitive materials such as pharmaceuticals or biological samples.
- Chemical Independence: There are no volatile or toxic chemicals required. No disposal is required for X-ray and e-beam radiation.
- No residue: Radiation does not leave any residues on sterilized products
- Flexibility: Products can be sterilized by radiation in any phase (liquid, gaseous, or solid), as well as products with variable size, density, thickness, or homogeneous systems. Sterilization can also be done at any temperature or pressure.
- Time efficiency: E beam sterilization can be done in seconds to minutes.
- Sterility assurance level (SAL): Radiation treatment can produce a high level of sterilization assurance (SAL) of 10-6 or higher, which means that only a fraction of one million microorganisms will survive the sterilization procedure.
- Ease: Radiation sterilization is simple and straightforward because only one variable must be monitored, the exposure time/dose.
Disadvantages of Radiation Sterilization
Radiation sterilization techniques have their drawbacks.
- Instrumentation: High capital costs and the need for specialized facilities make it difficult to obtain instruments. A nuclear reactor is required to generate gamma radiation. E-beam and X-ray radiation can be generated by electron beam accelerators.
- Product Degradation: Radiation-based methods can cause product degradation. Common plastics such as polyvinyl chloride (PVC), acetal and polytetrafluoroethylene (PTFE) are sensitive to gamma radiation. High energies in e beam radiation can cause main chain scission (breaking the long-chain backbone) or chemical crosslinking.
- Radioactive material: Radiation sterilization is required when gamma radiation serves as an ionization source. At the most common radiation levels, radioactivity is not inflicted on treated samples by gamma radiation.
Radiation Sterilization Market
In 2016, the global sterilization market had a value of $4.69 billion. It is expected to rise to $6.93 trillion by 2021. While gamma sterilization is the most common form of radiation-based sterilization (and the most popular), e-beam- and X-ray based technologies have become more popular. There are approximately 40.5% of sterilization methods that use gamma, 4.5% e beam sterilization, and 50% ethylene oxide sterilization (a method for sterilizing by using gaseous substances).
Over 200 gamma radiation facilities were found in 50 countries in 2017. To sterilize 400,000,000 cubic feet of product, these facilities use approximately 400 million curies each year of Co-60. The number of electron beam sterilization facilities was somewhat lower than the 75 worldwide. The development of high-powered electron accelerators has accelerated X-ray sterilization’s growth. In 2010, the first commercial facilities for Xray sterilization of medical devices were opened. By 2017, there were only five.
Applications to Medical Devices and Products
Radiation sterilizes approximately 40-50% of disposable medical products at the moment. Gamma radiation is used to sterilize sutures, surgical gloves and gowns, as well as stick plasters, dressings, and other single-use healthcare supplies. Radiation sterilization is a popular option for these products because it can be applied directly to the item in sealed packaging. This reduces the risk of recontamination and eliminates post-sterilization packaging steps.
Consider the compatibility between radiation and medical device components. Although many materials (such as metals) are not affected by radiation sterilization, polymers can experience chemical reactions that cause changes in their physical properties. Gamma sterilization can be minimized by using less radiation-sensitive materials and including polymer stabilizers within packaging and other device materials.
International Organization for Standardization (ISO) has established standards for medical products that can be radiation sterilized. The ISO published the first edition ISO-11137 in 1995. It outlines validation methods, quality control and requirements for sterilization activities. The United States was a major contributor to the development of the document. They participated in the Association for Advancement of Medical Instrumentation. The US adopted the final name ANSI/AAMI/ISO 11137. It consists of three parts. “Part 1: Requirements to develop, validate and routinely control a sterilization procedure for medical devices”, Part 2: Establishing sterilization dose” and “Part 3 : Guidance regarding dosimetric factors”. ISO 11137 has been updated and amended multiple times in order to include the most recent standards.
Applications to Biological Tissues
Gamma radiation is used to sterilize connective tissue allografts such as skin, cartilage and bone. The recipient’s risk of contracting disease is a major concern with tissue allografts. Potentially dangerous microorganisms could be from donors or have been introduced to tissue during processing, storage, and transfer. Tissue samples should be sterilized prior to being introduced into the recipient. This will reduce the risk of infection by fungal, bacterial or viral diseases.
Gamma radiation can be used to reduce the number of viruses and microbials in the body. It is often not associated with any significant changes in tissue properties. Radiation can cause some chemical and physical changes to the graft. To ensure that the radiation dose is high enough to kill microbes, but not too much to damage the properties of the allograft, a compromise must be reached. Long considered the gold standard in tissue treatment, 25 kGy radiation has been proven to be sufficient to kill many bacteria, viruses, and RNA.
Tissue banks may alter their dose from the reference 25kGy to use doses between 15 and 35kGy to match the bioburden and achieve the desired SAL. This helps maintain tissue integrity and tissue integrity. To help tissue banks decide the best radiation dose, the ISO provides guidance for dose validation. Current research is underway to determine how radiation treatment affects the biological quality and clinical efficacy the allograft.
References
- Madigan Michael T, Bender, Kelly S, Buckley, Daniel H, Sattley, W. Matthew, & Stahl, David A. (2018). Brock Biology of Microorganisms (15th Edition). Pearson.
- Lytle, C. D., & Sagripanti, J.-L. (2005). Predicted Inactivation of Viruses of Relevance to Biodefense by Solar Radiation. Journal of Virology, 79(22), 14244.
- Tille, P. (2017). Bailey & Scott’s Diagnostic Microbiology (14 edition). Mosby.
- Willey, Joanne M, Sherwood, Linda M, & Woolverton, Christopher J. (2016). Prescott’s Microbiology (10 edition). McGraw-Hill Education.
- Radiation Sterilization. Stanford University. Retrieved April 24, 2020, f. http://large.stanford.edu/courses/2018/ph241/goronzy2/
- https://microbeonline.com/radiation-sterilization-types-mechanism-applications/
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.