What is Puberty?
- Puberty is a natural process during which a child’s body undergoes significant physical changes, transforming into an adult body capable of sexual reproduction. It is triggered by hormonal signals from the brain to the gonads, which are the ovaries in girls and the testes in boys. In response to these signals, the gonads produce hormones that stimulate various aspects of development, including the growth, function, and transformation of the brain, bones, muscles, blood, skin, hair, breasts, and sex organs.
- During the first half of puberty, there is a noticeable acceleration in physical growth, including height and weight. This growth continues until the body has fully developed into that of an adult. Before puberty, the external sex organs, known as primary sexual characteristics, already differ between boys and girls. However, during puberty, secondary sex characteristics develop, further distinguishing the sexes. These secondary sex characteristics include features like the growth of facial and body hair in boys, deepening of the voice, and the development of breasts and wider hips in girls.
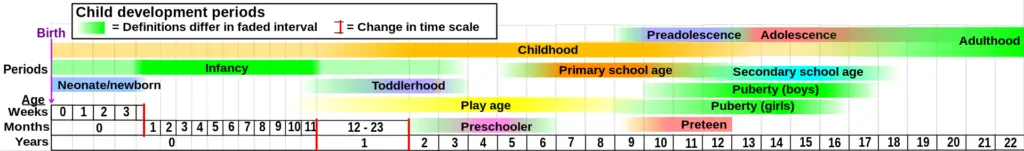
- The onset and duration of puberty can vary, but on average, girls begin puberty around the ages of 10 to 11 and complete it between the ages of 15 and 17. Boys, on the other hand, generally begin puberty between the ages of 11 and 12 and complete it between the ages of 16 and 17. In females, a significant milestone of puberty is menarche, the onset of menstruation, which typically occurs around the ages of 12 to 13. For males, the first ejaculation, known as spermarche, typically occurs around the age of 13.
- Comparing the average ages of puberty milestones today with those of the 19th century, it is evident that children, particularly girls, are reaching these milestones at younger ages. This can be attributed to factors such as improved nutrition, which leads to rapid body growth and increased weight and fat deposition. Additionally, exposure to endocrine disruptors like xenoestrogens found in certain foods or environmental factors can also influence the timing of puberty. However, recent archaeological research suggests that the current rate of puberty is actually the intended norm. While growth spurts may have started at around 10 to 12 years old, factors like severe environmental conditions, poverty, poor nutrition, and pollution could have caused delays in the later stages of puberty, such as menarche.
- In some cases, puberty may begin earlier than usual, which is referred to as precocious puberty, while in other cases, it may start later than usual, known as delayed puberty. These variations can occur due to various factors, including genetics, hormonal imbalances, or underlying medical conditions.
- It is important to note that while puberty primarily refers to the physical changes associated with sexual maturation, the term “adolescent development” encompasses the psychosocial and cultural aspects of transitioning from childhood to adulthood in Western culture. While puberty and adolescence overlap in terms of the body’s development, they represent distinct aspects of an individual’s growth and maturation.
Definition of Puberty
Puberty is the natural process of physical changes during which a child’s body develops into an adult body capable of sexual reproduction.
Effects of early and late puberty onset
The effects of early and late puberty onset can have significant implications for both girls and boys. Here’s a breakdown of the effects based on the provided information:
Girls:
- Early Onset: Girls who experience early puberty often face psychological challenges. The development of secondary sexual characteristics and weight gain can make them appear larger than their peers who have not yet entered puberty. This can lead to negative body image, lower self-esteem, and increased depression. Early-maturing girls may feel the need to hide their breasts and may experience embarrassment or discomfort, which can affect their participation in activities like undressing for gym class. Early-maturing girls may also develop relationships with older individuals, which can expose them to risky behaviors such as alcohol and drug use, unprotected sexual relations, eating disorders, and bullying.
- Late Onset: Girls who experience later puberty tend to have more positive outcomes. They exhibit positive behaviors in adolescence that carry over into adulthood. The delayed physical and emotional development allows them to align better with their same-age peers, leading to improved self-esteem and positive body image.
Boys:
- Early Onset: While early puberty in boys was traditionally associated with positive outcomes such as leadership and success in adulthood, recent studies suggest that the risks and problems of early maturation may outweigh the benefits. Early-maturing boys may exhibit more aggressive, law-breaking, and alcohol-abusing behaviors, leading to conflicts with parents, trouble in school, and potential legal issues. Early puberty is also linked to increased sexual activity and a higher incidence of teenage pregnancy, which can contribute to psychosocial problems such as depression. However, early-maturing boys may also experience positive outcomes, such as popularity among peers, higher self-esteem, and improved confidence, due to physical developments like height, muscular physique, and athletic abilities.
- Late Onset: Boys who experience late puberty often face challenges in terms of self-esteem, confidence, and popularity among peers. Their less-developed physiques can make them feel inferior and contribute to feelings of anxiety and depression. Late-maturing boys may also exhibit a greater fear of sex compared to their peers.
It’s important to note that these generalizations are based on the provided information, and individual experiences may vary. Puberty is a complex and individualized process, and the effects of early or late onset can differ for each person.
Certainly! Here’s the information presented in a table format:
| Aspect | Early Onset of Puberty in Girls | Late Onset of Puberty in Girls | Early Onset of Puberty in Boys | Late Onset of Puberty in Boys |
|---|---|---|---|---|
| Psychological Effects | – Negative body image | – Positive behaviors in adolescence and adulthood | – Aggressive, law-breaking, and alcohol-abusing behaviors | – Lower self-esteem and confidence |
| – Lower self-esteem | – Increased sexual activity and higher teenage pregnancy rate | – Lower popularity among peers | ||
| – More depression | – Potential conflicts with parents, trouble in school, and legal issues | – Problems with anxiety and depression | ||
| – Poorer body image | – Potential positive outcomes like popularity, higher self-esteem, and confidence | – Greater fear of sex compared to peers | ||
| Social Relationships | – Relationships with older individuals | |||
| – Risk of alcohol and drug use, increased sexual relations, eating disorders, and bullying | ||||
Changes in males
Testicular size
Testicular size is a significant aspect of male puberty and undergoes specific changes. Here’s an overview of testicular size based on the provided information:
- Testicular Enlargement: In boys, the first visible sign of puberty is the enlargement of the testicles, also known as gonadarche. Prior to puberty, the size of the testes remains relatively constant, averaging about 2-3 cm in length and 1.5-2 cm in width from around 1 year of age.
- Tanner Scale: The size of the testicles is measured and classified according to the Tanner scale, which assesses the development of male genitals. Stage I represents testicular volume less than 1.5 ml, while stage V indicates a testicular volume equal to or greater than 20 ml. This scale helps track the progression of testicular growth throughout puberty.
- Adult Testicular Size: Testicular size continues to increase after the onset of puberty, reaching its maximum adult size approximately six years later. On average, the adult testicular size is around 18-20 cm3, but it’s important to note that there can be considerable variation in testicular size within the normal population.
- Penis Development: As the boy’s testicles enlarge and develop for about a year, other changes occur in the penis. The length of the shaft and the breadth of the penis increase, and the glans penis (the head) and corpora cavernosa (erectile tissues) also start to enlarge, gradually reaching adult proportions.
These changes in testicular size and penis development are driven by hormonal fluctuations, particularly the release of testosterone during puberty. It’s important to remember that individual variations exist, and the timing and pace of these changes may differ among individuals.
Male musculature and body shape
During puberty, significant changes occur in male musculature and body shape. Here’s an overview based on the provided information:
- Increased Muscle Mass: By the end of puberty, adult men have significantly more skeletal muscle compared to women. On average, adult men possess nearly twice as much skeletal muscle as adult females. The increase in muscle mass is a result of hormonal changes, primarily the influence of testosterone.
- Bone Growth and Skeletal Shape: Puberty affects bone growth, leading to changes in skeletal shape. Some areas experience disproportionate growth, such as the shoulders and jaw, resulting in noticeable differences in male and female skeletal shapes. Adult men generally have heavier bones compared to women.
- Lean Body Mass: Adult men, on average, have approximately 150% of the lean body mass of adult females. This higher lean body mass contributes to the overall physical strength and muscularity observed in males.
- Body Fat: In contrast to lean body mass, adult men have about 50% of the body fat of adult females. This difference in body fat distribution is influenced by hormonal factors and contributes to the characteristic male body shape.
- Muscle Development: Muscle growth occurs primarily during the later stages of puberty. It is worth noting that muscle development can continue even after boys reach biological adulthood. The peak rate of muscle growth, often referred to as the “strength spurt,” typically occurs about one year after experiencing the peak growth rate.
- Gynecomastia: During puberty, the male breast tissue and nipples may develop fat pads. In some cases, this development becomes more apparent, resulting in a condition called gynecomastia. Gynecomastia can involve one or both breasts and is usually temporary rather than a permanent phenomenon.
These changes in male musculature and body shape are influenced by hormonal shifts, particularly the effects of testosterone. Individual variations exist, and the timing and extent of these changes may vary among individuals.
Erections
Erections are a natural physiological response in males and play a significant role during different stages of development. Here’s an overview based on the provided information:
- Nocturnal Penile Tumescence (NPT): Erections that occur during sleep or upon waking up are medically termed nocturnal penile tumescence. They are commonly known as “morning wood.” It is normal for the penis to become erect during sleep, and men or boys often wake up with an erection.
- Puberty and Increased Frequency: As boys enter their teenage years and go through puberty, erections become more frequent. Hormonal changes, particularly the surge in testosterone, contribute to the increased occurrence of erections during this stage of development.
- Spontaneous Erections: Erections can occur spontaneously at any time of the day. They are not solely limited to sleep or waking up. If a male is clothed, an erection may cause a noticeable bulge or “hump.” To conceal or hide an erection, wearing close-fitting underwear, longer shirts, or looser clothing can help.
- Erections in Prepubescent Children and Infants: Spontaneous erections can also occur in male prepubescent children and infants. These involuntary or unwanted erections are normal physiological responses and can happen even before birth.
- Embarrassment and Social Situations: Spontaneous erections, especially when they occur in public settings like classrooms or living rooms, can be embarrassing for individuals. However, it’s important to remember that these erections are a normal part of male physiology and not within conscious control.
Understanding the natural occurrence of erections and their association with different stages of development can help alleviate concerns and normalize the experience.
Foreskin retraction
During puberty, the foreskin of a boy’s penis undergoes changes that allow for retraction. The tip and opening of the foreskin gradually become wider, enabling it to be pulled back down the shaft and behind the glans without pain or difficulty. This is made possible by the disintegration of the membrane that bonds the inner surface of the foreskin with the glans, allowing the foreskin to separate from the glans. Over time, the foreskin becomes retractable.
Research conducted by Øster (1968) showed that as puberty progresses, the percentage of boys able to retract their foreskins increases. At ages 12-13, only 60% of boys were able to retract their foreskins, but this number increased to 85% by ages 14-15 and 95% by 16-17. Øster also found that 1% of those unable to fully retract their foreskins experienced phimosis, a condition where the foreskin is too tight, while the rest were partially able to retract it. This finding was supported by studies conducted by Kayaba et al. (1996) and Ishikawa and Kawakita (2004), which found similar rates of foreskin retractability in their respective samples of boys.
Once a boy is able to retract his foreskin, it becomes important to incorporate penile hygiene into his routine body care. Although the association between circumcision status and optimal penile hygiene is inconclusive, various studies suggest that boys should be educated about proper hygiene practices. This includes retracting the foreskin while urinating and rinsing under it and around the glans during bathing. Regular washing under the foreskin has been found to reduce the risk of penile disorders. However, excessive washing with soap should be avoided as it can dry out the tissues and cause non-specific dermatitis, as reported by Birley et al. (1993).
It’s important to note that each individual’s development may vary, and if there are concerns or difficulties with foreskin retraction or penile hygiene, it is advisable to consult a healthcare professional for guidance.
Pubic hair
During puberty, boys experience the growth of pubic hair, which typically appears shortly after the enlargement of the genitalia. The initial signs of pubic hair development are usually observed at the base of the penis on the abdominal side. This marks the beginning of stage 2 of pubic hair growth. Within another 6-12 months, boys progress to stage 3, during which the number of pubic hairs increases significantly, making them too numerous to count.
As puberty continues, boys enter stage 4 of pubic hair development. At this stage, the pubic hairs densely populate the “pubic triangle,” the area between the lower abdomen and the base of the penis. Finally, in stage 5, pubic hair spreads to the thighs and starts to extend upward towards the navel as part of the developing abdominal hair. Stage 5 represents the completion of pubic hair growth.
It’s important to note that the timing and progression of pubic hair growth can vary among individuals. While the general sequence described here is common, the exact timeline and patterns may differ. Pubic hair development is a natural part of the physical changes that occur during puberty in boys.
Body and facial hair
After the onset of pubic hair growth, other areas of the body that are responsive to androgens, or male hormones, may develop androgenic hair. The typical progression of androgenic hair growth follows a certain sequence, although it may vary among individuals. Generally, the order of development includes underarm (axillary) hair, perianal hair, upper lip hair, sideburn (preauricular) hair, periareolar hair, and the beard area.
However, it’s important to note that the specific order and timing of hair growth can differ among individuals. Some people may experience variations in the sequence described above. In addition, the growth of arm, leg, chest, abdominal, and back hair tends to occur more gradually. The amount and distribution of body hair can vary significantly among adult men, and there are notable differences in the timing and quantity of hair growth among different racial groups.
Facial hair, such as beard growth, often begins to appear during late adolescence but may not manifest until a later stage for some individuals. Following puberty, facial hair continues to undergo changes. It becomes coarser, darker, and thicker over a period of 2-4 years. It’s worth mentioning that some men may not develop a full beard until several years after puberty has ended. On the other hand, the appearance of chest hair can occur during puberty or even years later, and not all men will develop substantial chest hair.
The growth and distribution of body and facial hair are influenced by various factors, including genetic predisposition and hormonal activity. As with many aspects of human biology, there is a wide range of variation in hair growth patterns among individuals.
Voice change and Adam’s apple
During puberty, both boys and girls experience growth of the larynx, or voice box, under the influence of androgens, although the extent of growth is more pronounced in boys. This growth leads to a significant change in the male voice, causing it to drop and deepen. However, it’s important to note that this change doesn’t typically occur suddenly or “overnight.” Instead, it takes place gradually over time.
The lengthening and thickening of the vocal folds in the larynx result in a lower fundamental frequency of the voice, causing the pitch to become deeper. Prior to puberty, the size of the larynx is relatively similar between boys and girls, but as hormonal changes occur, the larynx in boys undergoes more substantial growth.
In the early stages of untrained voices, the process of voice change may be accompanied by some unsteadiness in vocalization. This is normal and tends to resolve as the voice continues to mature. The majority of the voice change occurs during stage 3-4 of male puberty, which typically coincides with the period of peak growth.
On average, the adult pitch of the male voice is attained around the age of 15 years. However, it’s important to note that the voice may not fully stabilize until the early twenties. The timing of voice change may vary among individuals. It is worth mentioning that the deepening of the voice usually occurs before the development of significant facial hair, typically with a gap of several months to years between the two processes.
Changes in females
Breast development
- Breast development in girls is one of the primary physical signs of puberty. It typically begins with the emergence of a firm and tender lump beneath the center of the areola in one or both breasts. This initial stage of breast development is known as thelarche and occurs, on average, around 10.5 years of age.
- According to the Tanner staging system, which is commonly used to assess pubertal development, thelarche corresponds to stage 2 of breast development. At this stage, the breasts are still relatively flat and prepubertal in appearance. Over the next 6-12 months, there is noticeable swelling and growth in both breasts. The swelling softens and extends beyond the edges of the areolae, becoming more palpable and visible. This marks stage 3 of breast development.
- Within approximately another 12 months (stage 4), the breasts continue to grow and approach their mature size and shape. The areolae and nipples also undergo changes, forming a secondary mound. By stage 5, which represents the final stage of breast development, the breasts have reached their mature size and shape. The areolae and nipples typically blend into the contour of the breast, although it’s important to note that there is considerable variation in the sizes and shapes of adult breasts, making stages 4 and 5 less distinguishable in some cases.
- It’s worth mentioning that breast development is a gradual process that can vary in duration and timing among individuals. The Tanner staging system provides a general framework for understanding the progression of breast development, but individual variations in sizes and shapes of breasts should also be considered.
Pubic hair
- Pubic hair is one of the visible changes that occur during puberty, typically appearing a few months after the onset of breast development, which is known as thelarche. The emergence of pubic hair is referred to as pubarche.
- Initially, the pubic hairs are often visible along the labia, and this marks the early stage of pubic hair development, described as Tanner stage 2. Within another 6-12 months, the pubic hair becomes more abundant and extends to the pubic mound, reaching Tanner stage 3. At this stage, the hairs are too numerous to count.
- As pubic hair continues to grow, it progresses to Tanner stage 4, where the pubic hairs densely fill the area known as the “pubic triangle.” Finally, in Tanner stage 5, the pubic hair extends beyond the pubic area, spreading to the thighs and sometimes upward towards the navel, forming abdominal hair.
- It’s interesting to note that pubic hair development can sometimes occur prior to breast development. In about 15% of girls, the appearance of pubic hair precedes the onset of breast development.
- Pubic hair growth is a normal part of sexual maturation and varies in timing and density among individuals. The Tanner staging system provides a framework for understanding the progression of pubic hair development, allowing healthcare professionals to assess and track pubertal changes in girls.
Vagina, uterus, ovaries
- During puberty, several changes occur in the female reproductive system, including the vagina, uterus, and ovaries. These changes are primarily influenced by the increased levels of estrogen.
- One significant change is the keratinization of the perineal skin, which is the result of estrogen’s effect. This process helps increase the skin’s resistance to infections. Additionally, the mucosal surface of the vagina undergoes transformation in response to elevated estrogen levels. It becomes thicker and changes in color from a brighter red to a duller pink hue compared to prepubertal vaginal mucosa. The vaginal mucosa transitions into a multilayered structure, with a superficial layer of squamous cells. Estrogen also plays a role in increasing the glycogen content in the vaginal epithelium, which becomes essential for maintaining the vaginal pH. The presence of whitish secretions, known as physiologic leukorrhea, is a normal effect of estrogen as well.
- In the two years following thelarche (the onset of breast development), the uterus, ovaries, and the follicles within the ovaries undergo growth. The uterus increases in size, and the ovaries develop larger follicles, which are visible through ultrasound examination. Before puberty, the ratio between the uterine body and cervix is approximately 1:1. However, during the completion of the pubertal period, this ratio typically increases to 2:1 or 3:1.
- These changes in the vagina, uterus, and ovaries are part of the normal maturation process of the female reproductive system during puberty, preparing the body for potential future reproductive functions.
Menstruation and fertility
- Menstruation, also known as the menstrual cycle, and fertility are important aspects of a woman’s reproductive health. Menstruation typically begins with the first menstrual bleeding, which is called menarche. Menarche usually occurs around two years after the onset of breast development (thelarche).
- The average age of menarche in the United States is around 12.5 years, although it can vary. Most American girls experience their first period between the ages of 11 and 13, but it can happen earlier (before the 11th birthday) or later (after the 14th birthday). In general, the normal range for menarche is between 8 and 16 years of age. In Canada, the average age of menarche is around 12.72, while in the United Kingdom it is approximately 12.9.
- During the first two years after menarche, the timing between menstrual periods, known as menses, may not be regular. It takes time for the hormonal fluctuations and ovulation to establish a more predictable pattern. Ovulation, the release of an egg from the ovary, is necessary for fertility. However, in the early stages of menarche, ovulation may or may not occur regularly.
- In the first year after menarche, approximately 80% of menstrual cycles are anovulatory, meaning no egg is released. This percentage decreases to around 50% in the third year and 10% in the sixth year. It is not guaranteed that ovulation will initiate immediately after menarche. Some girls may experience irregular menstrual cycles and anovulation for several years after menarche, putting them at a higher risk for reduced fertility in the future.
- It is important for girls and young women to understand that irregular menstrual cycles are common in the early stages of menarche. However, if irregularity persists for an extended period, it is advisable to consult a healthcare professional to evaluate and address any potential underlying issues.
- Understanding the menstrual cycle and its variations can help individuals manage their reproductive health and fertility effectively.
Body shape, fat distribution, and body composition
- During puberty, there are significant changes in body shape, fat distribution, and body composition, primarily driven by hormonal changes, particularly rising estrogen levels in females.
- One noticeable change is the widening of the lower half of the pelvis, which results in increased hip width. This widening of the hips is an adaptation that provides a larger birth canal for potential childbirth in the future.
- In terms of body composition, females tend to have a higher percentage of body fat compared to males. The increase in estrogen leads to a greater accumulation of fat tissue, particularly in areas such as the breasts, hips, buttocks, thighs, upper arms, and pubic region. These are the typical areas where females tend to exhibit fat distribution, contributing to the development of a curvier body shape.
- Additionally, sex differences in local skeletal growth also play a role in shaping the female body during puberty. The combination of increased fat deposition and skeletal growth contributes to the development of the characteristic female body shape by the end of puberty.
- On average, girls have approximately 6% more body fat than boys by the age of 10. This difference in body fat percentage persists throughout puberty and into adulthood.
- It’s important to note that these are general patterns, and individual variations in body shape and fat distribution exist. Factors such as genetics, lifestyle, and overall health can also influence body composition and shape during puberty.
- Understanding these changes in body shape, fat distribution, and body composition can help individuals navigate and appreciate the natural processes occurring during puberty. Embracing and maintaining a positive body image is important for promoting overall well-being and self-confidence during this transformative period.
Body odor and acne
- During puberty, the increased levels of androgens, such as testosterone, can lead to changes in body odor and an increased susceptibility to acne.
- As androgen levels rise, the composition of fatty acids in perspiration changes, resulting in a more “adult” body odor. This change in body odor often occurs before the onset of other pubertal changes like breast development (thelarche) and pubic hair growth (pubarche). The exact timing can vary among individuals, with some experiencing it earlier or later than others.
- Another effect of androgens is the increased secretion of oil, known as sebum, from the sebaceous glands in the skin. This increase in sebum production can contribute to the development of acne, a common skin condition associated with puberty. Acne occurs when the hair follicles become clogged with excess sebum, dead skin cells, and bacteria, leading to the formation of pimples, blackheads, and other skin blemishes.
- The severity of acne can vary greatly among individuals, ranging from mild occasional breakouts to more severe and persistent cases. Factors such as genetics, hormonal fluctuations, skin type, and hygiene practices can influence the development and progression of acne during puberty.
- It’s important to note that while acne is common during puberty, it is not exclusive to this period. Some individuals may continue to experience acne into adulthood, while others may see improvements as they mature. Proper skincare practices, including gentle cleansing, avoiding excessive touching or picking of the skin, and using non-comedogenic products, can help manage and prevent acne breakouts.
- If acne becomes severe or significantly impacts an individual’s self-esteem and well-being, it is advisable to seek medical advice from a dermatologist or healthcare professional who can provide appropriate treatment options, including topical or oral medications, to help manage the condition.
- Overall, understanding the hormonal changes and their effects on body odor and acne during puberty can assist individuals in maintaining good hygiene practices and seeking appropriate care when needed, promoting healthy skin and self-confidence.
Visual and other effects of hormonal changes
- Hormonal changes during puberty have various visual and other effects on the body, particularly in girls.
- Estradiol, the primary female sex hormone, plays a significant role in the development of certain features. It causes the lips and oral mucosa to thicken, resulting in fuller lips. The vulva, which includes the external female genitalia, undergoes further development under the influence of estradiol. The skin in the vulva and vagina becomes thicker and stratified, and there is growth in the myoepithelial layer and smooth muscle of the vagina. Estradiol also promotes pronounced growth of the labia minora (inner lips of the vulva) and, to a lesser extent, the labia majora (outer lips of the vulva).
- Estradiol contributes to the increased production of pheomelanin, a pigment that gives a reddish color to the lips, labia minora, and sometimes the labia majora. Additionally, estradiol, along with other ovarian steroids, causes darkening of the areola, the circular area surrounding the nipple.
- Testosterone, although primarily a male sex hormone, also plays a role in female puberty. It leads to enlargement of the clitoris, a sensitive organ in the female genitalia. Testosterone may also have important effects on the growth and maturation of the vestibular bulbs, corpus cavernosum of the clitoris, and urethral sponge.
- The changes initiated by estradiol in the vulva, as well as its direct effects, appear to influence the functioning of the lower urinary tract. The hormonal fluctuations during puberty can impact the urinary system, potentially affecting urinary habits and patterns.
- Overall, these hormonal changes during puberty result in visual transformations in the female body, such as fuller lips, development of the vulva, changes in pigmentation, and clitoral enlargement. It’s important to note that these changes are part of the normal physiological process of puberty, enabling the body to mature and develop reproductive functions.
Underarm hair
- During puberty, one of the noticeable changes in both boys and girls is the development of underarm hair. Underarm hair growth begins with sparse and fine hairs, gradually thickening and darkening over time.
- As hormonal changes occur during puberty, the androgens, particularly testosterone, stimulate the hair follicles in the underarm region. These hormones cause the follicles to produce thicker, coarser hair. The initial growth may be light or sparse, but as puberty progresses, the hair becomes more visible and prominent.
- The process of underarm hair growth varies among individuals. Some may experience more rapid and pronounced hair growth, while others may have a slower progression. The timing and extent of underarm hair development can also differ between boys and girls.
- Underarm hair serves as a secondary sexual characteristic, distinguishing individuals as they transition into adulthood. Its growth is a natural and normal part of the physical changes that occur during puberty.
Neurohormonal process
The neurohormonal process plays a crucial role in the development of the reproductive system during puberty. It involves the intricate interplay between the central nervous system, specifically the hypothalamus, the pituitary gland, and the gonads (ovaries or testes), as well as the adrenal glands. This process is responsible for the initiation and regulation of the physiological changes that occur during puberty.
The neurohormonal process begins with the release of gonadotropin-releasing hormone (GnRH) by the hypothalamus. GnRH is released in a pulsatile manner, and these pulses stimulate the cells in the anterior pituitary gland. In response to GnRH, the anterior pituitary gland releases two key hormones called luteinizing hormone (LH) and follicle-stimulating hormone (FSH) into the bloodstream.
The rising levels of LH and FSH in the bloodstream then act on the ovaries or testes. In females, the ovaries respond to the stimulation by LH and FSH by growing and maturing. They begin to produce the hormone estradiol, which is a type of estrogen. In males, the testes respond by growing and initiating the production of testosterone, the primary male sex hormone.
The increasing levels of estradiol and testosterone in the bloodstream are responsible for the characteristic body changes observed during female and male puberty, respectively. These changes include the development of secondary sexual characteristics, such as breast development, widening of hips, growth of pubic and underarm hair in females, and deepening of the voice, growth of facial and body hair, and muscle development in males.
It’s important to note that the onset of the neurohormonal process may occur before the visible body changes become apparent. This means that the hormonal changes within the body may already be underway for approximately 1-2 years before the external signs of puberty become noticeable.
Overall, the neurohormonal process of puberty represents a complex cascade of events involving the hypothalamus, pituitary gland, gonads, and hormonal interactions. It is this intricate interplay between the central nervous system and the endocrine system that drives the development of reproductive capabilities and the physical changes that occur during puberty.
Components of the endocrine reproductive system
The endocrine reproductive system is a complex network of organs and glands that work together to regulate and control reproductive functions in the body. Several components play crucial roles in this system:
- Arcuate Nucleus of the Hypothalamus: The arcuate nucleus, located in the hypothalamus of the brain, acts as the driver of the reproductive system. Within this nucleus, neurons generate and release pulses of gonadotropin-releasing hormone (GnRH) into the portal venous system of the pituitary gland. GnRH is responsible for stimulating the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland.
- Pituitary Gland: The pituitary gland, often referred to as the “master gland,” responds to the pulsatile GnRH signals from the hypothalamus by releasing LH and FSH into the bloodstream. LH and FSH are released in a pulsatile pattern, with their secretion regulated by the frequency and amplitude of GnRH pulses. LH and FSH play essential roles in the regulation of reproductive processes in both males and females.
- Gonads (Testes and Ovaries): The gonads, which are the testes in males and the ovaries in females, respond to the rising levels of LH and FSH released by the pituitary gland. In males, LH stimulates the Leydig cells in the testes to produce testosterone, the primary male sex hormone. FSH, on the other hand, stimulates the Sertoli cells in the testes, supporting the maturation of sperm cells. In females, LH triggers the release of an egg from the ovary (ovulation) and stimulates the production of progesterone. FSH, along with LH, promotes the growth and development of ovarian follicles and the production of estrogen.
- Adrenal Glands: The adrenal glands, located on top of the kidneys, are a secondary source of steroid hormones. Adrenal maturation, known as adrenarche, typically occurs in mid-childhood, preceding the onset of gonadarche. The adrenal glands produce and release steroid hormones, including androgens such as dehydroepiandrosterone (DHEA) and DHEA sulfate (DHEA-S). While these hormones are not directly involved in reproductive functions, they play important roles in the development of secondary sexual characteristics and contribute to overall hormonal balance.
Overall, the endocrine reproductive system relies on the coordination and interaction of various components, including the arcuate nucleus of the hypothalamus, the pituitary gland, the gonads (testes and ovaries), and even the adrenal glands. These components work together to regulate the secretion of hormones necessary for reproductive processes, including the production of sex hormones, maturation of gametes, and regulation of the menstrual cycle or spermatogenesis.
Major hormones
The endocrine system relies on various hormones to regulate and control reproductive processes. Here are the major hormones involved:
- Neurokinin B and Kisspeptin: Neurokinin B and kisspeptin are neuropeptides present in KNDy neurons of the hypothalamus. They play a critical role in initiating the release of gonadotropin-releasing hormone (GnRH) at the onset of puberty. These neuropeptides are part of the control system that triggers the activation of the reproductive system.
- GnRH (Gonadotropin-Releasing Hormone): GnRH is a peptide hormone released from the hypothalamus. It stimulates the gonadotrope cells in the anterior pituitary gland to secrete luteinizing hormone (LH) and follicle-stimulating hormone (FSH). GnRH acts as a key regulator of the reproductive system, initiating the release of other hormones involved in reproductive processes.
- LH (Luteinizing Hormone): LH is a larger protein hormone secreted by the gonadotrope cells in the anterior pituitary gland. It circulates in the bloodstream and primarily targets the Leydig cells in the testes and the theca cells in the ovaries. LH levels increase significantly during puberty, approximately 25-fold, playing a crucial role in the maturation of the reproductive organs and the production of sex hormones.
- FSH (Follicle-Stimulating Hormone): FSH is another protein hormone secreted by the gonadotrope cells in the anterior pituitary gland. It acts alongside LH to regulate reproductive processes. FSH primarily targets the ovarian follicles in females and the Sertoli cells and spermatogenic tissue in males. FSH is essential for follicular development in females and the production of sperm in males.
- Testosterone: Testosterone is a steroid hormone primarily produced by the Leydig cells in the testes. It is also produced in smaller amounts by the theca cells in the ovaries and the adrenal cortex. Testosterone is the primary androgen in mammals and acts on androgen receptors throughout the body. It plays a crucial role in the development and maintenance of male reproductive tissues and secondary sexual characteristics.
- Estradiol: Estradiol is a steroid hormone derived from the aromatization of testosterone. It is the principal estrogen in humans and acts on estrogen receptors throughout the body. While the ovaries, specifically the granulosa cells, produce the largest amounts of estradiol, smaller amounts are also derived from testicular and adrenal testosterone. Estradiol is involved in the development and maintenance of female reproductive tissues and secondary sexual characteristics.
- Adrenal Androgens: Adrenal androgens are steroids produced by the zona reticulosa of the adrenal cortex in both sexes. The major adrenal androgens include dehydroepiandrosterone (DHEA) and androstenedione, which serve as precursors for testosterone. Additionally, dehydroepiandrosterone sulfate is present in significant amounts in the blood. Adrenal androgens contribute to the androgenic events of early puberty in girls.
- IGF1 (Insulin-like Growth Factor 1): IGF1 is a hormone that rises substantially during puberty in response to increasing levels of growth hormone. It is considered the primary mediator of the pubertal growth spurt, contributing to the growth and development of various tissues, including bones and muscles.
- Leptin: Leptin is a protein hormone produced by adipose tissue (fat cells). It primarily targets the hypothalamus and serves as a rough indicator of adipose mass, regulating appetite and energy metabolism. Leptin also plays a permissive role in female puberty, as it signals the body’s readiness for reproductive development by achieving an adequate body mass.
These major hormones, along with their interactions and feedback mechanisms, orchestrate the intricate processes of the endocrine reproductive system, ensuring the development, maturation, and maintenance of reproductive functions in both males and females.
Hormonal changes in boys
During puberty, boys undergo significant hormonal changes that contribute to their physical and sexual maturation. Here are the key hormonal changes in boys:
- Maturation of the Hypothalamus: The early stages of hypothalamic maturation in boys are similar to those in girls, but they occur about 1-2 years later. The hypothalamus plays a crucial role in regulating the release of hormones involved in puberty.
- Rise in Testosterone Levels: Luteinizing hormone (LH) stimulates the Leydig cells in the testes to produce testosterone. As puberty progresses, blood levels of testosterone begin to rise. Interestingly, during much of puberty, nighttime levels of testosterone are higher than daytime levels. This hormone is responsible for the development of secondary sexual characteristics in boys, such as deepening of the voice, facial and body hair growth, and increased muscle mass.
- Conversion of Testosterone to Estradiol: A significant portion of testosterone in adolescent boys is converted to estradiol, a form of estrogen. Estradiol plays a vital role in mediating the growth spurt, bone maturation, and closure of the epiphyseal plates in boys, similar to its effects in girls. However, the conversion of testosterone to estradiol in boys can also lead to the development of gynecomastia, the enlargement of breast tissue. This is a temporary effect experienced by a large proportion of boys during puberty due to high levels of estradiol.
- Rise in Testosterone and Dihydrotestosterone: During the teenage years, testosterone levels gradually increase in young men. Testosterone and its derivative, dihydrotestosterone (DHT), mediate most of the effects through androgen receptors in target organs, including the bowels. DHT is particularly involved in the development of the male external genitalia and prostate gland.
These hormonal changes contribute to the overall physical and sexual maturation of boys during puberty. Testosterone and estradiol play essential roles in the development of secondary sexual characteristics, bone growth, and the establishment of reproductive functions. It’s important to note that the timing and progression of these hormonal changes can vary among individuals, and the effects of puberty may manifest differently in different boys.
Hormonal changes in girls
During puberty, girls experience significant hormonal changes that lead to the development of secondary sexual characteristics and reproductive functions. Here are the key hormonal changes in girls:
- LH and Testosterone Production: As the amplitude of LH pulses increases, the theca cells in the ovaries start producing testosterone along with smaller amounts of progesterone. Some of the testosterone moves into nearby cells called granulosa cells. Subsequent increases in FSH levels stimulate the aromatase activity of these granulosa cells, converting most of the testosterone into estradiol, which is then released into the bloodstream. The remaining testosterone, along with adrenal androgens, contributes to androgenic changes during female puberty, such as the growth of pubic hair, other androgenic hair, body odor, and acne.
- Estradiol Production and Estrogenic Changes: Rising levels of estradiol, the primary form of estrogen in females, lead to estrogenic changes during puberty. These changes include a growth spurt, acceleration of bone maturation and closure, breast development, increased fat composition, growth of the uterus, thickening of the endometrium and vaginal mucosa, and widening of the lower pelvis. Estradiol is responsible for the development of female secondary sexual characteristics and prepares the reproductive organs for potential fertility.
- Positive Feedback and Ovulation: As estradiol levels gradually rise and other autoamplification processes occur, the hypothalamic “gonadostat” reaches a point of maturation where the feedback sensitivity becomes positive. This positive feedback is a hallmark of female sexual maturity and allows for the mid-cycle surge of LH, which is necessary for ovulation—the release of a mature egg from the ovary.
- Growth Hormone and IGF1: Throughout puberty, growth hormone levels increase steadily. Alongside this, levels of insulin-like growth factor 1 (IGF1), which is stimulated by growth hormone, also rise. IGF1 plays a crucial role in the pubertal growth spurt. However, as puberty comes to an end, IGF1 levels start to decline, and growth finishes as estradiol completes the closure of the epiphyses (growth plates) in the long bones, leading to the attainment of adult height.
These hormonal changes in girls orchestrate the physical, reproductive, and skeletal maturation that occurs during puberty, resulting in the transition from childhood to adulthood. The interplay of LH, FSH, testosterone, estradiol, growth hormone, and IGF1 regulates the timing and progression of these developmental changes.
Differences between male and female puberty
Puberty is a transformative period in a person’s life, marking the transition from childhood to adulthood. While both boys and girls experience significant physical and hormonal changes during this stage, there are notable differences between male and female puberty.
One of the primary differences is the age at which puberty typically begins and ends. Girls usually enter puberty between the ages of 10 and 11 and complete it around 15 to 17 years old. In contrast, boys begin puberty slightly later, around 11 to 12 years old, and generally finish around 16 to 17 years old. It’s important to note that these ages can vary within a wide range and are not set in stone.
The major sex hormones involved in puberty also differ between males and females. For boys, the principal sex hormone is testosterone. Testosterone is responsible for the development of masculine characteristics, a process known as virilization. However, testosterone metabolism in males produces another hormone called estradiol, which is a form of estrogen. It’s worth mentioning that boys have lower estradiol levels compared to girls, primarily due to differences in body fat and hormonal levels.
In terms of physical growth, boys experience a delayed and more prolonged growth spurt compared to girls. The male growth spurt begins later, progresses at a slower rate, and lasts longer before the growth plates in the long bones fuse. As a result, boys continue to grow for about six years after the initial pubertal changes become visible. On the other hand, girls undergo a more rapid growth spurt that usually concludes within four years after the onset of puberty. Despite girls starting puberty shorter on average than boys, adult men are generally taller than adult women. This difference in adult height can be attributed to the later onset of the growth spurt in males and lower levels of estradiol during adulthood.
In females, the hormonal maturation during puberty is more complex. Multiple steroid hormones, including testosterone, estradiol, and progesterone, as well as prolactin, play crucial roles in the physiological changes that occur. The production of gonadal steroids in girls begins with testosterone, which is rapidly converted to estradiol within the ovaries. However, the rate of conversion from testosterone to estradiol varies widely during early puberty, leading to diverse patterns of development in secondary sexual characteristics among girls. Additionally, progesterone production starts with the onset of ovulatory cycles in girls, with low levels being produced in the adrenal glands of both boys and girls prior to puberty. Estradiol levels rise earlier and reach higher levels in women compared to men. Besides promoting breast and uterus growth, estradiol is the primary hormone driving the pubertal growth spurt and the maturation and closure of the growth plates.
Overall, the differences between male and female puberty encompass the age of onset, the primary sex hormones involved (testosterone and estradiol), the rate and duration of growth spurts, and the development of secondary sexual characteristics. While these variations exist, it’s important to remember that individuals may have unique experiences, and there can be considerable diversity within each gender.
| Aspect of Puberty | Girls | Boys |
|---|---|---|
| Age Range | 10-11 to 15-17 years old | 11-12 to 16-17 years old |
| Major Sex Hormones | Estrogens (estradiol) | Androgens (testosterone) |
| Progesterone | ||
| Prolactin | ||
| Physical Growth | Rapid growth spurt | Delayed and prolonged growth |
| spurt | ||
| Continued growth for about | ||
| six years after initial | ||
| pubertal changes | ||
| Hormonal Maturation | Testosterone converted | Testosterone metabolized |
| to estradiol in ovaries | to estradiol | |
| Estradiol levels rise | Lower estradiol levels | |
| earlier and reach higher | than in girls | |
| levels | ||
| Secondary Sexual | Breast and uterus growth | Virilization and development |
| Characteristics | of masculine features | |
| Pubertal growth spurt | ||
| and epiphyseal maturation | ||
| and closure |
Importance of Puberty
Puberty is a critical and transformative stage in human development, marking the transition from childhood to adulthood. It is a complex process driven by hormonal changes that lead to physical, reproductive, and psychological maturation. The importance of puberty can be understood in several key aspects:
- Physical Development: Puberty brings about significant physical changes in individuals. It is characterized by the development of secondary sexual characteristics, such as breast development in girls and facial hair growth in boys. There is also a growth spurt, where individuals experience a rapid increase in height and weight. These physical changes are essential for establishing adult body proportions and preparing the body for sexual and reproductive functions.
- Reproductive Maturation: One of the primary purposes of puberty is to prepare the body for reproduction. In girls, puberty involves the maturation of the reproductive organs, including the ovaries, uterus, and vagina. Menstruation begins, indicating the potential for fertility. In boys, puberty leads to the development of the testes, penis, and other reproductive structures. The production of sperm begins, enabling the ability to father a child. Puberty is crucial for ensuring the continuation of the human species through reproductive capabilities.
- Psychological and Emotional Changes: Puberty is a period of significant psychological and emotional development. Hormonal changes during this time can impact mood, behavior, and cognitive functioning. Adolescents may experience increased independence, self-awareness, and a search for personal identity. It is a time of exploration, self-discovery, and forming relationships. Puberty plays a vital role in shaping an individual’s social, emotional, and cognitive development as they transition from childhood to adulthood.
- Bone and Muscle Development: During puberty, there is a rapid increase in bone density and muscle mass. This is important for achieving optimal skeletal strength and muscle function in adulthood. Adequate bone and muscle development during this period contribute to overall physical health and reduce the risk of musculoskeletal disorders later in life.
- Overall Well-being and Self-esteem: Going through puberty and experiencing the associated changes is a significant milestone for individuals. It can impact self-esteem, body image, and overall well-being. Understanding and accepting these changes as a natural part of development is crucial for positive self-perception and mental health. Puberty provides an opportunity for individuals to develop a healthy body image, self-confidence, and a positive sense of identity.
In summary, puberty is a fundamental and transformative stage of human development. It brings about physical, reproductive, psychological, and emotional changes that are essential for transitioning into adulthood. Understanding and supporting individuals through this period of growth and development is vital for their overall well-being and successful navigation into adult life.
FAQ
What is puberty?
Puberty is a natural and gradual process of physical, reproductive, and psychological changes that occur during adolescence. It is the transition from childhood to adulthood.
At what age does puberty typically begin?
Puberty usually begins between the ages of 8 and 13 in girls, and between the ages of 9 and 14 in boys. However, the timing can vary widely among individuals.
What are the signs of puberty in girls?
Signs of puberty in girls include breast development, the growth of pubic and underarm hair, the onset of menstruation (menarche), growth spurts, and changes in body shape.
What are the signs of puberty in boys?
Signs of puberty in boys include testicular and scrotal growth, the growth of pubic, facial, and underarm hair, deepening of the voice, growth spurts, and changes in body shape.
Are there emotional changes during puberty?
Yes, hormonal changes during puberty can have an impact on emotions and behavior. Adolescents may experience mood swings, increased sensitivity, and changes in social interactions.
How long does puberty last?
Puberty typically lasts about 2 to 5 years, although individual experiences may vary. The completion of puberty is marked by the attainment of sexual and physical maturity.
Is it normal for the timing of puberty to vary among individuals?
Yes, there is a wide range of normal variation in the timing of puberty. Factors such as genetics, nutrition, overall health, and environmental factors can influence when puberty begins and progresses.
What can parents do to support their child during puberty?
Parents can provide information and open communication about the changes of puberty, addressing any concerns or questions their child may have. Creating a supportive and understanding environment can help adolescents navigate this transitional period.
Are there any health concerns related to puberty?
While puberty itself is a normal process, it can be accompanied by various health concerns. Regular medical check-ups, including discussions about growth, development, and sexual health, can help address any potential issues or provide appropriate guidance.
Can puberty affect academic performance?
During puberty, hormonal changes and emotional adjustments may temporarily impact academic performance. It is important for parents, teachers, and caregivers to provide support, understanding, and necessary accommodations to help adolescents manage these challenges and maintain academic progress.