What is Nondisjunction?
- Nondisjunction can define as failure of homologous chromosomes or sister chromatids to separate properly during cell division (mitosis or meiosis).
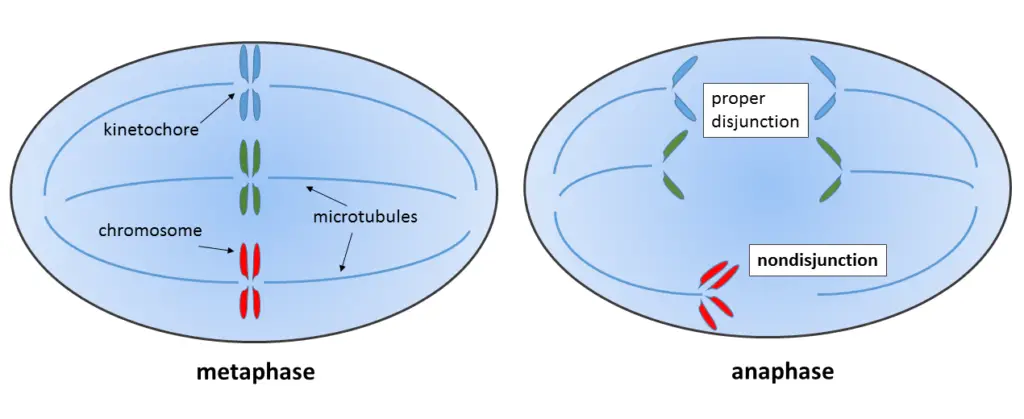
- It usually happens at anaphase stage, when both chromatids or chromosomes get pulled to one side of the cell.
- Because of this, daughter cells/gametes form with wrong chromosome number, this abnormal state called aneuploidy.
- Aneuploid cells may have one extra chromosome (trisomy, n+1 or 2n+1) or missing one (monosomy, n−1 or 2n−1).
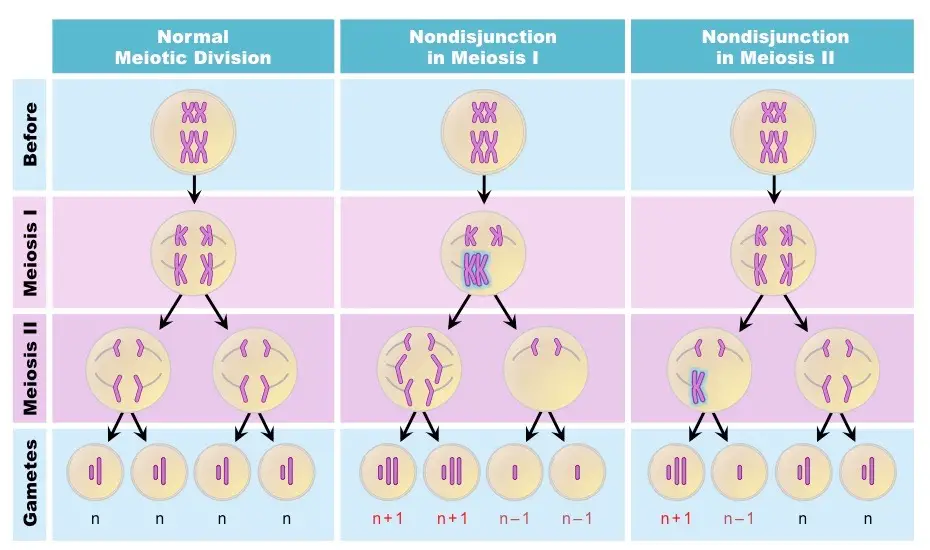
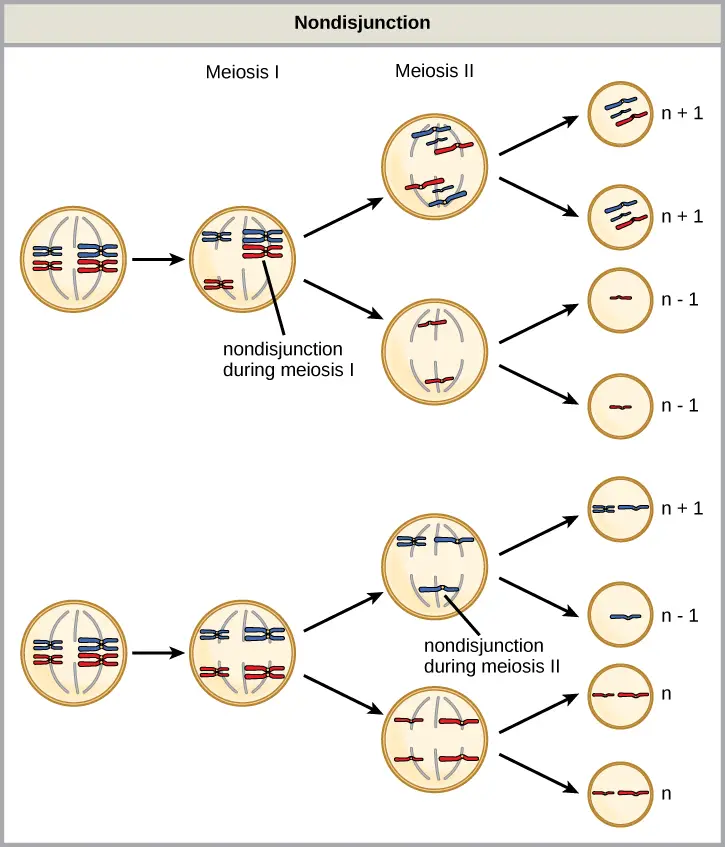
- Three kinds of nondisjunction mostly seen—during Meiosis I, Meiosis II, or Mitosis.
- Meiosis I – when homologous chromosomes (tetrads) fail to separate, all gametes become aneuploid (two n+1 & two n−1).
- Meiosis II – when sister chromatids not separate at anaphase II, two gametes normal (n) and two abnormal (n+1 & n−1).
- Mitosis – seen in somatic cells, gives one daughter with 2n+1 and another with 2n−1 chromosomes.
- Mitotic nondisjunction leads to somatic mosaicism, means only some cells in body show chromosome mistake.
- Molecularly, it can happen by inactivation of vital proteins like topoisomerase II, condensin, or separase.
- Also when the spindle assembly checkpoint (SAC) fails to work properly, wrong segregation occurs.
- The cohesin proteins that hold chromatids sometimes weaken with age—especially in female oocytes, causing segregation errors.
- Sometimes, wrong crossing over (recombination) or misplaced crossovers also cause this.
- Meiotic nondisjunction often produce aneuploidy syndromes like:
- Down syndrome (Trisomy 21)
- Klinefelter syndrome (XXY)
- Turner syndrome (Monosomy X)
- Edwards syndrome (Trisomy 18)
- Patau syndrome (Trisomy 13)
- Triple X (XXX)
- XYY syndrome, etc.
- Sex chromosome nondisjunction gives several abnormal karyotypes, depending on which chromosome fail to separate.
- In few cancers (like retinoblastoma), mitotic nondisjunction plays role by creating mosaic condition in cells.
Types of Nondisjunction
- Meiosis I nondisjunction – happens when homologous chromosomes (tetrads) not separate during anaphase I. Both chromosomes move toward same pole.
- The gametes formed all abnormal: two with extra chromosome (n+1) and two with missing one (n−1).
- This type is very common in maternal oocytes, especially with aging.
- Meiosis II nondisjunction – occurs when sister chromatids fail to separate during anaphase II stage.
- It makes four gametes: two normal (n), one with n+1, and one with n−1 chromosomes.
- This type generally less frequent but still cause disorders like Down’s syndrome or Turner’s sometimes.
- Mitotic nondisjunction – observed in somatic cells, not in gametes.
- During mitosis, sister chromatids are not pulled apart evenly, producing one cell with 2n+1 and another with 2n−1.
- This result cause somatic mosaicism, where only some cells in body show abnormal number.
- It may also contribute by cancer cell formation (example: retinoblastoma).
Causes of Nondisjunction
- Nondisjunction happens when chromosomes fail to separate properly during cell division (meiosis or mitosis).
- The main cause is usually fault in spindle fibers, they not attach rightly with centromere of chromosomes.
- Sometimes, the homologous chromosomes are not pulled apart in meiosis I, that leads to whole pair going in one daughter cell.
- In meiosis II, when sister chromatids not divide correctly, it also cause nondisjunction.
- Age is also big factor — as the oocyte become older, the spindle formation get weaker, so error chances rise.
- Errors may occur by improper crossing-over; when recombination happen at wrong place or not at all, chromosomes get sticked abnormally.
- Presence of mutations in spindle check proteins (like MAD2, BUB1) disturb the checkpoint, and division proceed wrongly.
- Exposure by some chemicals/radiations also damage microtubule structure or DNA, so the chromosomes can’t separate fine.
- Some researchers think delayed anaphase movement of one chromosome also result in nondisjunction because of time lag.
- When cohesin proteins that hold chromatids together break too early/too late, the whole segregation mess up badly.
- In few cases, environmental stress during gametogenesis (temperature shock, toxins etc.) disturb spindle orientation, giving rise to abnormal gametes.
Molecular Biology of Nondisjunction
- Nondisjunction on a molecular level is a consequence arising from a dysfunctional spindle assembly checkpoint (SAC), which normally halts the cell cycle when there are improperly attached chromosomes. However, in this case, the cell cycle continues as if everything were fine.
- Among the factors that most frequently cause attachment errors of microtubules to the kinetochore are, for instance, formation of syntelic or monotelic attachments and subsequent mis-segregation of chromosomes.
- The cohesin complex that glues the sister chromatids together is also the source of the correct tension, so if cohesin is depleted or lost at an early stage one can expect segregation faults to follow.
- Separase (the protease) has to cut cohesin at the right moment. In the event that separase is inhibited or activated at the wrong time, chromatids will be left together and NDJ will take place.
- Both condensin and topoisomerase II are responsible for decatenating DNA, thus if they are malfunctioning physical intertwining of chromatids remains and pulling them apart is not possible.
- There is a possibility that the anaphase-promoting complex (APC/C) gets activated prematurely, securin is removed quickly, separase is liberated too early — in this way chromosomes become disordered.
- Checkpoint proteins such as MAD2, BUB1, BUBR1 can suffer mutations or reduced expression, thus being associated with weakened checkpoint which can be detected in some cells and consequently NDJ is facilitated.
- The main factor for non-disjunction in meiosis is abnormal recombination (crossing-over). Either lack of crossovers or wrongly placed crossover near telomere/centromere leads to changed alignment and mis-segregation of entire homologs or sister chromatids.
- The source of errors in the aging oocytes is the loss of cohesion and instability of the spindle, maintenance proteins gradually lose their function over decades, thus errors accumulate with maternal age.
- It has been experimentally observed that chemical agents or drugs (colchicine, certain pesticides, benzene-like exposures) that disrupt microtubules or checkpoints lead to the production of aneuploid gametes.
- Slow or delayed anaphase movement due to DNA damage or unresolved catenations after replication give rise to nondisjunction as a result of timing mismatch, the process continues but out of synchronization.
- There are scenarios when the SAC signal gets overridden, or the kinetochore attachment is not recognized correctly, hence the safeguard is bypassed — a train leaving the station early, you might say, and derailment is the result.
- The timing of cohesin cleavage is the most important thing; if cleavage is too early or too late, segregation is incorrect, meiosis I vs II errors depend on the particular stage at which cohesion was lost.
- The molecular consequence is aneuploid cells (trisomy, monosomy), and the cells in question come about as a result of failure of the mechanical/regulatory parts — proteins, attachments, timing all working together.
Consequences of Nondisjunction
The nondisjunction is the failure when chromosomes don’t separate properly during cell division (like meiosis/mitosis), causing abnormal number of chromosomes in daughter cells. Such imbalance is termed as aneuploidy, sometimes loss of one (monosomy 2n–1) or gain of one (trisomy 2n+1) chromosome happen.
Around 15–20 % of human pregnancies ends by spontaneous abortion, and half or more are aneuploid ones. It show that this condition very fatal for early embryos.Most embryos don’t reach birth, but few, like Down’s, Turner’s, and Klinefelter’s, somehow live — though with developmental defects etc.
I. Chromosomal Disorders (Aneuploidy)
- During meiosis, when homologous or sister chromatids not pulled apart, abnormal gametes form. After fertilization those gametes give a zygote with extra or missing chromosome — disorder starts there.
- These disorders grouped as autosomal aneuploidy and sex chromosome aneuploidy, depending where the error lies.
A. Autosomal Aneuploidies – (Trisomies)
- Down Syndrome (Trisomy 21) – presence of an extra 21st chromosome.
- It’s the most frequent viable aneuploidy seen in humans.
- Signs: flattened face, upward eyes, poor muscle tone, delayed mind growth, heart defect.
- Usually result by nondisjunction in maternal meiosis I.
- Later, risk for Alzheimer’s disease / leukemia is high.
- Edwards Syndrome (Trisomy 18) – an extra chromosome 18 appears.
- Growth deficiency, small head (microcephaly), clenched fists with overlapped fingers, skeletal & heart defects.
- About 95 % don’t survive till birth, and only 5–10 % live for near one year.
- Patau Syndrome (Trisomy 13) – one more copy of chromosome 13.
- Shows severe mental retardation, small eyes, cleft lip or palate, heart defects, and extra fingers/toes (polydactyly).
- Mortality very high; most babies die inside first week (avg. 7 days).
- Other full trisomies mostly non-viable; they cause miscarriage, no living child seen.
B. Sex Chromosome Aneuploidies
- Klinefelter Syndrome (47, XXY) – found in males; one extra X chromosome.
- Most common sex chromosomal abnormality.
- Cause infertility / small testes, long arms–legs, some have gynecomastia (~1/3 cases).
- Mostly result from paternal nondisjunction in meiosis I.
- Turner Syndrome (45, X or X0) – female have only one X chromosome.
- Only monosomy that can survive to birth.
- Short stature, webbed neck, kidney defect (horseshoe type), heart malformation, infertility.
- 99 % of such embryos lost by spontaneous abortion.
- Triple X (47, XXX) – extra X in female. Many look normal, sometimes taller, or mild learning issues, irregular cycles.
- XYY Male (47, XYY) – male with extra Y; mostly normal but taller than normal average, some learning problem maybe.
II. Non-Aneuploid / Somatic Results
- If nondisjunction happens during mitosis, then only part of organism’s cells get abnormal chromosome number — called somatic mosaicism.
- So body become mix of cell lines: some normal (2n), some abnormal (2n ± 1). Mosaic cases seen in Down’s or Turner type disorders.
- Mitotic nondisjunction also related with cancer formation, by loss of tumor-suppressor gene like RB1 (chromosome 13) in retinoblastoma – this “second hit” event cause tumor formation.
- The chromosomal instability (CIN) produced by such errors often noticed in malignant tissues; it make cells unstable and abnormal in growth pattern.
- Sometimes, when trisomic conceptus lose one chromosome, both left copies may come from same parent — this strange event called uniparental disomy (UPD).
- UPD in chromosome 15 connected with Prader-Willi and Angelman syndromes.
III. Fate of Abnormal Gametes
- In meiosis I failure, homologous chromosomes not separate, all gametes abnormal — two (n + 1) and two (n − 1).
- In meiosis II, only half gametes defective (1 n + 1, 1 n − 1, rest normal).
- In mitosis, when sister chromatids not pulled apart, two daughter cells form: one with 47 and one with 45 chromosomes.
Risk Factors of Nondisjunction
Nondisjunction (NDJ) happen when chromosomes or sister chromatids fail to split correctly in cell division.
Risk factors are mainly grouped as Age-related, Genetic/Molecular, Environmental, and Chromosomal structure related things.
I. Age Related Risk Factors
- Advanced Maternal Age – most known factor for meiotic NDJ, especially for autosomal trisomies like Trisomy 21.
- The older the mother, the higher the risk — ex: 1 in 1,250 at age 25 → around 1 in 100 at 40 → nearly 1 in 12 by 49 yrs.
- Almost 90 % of all aneuploidies come from the mother’s side, and about 70 % of those caused by errors in Meiosis I.
- The main molecular reason is that oocytes stay arrested too long in Prophase I, sometimes decades — this aging cause weak chromatid connection.
- Cohesin proteins get degraded slowly, so chromatids no longer hold tightly, and chiasmata (crossovers) are lost.
- Also, spindle machinery weaken with age; the SAC (Spindle Assembly Checkpoint) doesn’t work properly, so wrong segregation passes unnoticed.
- Paternal age effect is smaller but still there, about 8 % of Trisomy 21 comes from father’s side.
- Half of Klinefelter (XXY) cases are maternal, rest from paternal Meiosis I errors. Older men have longer spermatogenesis cycles, giving more pairing mistakes.
II. Genetic / Molecular Risk Factors
- The most crucial molecular trigger is abnormal recombination or failure in regulatory proteins.
- When recombination pattern on chromosome 21q gets abnormal, risk of segregation mistake rise a lot.
- No recombination (non-exchange) or crossover too far at telomeric ends → increase Meiosis I NDJ, and it doesn’t depend on age.
- But when crossover happens too near centromere, then Meiosis II errors go high.
- Specific gene variants, like MCM9 (Mini-chromosome maintenance 9) polymorphism, connected with higher NDJ risk.
- That gene affect recombination and DNA repair; risk variants may cause wrong splicing or less stable protein → oocytes suffer imbalance in MCM9 levels.
- Defects also seen in cell-cycle controls. SAC failure, poor attachment, or inactive segregation enzymes cause both meiotic and mitotic NDJ.
- Example: inactivation of topoisomerase II, condensin, or separase enzymes lead to abnormal separation.
- Wrong spindle links—like monotelic (only one side attached) or syntelic (both attached to same pole)—also cause mis-segregation mainly in Meiosis I.
III. Environmental / Lifestyle Risk Factors
- Many chemical/physical exposures work as aneugens, increasing NDJ frequency.
- Cigarette smoke and ethanol (alcohol) are known causes in lab animals, possibly same in humans too.
- Long exposure to benzene, insecticides like fenvalerate / carbaryl linked to more aneuploid gametes.
- Physical reasons also exist – ionizing radiation (like from Chernobyl fallout) increases number of Trisomy 21 births.
- UV rays damage DNA and may disturb segregation mechanism.
- Nutrient deficiency, esp. folic acid lack, also linked to NDJ seen in cultured human cells.
IV. Structural Chromosomal Risk Factors
- People carrying balanced translocations (for ex. Robertsonian types in chr. 13, 14, 15, 21, 22) have higher NDJ risk.
- They look normal but during meiosis, the rearranged chromosomes don’t pair or separate properly → make unbalanced gametes.
- Such event produce translocation Down Syndrome in offspring when extra chromosome piece inherited.
- Male Robertsonian carriers often show higher aneuploidy in sperm count compared to normal males.
Nondisjunction Examples
The nondisjunction mostly seen in few known syndromes, each having their own abnormal story of chromosome numbers. It happens because chromosomes don’t split when they should, the result, cells get too many / too less of them.
- Down’s Syndrome (Trisomy 21) – One extra chromosome 21 found (so total 47).
- This is the most common and somehow survivable aneuploidy.
- Most time the error come from maternal meiosis I, during egg formation.
- Face becomes flat, tongue big, heart defects common. Growth slow and mental delay usual thing.
- Risk jumps crazy fast with mother’s age – 25 yrs (1/1250), 40 yrs (1/100).
- Edwards Syndrome (Trisomy 18) – The cell carry one extra 18th chromosome.
- Babies very small, weak cry, clenched fists (with fingers overlap weirdly).
- Head tiny, heart and organ problems also, most die before 1 year, actually 95% not even born alive.
- The nondisjunction happens usually by meiosis II, maternal side again.
- Patau’s Syndrome (Trisomy 13) – here the 13th chromosome got an extra copy.
- Cleft lip/palate, extra fingers/toes, very small eyes, brain and heart both malformed.
- Mortality nearly total, average life just about a week, it’s heartbreaking.
- The NDJ error mostly maternal, rarely paternal.
- Klinefelter (47, XXY) – male born with one extra X chromosome.
- Body tall and slim, voice high pitch sometimes, gynecomastia (breast like structure).
- Infertility very common. Many don’t realize until adulthood.
- Half the cases by paternal nondisjunction, during meiosis I.
- Turner’s Syndrome (45, X or X0) – a female got only one X chromosome, no second sex chromosome.
- Short stature, wide chest, webbed neck, missing menstruation and sterile mostly.
- The monosomy only one that can live, but 99% of embryos lost before birth.
- Sometimes, mosaic form survive better if some cells have 46,XX.
- Triple X (47, XXX) – a woman have one extra X, but it’s subtle condition.
- Often tall, some learning difficulty, sometimes no signs at all.
- Usually discovered accidentally in genetic test.
- Error can happen both in meiosis I or II, maternal mostly.
- XYY Male (47, XYY) – extra Y in male, also caused by paternal nondisjunction.
- Taller than average, few may show mild behavioral issue or learning problem.
- They usually normal fertility and physical look.
- Mosaic Down Syndrome – nondisjunction after fertilization (during mitosis).
- So person have mix of normal cells (46) and trisomic cells (47).
- The more abnormal cells, the stronger the features appear.
- Uniparental Disomy (UPD) – an odd outcome when trisomic zygote “fix itself” by losing one chromosome.
- Then both left copies come from same parent, not one from each.
- Ex: Prader–Willi or Angelman syndromes (chromosome 15) depend which parent gave both.
- Cancer-related NDJ – not all NDJ about birth defects, sometimes it happen later.
- In somatic cells, like in retinoblastoma, RB1 gene (chr 13) lost by NDJ, removing tumor suppression.
- That’s “second hit” mechanism, and then the cancer cell just keep dividing unstoppably.
- Chromosomal instability (CIN) becomes visible, the cells look weird under microscope.
- Some NDJ also seen in plants and fungi etc., but human ones studied more, since consequences are serious and visible.
Clinical Significance of Nondisjunction
The nondisjunction (NDJ) have deep clinical meaning since it cause wrong chromosome number, that change whole phenotype of a person, sometimes even viability of embryo itself.
In humans, NDJ mainly cause aneuploidy, either gain or loss of chromosome. That condition leads to developmental disorders or spontaneous abortions etc.
Almost 50–60 % of miscarried fetuses found to be aneuploid — it means this error very common but mostly incompatible with life.
When it not fatal, NDJ still produce multiple clinical syndromes which survive, like Down, Turner, Klinefelter, Patau, and Edwards syndromes.
- Down Syndrome (Trisomy 21) – most frequent viable NDJ disorder.
- Intellectual delay, facial flattening, congenital heart defects seen.
- Risk increase sharply with maternal age.
- Patients live into adulthood but show higher risk of Alzheimer’s and leukemia.
- Turner Syndrome (45, X) – occurs in females missing one X.
- Short stature, webbed neck, infertility, and cardiovascular defects common.
- Ovarian dysgenesis leads to absent puberty; often diagnosed during teenage years.
- Klinefelter (47, XXY) – in males; they often tall and sterile, with low testosterone.
- Sometimes gynecomastia develops, and cognitive/social delay may appear.
- Edwards (Trisomy 18) and Patau (Trisomy 13) – both usually lethal; newborns seldom survive beyond few weeks.
- Severe brain/heart malformations occur, thus mostly fatal outcome.
- NDJ can occur also in somatic cells — making mosaicism, where only certain tissues have abnormal chromosome count.
- Example: Mosaic Down Syndrome show milder signs because only some cells affected.
- In cancer, NDJ play critical role by promoting chromosomal instability (CIN).
- When tumor-suppressor genes like RB1 lose one copy by NDJ (so-called “second hit”), uncontrolled cell division begins.
- Seen in retinoblastoma, also other malignancies like colon and breast cancers show CIN.
- NDJ also contributes to uniparental disomy (UPD), which can trigger imprinting disorders.
- For example, chromosome 15 UPD cause either Prader-Willi or Angelman syndrome, depending which parent both chromosomes came from.
Clinically, NDJ screening important for prenatal diagnosis — tests like amniocentesis, chorionic villus sampling (CVS), or NIPT (non-invasive prenatal testing) detect abnormal chromosome number early.
Proper understanding of NDJ mechanism help in genetic counseling, especially for older women, families with previous trisomy child, or known translocation carriers.
Thus, significance of NDJ is both diagnostic and prognostic – it tell risk, explain etiology, and guide prevention or care in next pregnancy.
- Forejt, J. (2001). Nondisjunction. Encyclopedia of Genetics, 1345–1347. doi:10.1006/rwgn.2001.0903
- Gottlieb SF, Tupper C, Kerndt CC, et al. Genetics, Nondisjunction. [Updated 2023 Aug 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482240/
- https://www.expii.com/t/nondisjunction-definition-overview-10190
- https://byjus.com/neet/nondisjunction/
- https://www.thoughtco.com/nondisjunction-definition-and-examples-4783773
- https://old-ib.bioninja.com.au/standard-level/topic-3-genetics/33-meiosis/non-disjunction.html
- https://www.expii.com/t/nondisjunction-in-meiosis-overview-impact-on-cells-10166
- https://www.vocabulary.com/dictionary/nondisjunction
- http://basicgenetics.ansci.cornell.edu/nondisjunction.php?section=sex
- https://www.jove.com/science-education/12075/nondisjunction-of-chromosomes-and-aneuploidy
- https://slcc.pressbooks.pub/collegebiology1/chapter/nondisjunction/
- https://www.savemyexams.com/dp/biology_hl/ib/16/revision-notes/3-genetics/3-2-meiosis/3-2-4-non-disjunction/