What is Neisseria gonorrhoeae?
- Neisseria gonorrhoeae is a Gram-negative diplococcus bacterium that is an obligate human pathogen, meaning it can only infect humans. It was first isolated by Albert Neisser in 1879 and is responsible for gonorrhea, one of the most prevalent sexually transmitted infections (STIs) globally. While it primarily infects the urogenital tract, it can also colonize the mucosal surfaces of the rectum, pharynx, nose, and conjunctiva, leading to a range of gonococcal diseases.
- The bacterium is microaerophilic, meaning it thrives in low-oxygen environments, and it produces oxidase. It has evolved mechanisms to evade the immune system, particularly through antigenic variation, where its pili and surface proteins undergo genetic recombination. This variation enables it to resist immune attacks, making reinfection possible even after an individual has recovered from a previous infection. N. gonorrhoeae also has the ability to survive phagocytosis by immune cells, growing inside neutrophils and contributing to its persistence in the host.
- Transmission of N. gonorrhoeae occurs primarily through sexual contact, including vaginal, anal, and oral intercourse. It can also be transmitted perinatally during childbirth, potentially causing ophthalmia neonatorum in newborns. However, perinatal transmission can be prevented by administering antibiotics to the mother and using antibiotic eye drops on the newborn. Asymptomatic infections are common in both males and females, which complicates diagnosis and increases the risk of transmission. If left untreated, the infection can spread to other parts of the body, leading to disseminated gonococcal infections, septic arthritis, or pelvic inflammatory disease (PID), which can cause infertility in women.
- The diagnosis of gonorrhea is typically made through a variety of methods, including bacterial culture, Gram staining, and nucleic acid amplification tests such as polymerase chain reaction (PCR). Testing for other STIs is often recommended due to the high rate of co-infections, particularly with Chlamydia trachomatis.
- Treatment of gonorrhea has become increasingly challenging due to the development of antibiotic resistance. N. gonorrhoeae has shown a remarkable ability to adapt to antimicrobial treatments, making previously effective drugs obsolete. In recent years, resistance to ceftriaxone, a key treatment, has been observed in some strains, raising concerns about the future management of gonorrhea. Therefore, constant monitoring of antimicrobial resistance patterns and the development of new treatment options remain critical in controlling the spread of this infection.
Morphology of Neisseria gonorrhoeae
Neisseria gonorrhoeae is a Gram-negative bacterium that presents a distinctive morphology. It exhibits unique structural features that help in its identification and understanding of its pathogenic mechanisms.
- Gram-Negative and Aerobic: N. gonorrhoeae is a Gram-negative bacterium, which means it does not retain the crystal violet stain used in Gram staining, appearing pink under a microscope. It requires oxygen to grow, making it aerobic in nature.
- Shape and Arrangement: The bacterium is spherical in shape, measuring around 0.6 to 1.0 micrometers in diameter. It typically forms pairs, with each cell displaying a characteristic coffee bean shape. The concave sides of adjacent cocci face each other, a defining feature of its morphology.
- Intracellular Presence: A notable characteristic of N. gonorrhoeae is its intracellular location. The bacteria are often found within polymorphonuclear leukocytes (PMNs), a type of white blood cell, especially in infected tissues. Smears of pus samples commonly reveal these intracellular cocci, sometimes numbering in the hundreds within a single leukocyte.
- Fimbriae and Pili: The bacterium has pili, which are hair-like appendages on its surface. These pili are involved in attachment to host tissues and play a role in twitching motility, a form of bacterial movement. Additionally, the bacteria possess fimbriae, which aid in adhesion to surfaces, contributing to its virulence.
- Non-Motile: Despite having pili that assist in movement, N. gonorrhoeae is non-motile in the traditional sense, meaning it cannot propel itself actively like some other bacteria.
- Capsule and Spores: Freshly isolated strains of N. gonorrhoeae may possess a capsule, which can help the bacterium evade immune responses. However, it does not form endospores, a feature found in some other bacterial species that aids in surviving harsh conditions.
- Lipooligosaccharide (LOS): The bacterium’s outer membrane contains a lipooligosaccharide (LOS), which has a highly branched basal oligosaccharide structure. This structure is important for the bacterium’s interactions with the immune system and its ability to evade host defenses.
These structural features give N. gonorrhoeae the tools it needs to infect and persist in the human body, leading to the development of gonorrhea and other related diseases.
Habitat of Neisseria gonorrhoeae
Neisseria gonorrhoeae is an obligate human pathogen, meaning humans are its only natural host. This bacterium thrives in specific areas of the human body, particularly in mucosal surfaces, where it can cause infections.
- Urogenital Tract: N. gonorrhoeae primarily colonizes the human urogenital tract, making it the main site for infection. It is the causative agent of gonorrhea, which typically affects the urethra, cervix, and other parts of the reproductive system.
- Rectal Carriage: While the urogenital tract is its primary habitat, N. gonorrhoeae can also be present in the rectum of healthy individuals, even in the absence of symptoms. This can occur due to sexual contact, particularly through anal intercourse.
- Intracellular Habitat: The bacterium is often found intracellularly, particularly within polymorphonuclear leukocytes (PMNs). These are a type of white blood cell with irregularly shaped nuclei. The bacteria can survive and multiply inside these cells, evading the immune system and complicating diagnosis.
- Pus Cells: When infections occur, the bacteria are commonly detected in pus cells. These cells are a mixture of dead cells, bacteria, and immune cells that form during infection. The gonococci appear inside these cells, typically arranged in pairs, with each bacterium resembling a kidney bean shape.
Culture Characteristics and Biochemical Reactions of Neisseria gonorrhoeae
Neisseria gonorrhoeae is a fastidious pathogen, meaning it requires specific growth conditions and media for successful cultivation. Here’s a breakdown of the critical culture characteristics and biochemical reactions that help identify and differentiate this bacterium.
Culture Characteristics
- Growth Requirements
- N. gonorrhoeae thrives on enriched media, such as blood agar and chocolate agar. It cannot grow on basic media like nutrient agar or Mueller-Hinton agar.
- It grows well in aerobic conditions but can also survive anaerobically.
- The bacterium prefers a temperature range of 35–36°C for optimal growth. It does not grow effectively at temperatures below 25°C or above 37°C.
- The growth is enhanced in a humid atmosphere supplemented with 5–10% CO2.
- Blood Agar
- When cultured on blood agar, N. gonorrhoeae forms small, convex colonies around 0.6 to 1.4 mm in diameter after 24 hours.
- The colonies are translucent, with entire edges and a finely granular surface.
- The colonies are soft and easily emulsifiable.
- Fatty acids and trace metals in the blood agar can inhibit gonococcal growth, but adding soluble starch neutralizes these inhibitory effects.
- Selective Media
- Thayer-Martin medium (chocolate agar with antibiotics like colistin, nystatin, and vancomycin) and modified New York City medium (a translucent medium with vancomycin, colistin, trimethoprim, and either nystatin or amphotericin B) are used to isolate N. gonorrhoeae from clinical samples containing mixed microbial flora.
- These selective media suppress the growth of contaminating bacteria, including commensal Neisseria species.
- On these media, gonococci produce small, translucent, convex colonies that are soft and friable.
- Four colony types have been identified:
- T1 and T2: Small and brown-pigmented colonies. These strains possess pili, are virulent, and are associated with acute gonorrhea.
- T3 and T4: Large, non-pigmented colonies. These strains lack pili and are avirulent.
- Transport Medium
- For transporting clinical samples, Stuart’s transport medium is commonly used to preserve the viability of N. gonorrhoeae during collection and transit.
Biochemical Reactions
- Carbohydrate Fermentation
- N. gonorrhoeae ferments glucose, producing acid without gas formation.
- It does not ferment other sugars like maltose, lactose, sucrose, or fructose. This is a key differentiator between N. gonorrhoeae and N. meningitidis, as the latter ferments both glucose and maltose.
- Nitrate Reduction and Hydrogen Sulfide Production
- N. gonorrhoeae does not reduce nitrates nor does it produce hydrogen sulfide.
- Oxidase and Catalase Reactions
- N. gonorrhoeae is oxidase positive and catalase positive, which helps in the differentiation of this species from other pathogens.
Genome of Neisseria gonorrhoeae
The genome of Neisseria gonorrhoeae is compact and efficient, playing a crucial role in its survival and pathogenicity. It consists of a single, circular DNA molecule that carries all the genetic information necessary for the bacterium to thrive.
- Genome Structure: N. gonorrhoeae’s genome is composed of a single circular DNA molecule, a common feature in many bacteria. This structure allows for efficient replication and expression of genes.
- Genome Size: The total genome length is approximately 2,153,922 nucleotides (nt). This relatively small size reflects the bacterium’s streamlined genetic material, with just enough genes to support its complex life cycle.
- Gene Content: There are 2069 genes within the genome, of which 2002 are protein-encoding genes. These genes encode the proteins necessary for the bacterium’s metabolic functions, immune evasion, and pathogenesis.
- RNA Elements: In addition to protein-coding genes, the genome also contains 67 structural RNAs, which play key roles in gene expression and cellular functions.
- G+C Content: The guanine-cytosine (G+C) content of N. gonorrhoeae’s genome is around 52.4%, which influences the stability and structure of the DNA.
- Surface Proteins: One of the important features encoded by the genome is the Opa protein, a surface protein that aids in adhesion to host cells and contributes to the bacterium’s ability to interact with the immune system.
These genomic characteristics provide N. gonorrhoeae with the necessary tools to infect human tissues, evade immune responses, and adapt to changing environments.
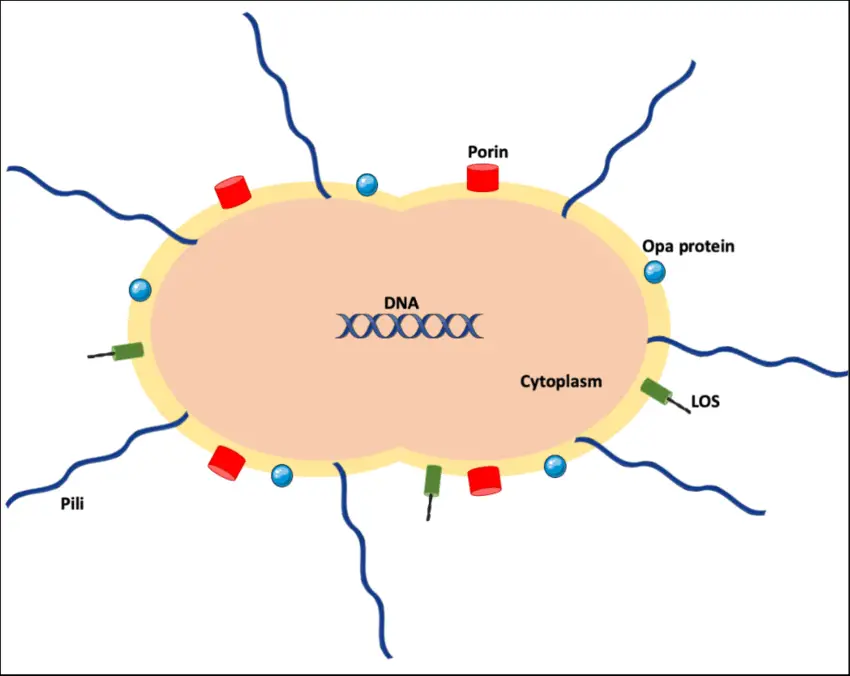
Virulence Factors of Neisseria gonorrhoeae
Neisseria gonorrhoeae relies on a variety of virulence factors to establish infection and evade the immune system. These factors allow it to survive in the human host, causing symptoms and complications associated with gonorrhea and other related diseases.
- Capsule
- Unlike Neisseria meningitidis, N. gonorrhoeae doesn’t form a typical carbohydrate capsule.
- It forms a polyphosphate capsule, which is loosely attached to its surface.
- This capsule acts as an antiphagocytic barrier, preventing the bacteria from being ingested and killed by immune cells like neutrophils.
- Pili
- Pili are hair-like structures extending from the bacterial membrane.
- They consist of pilin proteins that form repeating subunits.
- Pili are critical for the attachment of gonococci to nonciliated epithelial cells—an essential first step in establishing infection.
- They also help prevent the ingestion and destruction of the bacteria by neutrophils.
- The pili exhibit antigenic variation, which means their surface proteins can change to avoid immune detection. There are over 100 serotypes due to this variation.
- Por Proteins
- Por proteins are outer membrane proteins that help the bacteria resist serum killing.
- They achieve this by blocking the fusion of the phagolysosome in neutrophils, allowing gonococci to survive inside immune cells.
- Opa Proteins
- Opa proteins mediate bacterial adherence not only to eukaryotic cells but also to each other.
- This enables gonococci to form colonies and maintain an infection by sticking to the surfaces of host cells.
- Rmp Proteins
- Rmp proteins create antibodies that hinder the serum bactericidal activity against gonococci.
- By blocking immune defenses, Rmp proteins help the bacteria evade the host’s immune system.
- Lipo-oligosaccharide (LOS)
- The Lipo-oligosaccharide on the surface of N. gonorrhoeae possesses endotoxic activity, contributing to the inflammation and tissue damage seen during infection.
- IgA Protease
- IgA protease is an enzyme produced by gonococci to destroy IgA, an important antibody in mucosal immunity.
- By targeting IgA, the bacteria impair the host’s immune response at mucosal surfaces, aiding in gonococcal persistence.
- Beta-lactamase
- Beta-lactamase is an enzyme that degrades beta-lactam antibiotics like penicillin.
- This enzyme allows gonococci to resist the effects of these commonly used antibiotics, making treatment more challenging.
- Plasmids
- Plasmids in gonococci can carry antimicrobial resistance genes, contributing to resistance against various antibiotics.
- These plasmid-borne virulence factors allow the bacteria to survive in the face of antibiotic pressure, leading to treatment failures.
Cell Wall Components and Antigenic Properties of Neisseria gonorrhoeae
Neisseria gonorrhoeae has a complex cell wall structure typical of Gram-negative bacteria, consisting of several key components. These components not only serve structural functions but also play a role in the bacterium’s ability to evade the immune system and cause disease. The cell wall contains specific proteins that contribute to antigenic variability and immune evasion.
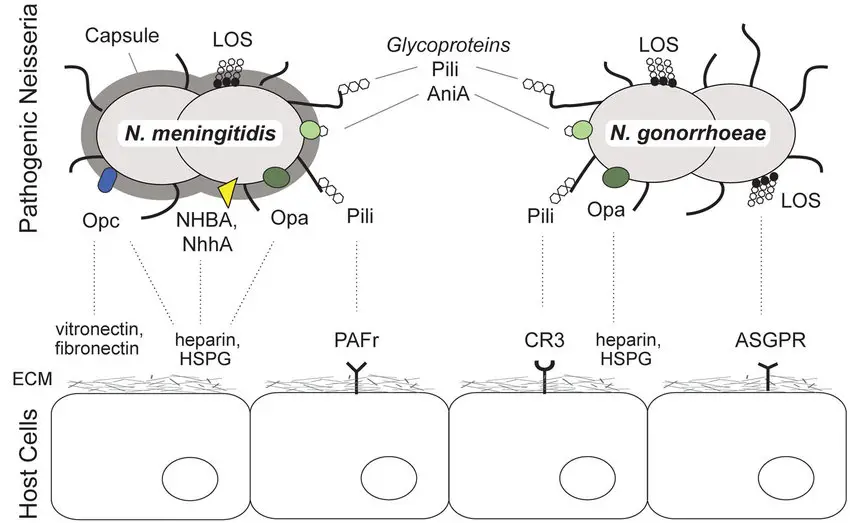
Outer Membrane Proteins (OMPs)
The outer membrane of N. gonorrhoeae contains several important proteins that aid in its survival and virulence:
- Por Proteins
- The Por proteins (also known as protein I) are porin proteins that create pores or channels in the outer membrane, allowing the bacteria to take up essential nutrients like iron.
- There are two main types: Por-A and Por-B. Each type has different antigenic variations that are crucial for serotype classification.
- Por-A is typically linked to disseminated gonococcal disease, as it helps the bacteria resist killing by serum complement components. This resistance enables the bacteria to survive longer in the bloodstream.
- Opa Proteins
- Opa proteins, previously known as protein II, are membrane proteins that help N. gonorrhoeae adhere to both other bacteria and eukaryotic cells.
- These proteins contribute to the formation of opaque colonies in culture, making them a distinct feature for identification.
- Rmp Proteins
- Rmp proteins, formerly known as protein III, are involved in immune evasion. They induce the production of antibodies that block the serum bactericidal activity against the bacteria, allowing the gonococci to survive in the bloodstream.
Other Key Cell Wall Components
- Lipo-Oligosaccharide (LOS)
- LOS is another crucial antigen found in the outer membrane of N. gonorrhoeae. It is composed of lipid A and an oligosaccharide, similar to the lipopolysaccharide (LPS) of other Gram-negative bacteria.
- However, unlike LPS, LOS does not exhibit antigenic variation.
- LOS plays a role in the endotoxic activity of the bacterium, contributing to the inflammatory response during infection.
- IgA1 Protease
- IgA1 protease is an enzyme produced by N. gonorrhoeae that specifically targets and degrades secretory IgA1. This immunoglobulin is found in mucosal areas like the urogenital tract, where it plays a key role in defending against bacterial pathogens.
- By degrading IgA1, the bacteria are able to bypass a major line of immune defense.
- Beta-Lactamase
- Beta-lactamase is an enzyme that breaks down the beta-lactam rings of penicillin, rendering the antibiotic ineffective.
- This allows N. gonorrhoeae to resist treatment with penicillin, one of the traditional antibiotics used to treat gonorrhea.
Together, these cell wall components and antigenic properties make N. gonorrhoeae a highly adaptable and virulent pathogen capable of evading the host immune system and surviving under various conditions. The antigenic variation in its proteins, such as the Por and Opa proteins, also contributes to the challenge of developing long-lasting immunity or effective vaccines.
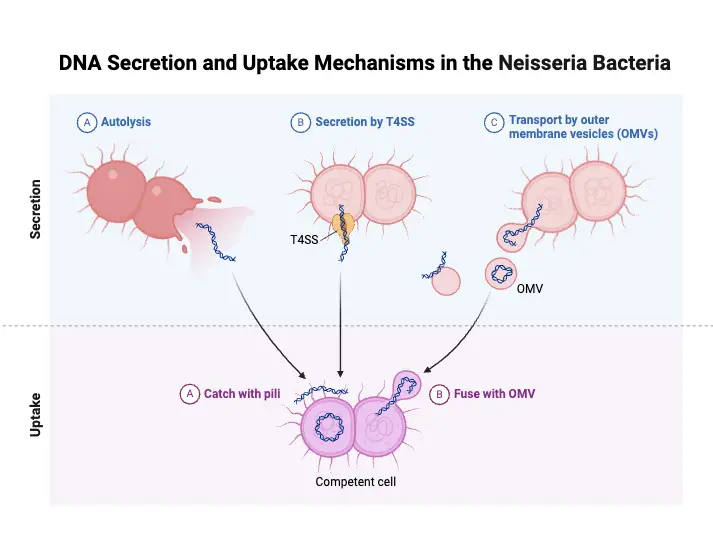
Pathogenesis of Neisseria gonorrhoeae
Neisseria gonorrhoeae is a strict human pathogen that primarily infects superficial mucosal surfaces, such as those in the urethra, rectum, cervix, pharynx, and conjunctiva. The bacterium uses specialized structures and mechanisms to adhere, invade, and survive in these tissues, establishing infection.
- Adhesion to Mucosal Surfaces
- The gonococcus relies on pili and Opa proteins for adhesion to the columnar epithelial cells lining mucosal surfaces.
- Pili, hair-like appendages, are critical for:
- Attachment to the mucosal cells.
- Facilitating genetic exchange between strains.
- Opa proteins also play a key role in tight binding to host cells, enabling colonization at the site of infection.
- Penetration and Evasion
- After adhesion, Pili, PorB, and Opa proteins work together to:
- Penetrate host cells.
- Multiply within the epithelial cells.
- Translocate through the cells into the subepithelial space, where infection is further established.
- This process allows gonococci to escape immune detection and persist in the host.
- After adhesion, Pili, PorB, and Opa proteins work together to:
- Inflammatory Response
- Gonococcal lipooligosaccharide (LOS) plays a crucial role in triggering inflammation.
- LOS stimulates the release of tumor necrosis factor-α (TNF-α), a key proinflammatory cytokine that is responsible for many of the symptoms seen in gonococcal infections, such as pain and swelling.
- Antibodies to LOS can activate the complement system, particularly releasing C5a, which attracts neutrophils to the site of infection, contributing to the inflammatory response.
- Immune Evasion
- Gonococci have evolved mechanisms to evade immune defenses. For example:
- IgG and secretory IgA1 antibodies, which are crucial for neutralizing infections, can be blocked by Rmp proteins.
- This interference prevents the body’s immune system from mounting an effective bactericidal response.
- Gonococci have evolved mechanisms to evade immune defenses. For example:
- Iron Acquisition
- For survival and growth within the host, gonococci require iron, a nutrient that is tightly regulated by the human body.
- The bacteria express specific transport systems to acquire iron by scavenging it from human iron-binding proteins such as transferrin, lactoferrin, and hemoglobin.
- This ability to extract iron is vital for the bacteria’s pathogenicity and persistence in vivo.
These pathogenic mechanisms allow Neisseria gonorrhoeae to successfully colonize the mucosal surfaces, evade the immune response, and cause inflammation, all of which contribute to the symptoms and progression of gonorrhea.
Clinical Syndromes of Neisseria gonorrhoeae
Neisseria gonorrhoeae causes a variety of clinical syndromes, from localized genital infections to more severe, disseminated diseases. The major syndromes include gonorrhea, disseminated gonococcal infections (DGI), ophthalmia neonatorum, and several other gonococcal-related conditions.
- Gonorrhea
- Gonorrhea is primarily a sexually transmitted infection, often presenting with symptoms in the genital area.
- In men, the infection usually manifests as urethritis, with symptoms like burning during urination and serous urethral discharge.
- Over time, the discharge becomes more purulent and may even turn blood-tinged.
- Complications like acute epididymitis, prostatitis, and periurethral abscess can occur, but these are rare.
- In women, gonorrhea typically affects the endocervix (80–90% of cases), as gonococci prefer to invade columnar epithelial cells.
- The infection is often asymptomatic in women, but when symptoms do appear, they include vaginal discharge, dysuria, dyspareunia, and mild lower abdominal pain.
- In 10–20% of cases, the infection can ascend from the cervix to cause more severe complications, such as salpingitis, tubo-ovarian abscess, and pelvic inflammatory disease (PID).
- PID is a major complication, leading to ectopic pregnancy, infertility, and tubal scarring.
- Gonococcal vulvovaginitis can also affect prepubertal girls through sexual contact.
- Disseminated Gonococcal Infections (DGI)
- DGI occurs when gonococci spread via the bloodstream from the primary infection site to distant body parts.
- The classic presentation is arthritis-dermatitis syndrome.
- Symptoms often include migratory polyarthralgia, primarily in the knees, elbows, and other joints, along with tenosynovitis (tendon inflammation).
- Skin lesions often appear as maculopapular or pustular rashes, sometimes with hemorrhagic components.
- As the infection progresses, septic arthritis may develop, especially in the knee. The skin lesions usually disappear by this stage, and gonococci are often not detectable in blood cultures.
- DGI is more commonly seen in untreated asymptomatic women and those with complement deficiencies.
- Ophthalmia Neonatorum
- Ophthalmia neonatorum is a serious infection caused by N. gonorrhoeae, transmitted to newborns during vaginal delivery from an infected mother.
- It presents as bilateral conjunctivitis, with pain, redness, and purulent discharge in the newborn’s eyes.
- Without prompt treatment, the infection can lead to blindness due to the rapid damage gonococci can cause to the eyes.
- The infection may also be transmitted in utero or in the postpartum period, making early detection and treatment critical.
- Other Gonococcal Infections
- Anorectal Gonorrhea and gonococcal pharyngitis often occur in homosexual men through rectal intercourse or orogenital contact, respectively.
- Pharyngitis is typically asymptomatic but can present with exudative pharyngitis and cervical lymphadenopathy.
- Purulent gonococcal conjunctivitis in adults happens when gonococci are transferred to the eyes through autoinoculation from a primary site of infection, such as the genitals.
- This condition can rapidly develop into panophthalmitis and result in loss of the eye without swift intervention.
- Acute perihepatitis (Fitz-Hugh and Curtis syndrome) can occur when N. gonorrhoeae or Chlamydia trachomatis extends from the fallopian tubes to the liver capsule and surrounding tissues.
Each of these clinical syndromes presents unique challenges, with some requiring prompt intervention to prevent serious complications like infertility, blindness, or septic arthritis. Early detection and treatment remain key to managing gonorrheal infections effectively.
Laboratory Diagnosis of Neisseria gonorrhoeae
The diagnosis of gonococcal infection primarily relies on identifying Neisseria gonorrhoeae at the infection site through various laboratory methods. Specimens are collected based on the infection location, and multiple techniques, including microscopy, culture, and antigen detection, are employed to confirm the diagnosis.
- Specimen Collection
- Genital specimens (e.g., urethral discharge in men, cervical discharge in women) are typically used for diagnosis in acute cases.
- For males, urethral discharge is collected by cleaning the meatus with saline-soaked gauze and using a platinum loop to gather the discharge. If no discharge is visible, a swab is inserted 2-3 cm into the urethra for sample collection.
- In females, the cervix is cleaned of exudate, and a swab is inserted into the external os and rotated to collect the discharge.
- Rectal samples are collected from asymptomatic women, bisexual, and homosexual men, where rectal gonorrhea may be present.
- Chronic infections may require additional samples such as urine (especially morning specimens) or prostatic massage in males to detect the infection when urethral discharge is absent.
- Microscopic Examination
- Gram stain is a key diagnostic tool. For urethritis in males, a smear of the urethral exudate is examined under oil immersion. Polymorphonuclear leukocytes (PMNs) greater than 4 per field is indicative of urethritis.
- Gram-negative intracellular diplococci are diagnostic of Neisseria gonorrhoeae in symptomatic males.
- In females, Gram stain of endocervical smears is less sensitive (50–60%) but shows PMNs in the presence of cervicitis. However, Gram stain is less reliable for diagnosing infections in anorectal gonorrhea, pharyngitis, and skin lesions due to cross-reactivity with other Neisseria species.
- Culture
- Culture is the gold standard for confirming gonococcal infections. Specimens are cultured on both non-selective media (like blood agar or chocolate agar) and selective media (such as Modified Thayer Martin medium).
- On chocolate agar, gonococci colonies appear small, translucent, round, and convex with a granular surface. Thayer Martin medium suppresses other microbial growth but can inhibit some gonococcal strains due to the vancomycin present.
- 48-hour incubation at 35–36°C with 5–10% CO2 is ideal for colony development.
- Identification
- Neisseria gonorrhoeae is identified by its unique biochemical and morphological characteristics, differentiating it from other Neisseria species like N. meningitidis.
- Tests may include oxidase testing, sugar fermentation, and specific antimicrobial susceptibility profiles.
- Antigen Detection
- The direct fluorescent antibody (DFA) test is used to detect gonococcal antigens in specimens such as urethral and endocervical discharge.
- The enzyme-immunoassay (EIA) detects gonococcal antigens as well and is commonly used for the same specimens.
- These antigen detection methods offer a faster, yet reliable, alternative to traditional culture, though their sensitivity can vary.
- Serodiagnosis
- Serological tests like ELISA and radioimmunoassays (RIA) detect gonococcal antigens or specific antibodies in the serum.
- These tests are not routinely used for diagnosis but may be employed in cases like chronic gonorrhea or gonococcal arthritis to identify systemic involvement.
Treatment of Neisseria gonorrhoeae
The treatment for Neisseria gonorrhoeae has evolved as the bacteria developed resistance to multiple drugs over time. What worked decades ago no longer serves as an effective treatment for most cases. Here’s how the landscape of gonorrhea treatment has changed and how current strategies address it.
- Penicillin Resistance
- Initially, penicillin was the go-to treatment for penicillin-sensitive N. gonorrhoeae strains.
- In the late 1950s, penicillin resistance emerged. Strains with a minimal inhibitory concentration (MIC) of 0.1 U/mL were first noted.
- Over the years, resistance escalated, with the MIC required to halt bacterial growth climbing significantly, sometimes needing 2.4–4.8 million units (MU) of penicillin.
- Most penicillin-resistant strains produce beta-lactamase, an enzyme that breaks down penicillin. This resistance is often plasmid-mediated, meaning it spreads easily between bacteria.
- Some strains do not produce beta-lactamase but still show low-level penicillin resistance, mediated through chromosomal mechanisms.
- Other Antibiotic Resistance
- Tetracycline and erythromycin resistance has also been noted due to chromosomal-mediated changes. This makes older treatments like tetracycline ineffective for gonococcal infections.
- Ciprofloxacin, a commonly used fluoroquinolone, has also seen rising resistance, especially in regions like Southeast Asia, Africa, and Australia. This highlights the shifting patterns of resistance in N. gonorrhoeae.
- As these resistances accumulate, treating gonorrhea has become more complex, demanding careful selection of antibiotics.
- Effective Treatment for Gonococcal Conjunctivitis
- Gonococcal conjunctivitis, a serious eye infection, requires immediate saline irrigation to reduce irritation and prevent further damage.
- Intravenous ceftriaxone is the recommended treatment for severe cases. Ceftriaxone is a third-generation cephalosporin with strong efficacy against resistant strains.
- For gonococcal ophthalmia neonatorum, an eye infection in newborns, the local application of 0.5% erythromycin ophthalmic ointment or alternatives like 1% tetracycline or 1% silver nitrate ointment can be used.
- Treatment of Pelvic Inflammatory Disease (PID)
- PID often involves a mix of infections, including gonococci, Chlamydia, and other facultative anaerobes.
- Due to the mixed nature of the infection, broad-spectrum antibiotics are needed. This ensures that all the organisms contributing to the infection are addressed in a single treatment course.
Prevention and Control of Neisseria gonorrhoeae
Neisseria gonorrhoeae remains a significant public health concern, especially with rising antibiotic resistance. While there’s no vaccine for gonorrhea and chemoprophylaxis is ineffective, several strategies are critical in reducing the spread and impact of the infection.
- Health Education
- Educating the public about gonorrhea, its symptoms, transmission, and prevention is crucial.
- Health education efforts should focus on safe sex practices, emphasizing the consistent use of condoms and the risks of multiple sexual partners.
- Early Detection and Diagnosis
- Identifying gonococcal infections early helps prevent further transmission and complications.
- Prompt treatment of infected individuals can stop the spread to others.
- Contact Tracing
- Once a case of gonorrhea is diagnosed, tracing sexual contacts is essential.
- Contact tracing ensures that individuals exposed to the infected person are informed and treated, preventing reinfection and wider outbreaks.
- Follow-up and Screening
- Regular screening of individuals at risk (e.g., sexually active individuals, especially those with multiple partners) helps detect infections early.
- Follow-up appointments for treated individuals ensure that the infection has been cleared and reduce the chance of reinfection or complications.
- Prevention of Gonococcal Conjunctivitis in Newborns
- Gonococcal conjunctivitis in newborns can be prevented by administering erythromycin ointment to the infant’s eyes shortly after birth.
- This prevents the infection from being transmitted during delivery, protecting the newborn from serious eye damage.
- Promotion of Safe Sex
- Encouraging safe sex practices, particularly the use of condoms, is one of the most effective measures in preventing gonorrhea.
- Safe sex campaigns are essential in reducing transmission rates, especially in areas with high incidence.
While the control of N. gonorrhoeae largely depends on these preventive measures, early detection and consistent education remain the backbone of managing its spread.
- Textbook of Microbiology and Immunology – Textbook by Parija SC
- https://en.wikipedia.org/wiki/Neisseria_gonorrhoeae
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.