What is Myocardium?
- The myocardium is a crucial component of the heart, situated as the muscular middle layer between the epicardium and endocardium. This central structure plays a vital role in the overall function of the heart, often referred to as the “mass of the heart.” The myocardium is primarily composed of two types of cells: cardiac muscle cells, also known as cardiomyocytes, and fibroblasts. These cells work in harmony to ensure the heart can effectively contract and pump blood throughout the body.
- Cardiomyocytes are specialized cells responsible for the heart’s contractile function. They exhibit unique characteristics, including the ability to generate spontaneous electrical impulses that trigger heartbeats. This intrinsic property allows the heart to maintain a rhythmic cycle, ensuring a continuous supply of oxygen-rich blood to vital organs. Meanwhile, fibroblasts play a supportive role by maintaining the structural integrity of the myocardium, producing extracellular matrix components that provide stability and resilience to the heart muscle.
- The heart itself serves as the central organ of the circulatory system, facilitating the circulation of blood. It is encased in the pericardium, a thin fibroelastic, double-layered sac filled with fluid. This protective structure consists of an outer fibrous layer, known as the parietal pericardium, and an inner serous layer, referred to as the visceral pericardium. Together, these layers safeguard the heart against external shocks and provide lubrication to reduce friction during cardiac contractions.
- The term “myocardium” derives from the Ancient Greek words “mûs,” meaning muscle, and “kardía,” meaning heart. This etymology emphasizes its essential muscular nature, highlighting its function as the powerhouse of the heart. The myocardial layer is integral not only for facilitating the heart’s pumping action but also for maintaining overall cardiovascular health.
Definition of Myocardium
The myocardium is the thick, muscular middle layer of the heart wall, located between the epicardium and endocardium. It is primarily composed of cardiac muscle cells (cardiomyocytes) that enable the heart to contract and pump blood throughout the body.
Layers in the Walls of the Heart
The heart, a muscular organ, plays a crucial role in pumping blood throughout the body through rhythmic contractions. Its structure consists of three distinct layers, each with specific functions and characteristics. Understanding these layers is essential for comprehending how the heart operates effectively.
- Epicardium:
- This layer serves as the outermost boundary of the heart wall.
- It comprises mesothelial cells, which are flat epithelial cells that provide a protective covering.
- Beneath these mesothelial cells are connective and adipose tissues, which help cushion and support the heart.
- The epicardium also functions as the visceral layer of the serous pericardium, which surrounds the heart.
- Within this layer, important structures such as coronary arteries and veins, lymphatic vessels, and nerves are present, contributing to the heart’s blood supply and innervation.
- Myocardium:
- The myocardium is the thick, muscular middle layer of the heart, constituting approximately 95% of the mass of cardiomyocytes.
- This layer is primarily responsible for the heart’s pumping action, enabling it to contract and propel blood throughout the circulatory system.
- The thickness of the myocardium varies among the heart’s chambers, influenced by the pressure each chamber must generate.
- In general, the myocardium is thinner in the atria compared to the ventricles, with the left ventricle exhibiting the greatest thickness.
- In adult animals, the left ventricular myocardium is approximately three times thicker than that of the right ventricle.
- This disparity arises because the left ventricle pumps blood into the systemic circulation against higher pressure, necessitating a more robust muscular wall.
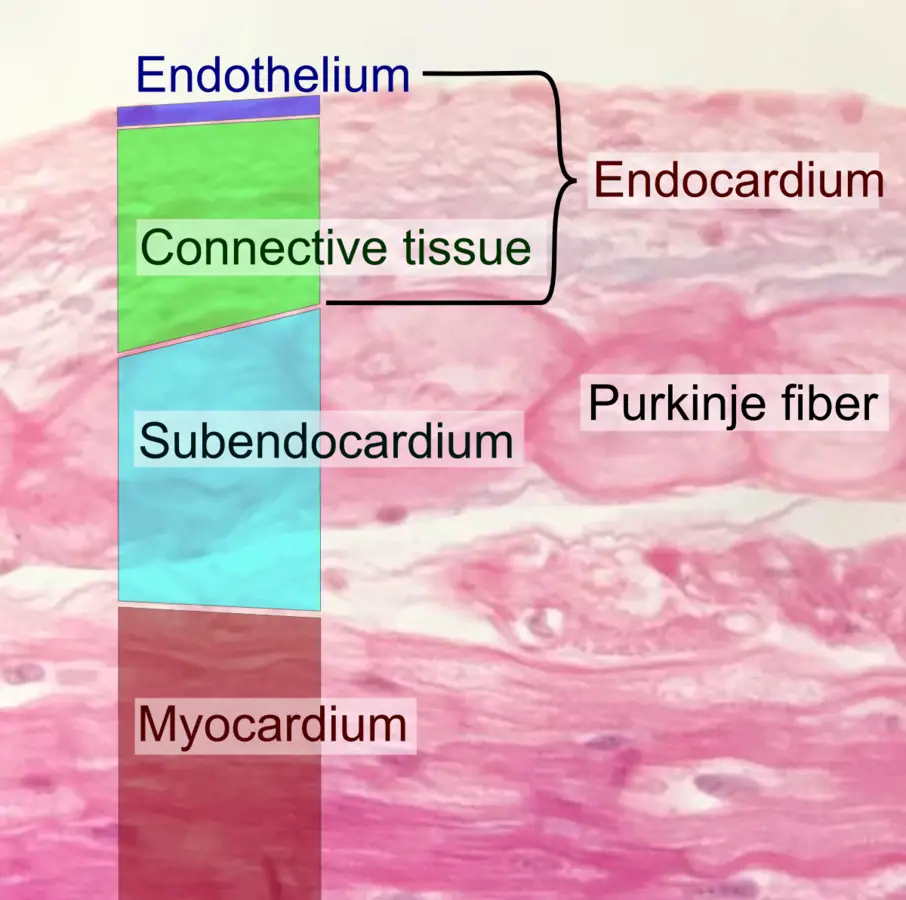
- Endocardium:
- The endocardium is the innermost layer of the heart, lining the interior walls and the heart valves.
- This layer is further divided into two components:
- Inner Endothelial Cell Layer: This thin layer consists of endothelial cells that provide a smooth lining for the heart chambers, minimizing turbulence as blood flows through.
- Subendocardial Layer: This connective tissue layer is continuous with the myocardial connective tissue layer. It houses the impulse-conduction system of the heart, which is crucial for coordinating heartbeats and ensuring effective contractions.
Cardiac Muscle Histology
Cardiac muscle, a vital component of the heart, is distinguished by its unique structure and function. As one of the three types of vertebrate muscle—alongside skeletal and smooth muscle—cardiac muscle possesses features that set it apart while also sharing characteristics with both smooth and skeletal muscles. Understanding the histology of cardiac muscle is essential for comprehending its role in cardiovascular function.
- Definition and Characteristics:
- Cardiac muscles are involuntary, striated muscles composed of specialized cells known as cardiomyocytes.
- Unlike skeletal muscle, which can contract voluntarily, cardiac muscle operates autonomously and rhythmically.
- The muscle fibers are striated, similar to skeletal muscle, and exhibit strong contractions akin to those seen in smooth muscle.
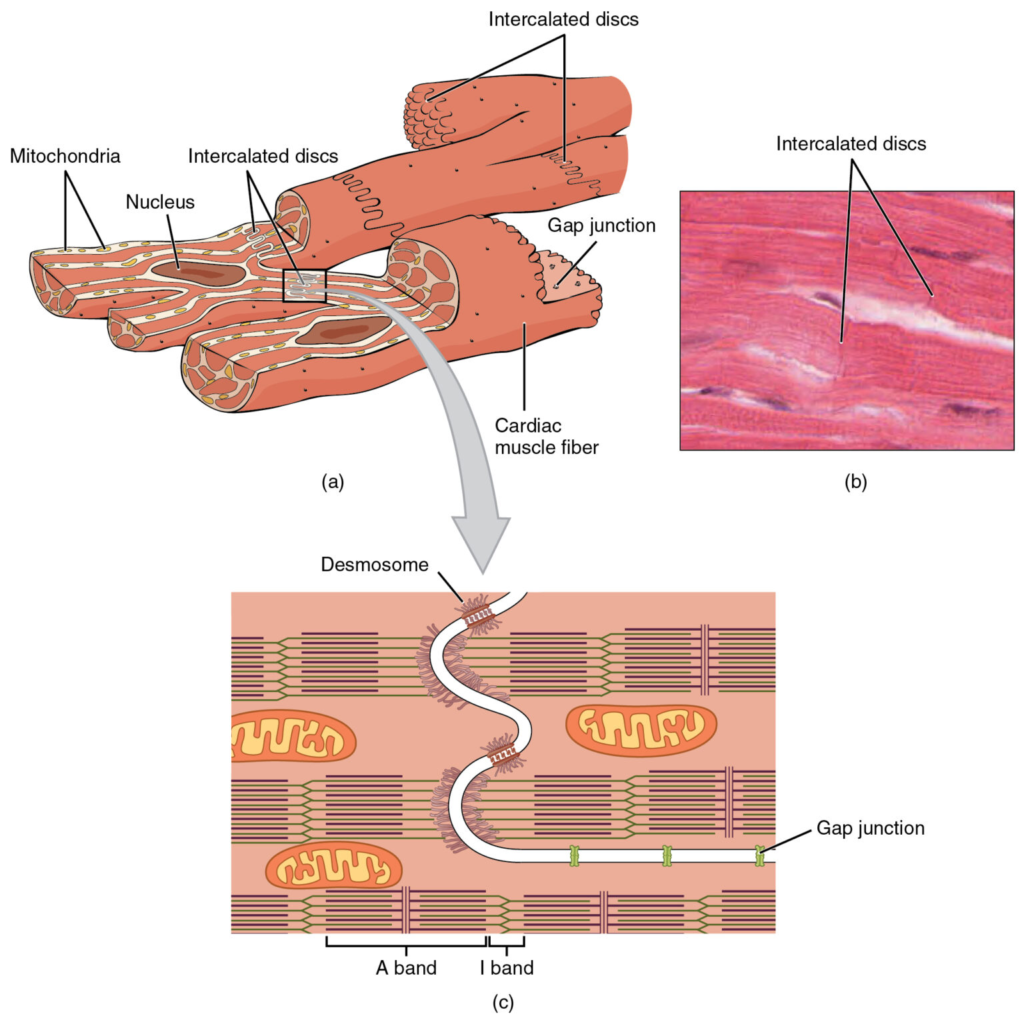
- Structural Arrangement:
- Cardiomyocytes are arranged in a helical or overlapping spiral pattern, creating a complex three-dimensional network.
- Each cardiac muscle fiber is elongated and cylindrical, typically measuring 50–100 μm in length and 10–25 μm in width.
- The individual cells are quadrangular in shape with a centrally located, clear oval nucleus.
- These muscle cells often branch and connect end-to-end, forming a functional syncytium, which allows for coordinated contractions.
- Intercalated Discs:
- Intercalated discs are specialized junctions where two cardiac muscle cells meet.
- These discs contain three critical components:
- Desmosomes: Join the intermediate filaments of the cytoskeleton, providing structural stability.
- Gap Junctions: Facilitate the spread of electrical excitation by offering low electrical resistance, promoting synchronization of contractions.
- Fascia Adherens: Connects with actin filaments to transmit the contraction force between cells.
- The structure of intercalated discs includes tightly bound membranes by desmosomes, connected through gap junctions, essential for efficient electrical impulse conduction between cells.
- Contractile Function:
- Cardiac muscle cells are capable of strong, continuous, and rhythmic contractions generated automatically.
- Although the autonomic nervous system and hormones can modulate contractility, the basic rhythm is inherently myogenic.
- Under microscopic examination, intercalated discs appear as faint lines perpendicular to the long axis of the muscle fibers.
- Histological Features:
- In adult human cardiac muscle, a brown pigment called lipofuscin can often be observed around the nucleus.
- Lipofuscin is considered a “wear and tear” pigment, resulting from the accumulation of lipids, phospholipids, and proteins due to lipid peroxidation.
- Sarcomeres and Contractile Proteins:
- Sarcomeres serve as the functional units of cardiac myocytes, surrounded by transverse discs known as Z-bands.
- Each myocyte contains numerous sarcomeres stacked end-to-end, creating a “cable effect” that enhances contraction.
- The primary proteins involved in contraction are myosin and actin, with thick filaments composed of myosin and thin filaments made of actin.
- These proteins collectively form the myofibrillar filament, enabling contractile function in cardiac tissue.
- Metabolic Requirements:
- The sarcoplasm, or cytoplasm, of cardiac muscle cells is rich in mitochondria, reflecting the high energy demands for continuous contractions.
- Cardiac muscle relies on oxidative phosphorylation to meet energy needs and requires a constant supply of oxygen delivered by coronary arteries.
- Additionally, glycogen granules are present within the myofibrils, providing a reserve of energy.
- Oxygen Demand and Ischemia:
- The myocardium has the highest oxygen requirement among tissues and is critically affected by reduced blood flow, known as ischemia.
- Cardiac muscles are highly resistant to fatigue, allowing for sustained contractions over a lifetime.
- Conducting System:
- Cardiac muscle cells can generate their own action potential, making them myogenic in nature.
- Specialized cells within the myocardial conduction system, including the sinoatrial node, atrioventricular node, bundle of His, and Purkinje fibers, play a key role in initiating and conducting impulses.
- Notably, 99% of the myocardium consists of contractile cells, while the remaining 1% is dedicated to the conduction system.
Physiology of the Myocardium
The myocardium, the muscular layer of the heart, plays a critical role in the overall function of the circulatory system. Understanding its physiology provides insights into how the heart generates and maintains rhythmic contractions essential for effective blood circulation.
- Action Potential and Calcium Release:
- The physiological process begins with the generation of an action potential or nerve impulse.
- This impulse stimulates the sarcoplasmic reticulum within cardiac muscle cells, leading to the release of calcium ions (Ca²⁺) into the cytoplasm.
- The influx of Ca²⁺ ions is crucial for initiating contraction, as they bind to troponin.
- Role of Troponin and Tropomyosin:
- Upon binding of Ca²⁺, troponin undergoes a conformational change that causes tropomyosin to shift position.
- This repositioning of tropomyosin allows myosin heads to attach to actin filaments, facilitating the contraction process.
- Contraction Mechanism:
- Myosin utilizes stored ATP molecules to perform a power stroke, effectively shortening each sarcomere and leading to muscle contraction.
- The result is a coordinated contraction of the cardiac muscle fibers, generating force against the walls of the heart chambers.
- Calcium Reabsorption and Relaxation:
- In the absence of a nerve impulse, calcium ions are rapidly reabsorbed back into the sarcoplasmic reticulum.
- This reabsorption of Ca²⁺ causes troponin to re-anchor to tropomyosin, leading to relaxation of the cardiac muscle cells.
- This relaxation phase is essential for allowing the atria to fill with blood in preparation for the next contraction cycle.
- Contraction Dynamics:
- Cardiac muscle exhibits twitch-type contractions characterized by a long refractory period followed by brief relaxation.
- The arrangement of cardiac muscle fibers in sheets, with each muscle fiber positioned perpendicularly to its neighbors, allows for multi-directional contraction.
- This structural organization ensures that when the heart contracts, it generates a strong pumping and twisting force, effectively shrinking the ventricles and atria from multiple angles.
- Metabolic Requirements:
- The myocardium primarily relies on aerobic metabolism for energy production, utilizing lipids and carbohydrates to meet its high energy demands.
- This aerobic requirement underscores the importance of a continuous oxygen supply to maintain optimal cardiac function.
Functions of the Myocardium
The myocardium, the muscular layer of the heart, plays a vital role in the circulatory system. Understanding its functions is crucial for comprehending how the heart operates effectively to maintain blood circulation throughout the body.
- Contraction and Relaxation:
- The primary function of the myocardium is to facilitate the contraction and relaxation of the heart.
- During contraction, the cardiac muscles pump blood from the ventricles into the systemic circulation.
- This pumping action is essential for delivering oxygen and nutrients to every cell and tissue in the body.
- Conversely, during relaxation, the myocardium allows the atria to receive blood, preparing for the next cycle of contraction.
- Pumping Mechanism:
- The rhythmic beating of the heart is a result of the myocardium’s ability to contract and relax in a coordinated manner.
- This cycle ensures continuous blood flow, which is critical for maintaining homeostasis and supporting cellular functions.
- Autonomic Nervous System Control:
- Cardiac muscles are regulated by the autonomic nervous system, which is responsible for involuntary bodily functions.
- The autonomic nervous system releases timed neural impulses that signal the myocardium to contract and relax rhythmically.
- This precise timing is crucial for maintaining an effective heart rate and ensuring optimal blood circulation throughout the body.
Myocardium Dysfunction
Myocardium dysfunction encompasses a range of cardiac conditions that impair the heart’s ability to function effectively. These dysfunctions can be categorized as primary, stemming from genetic causes, or secondary, often arising from acquired factors but potentially exacerbated by genetic predispositions. Understanding these dysfunctions is crucial for both clinical and educational purposes.
- Cardiomyopathy:
- Definition: Cardiomyopathy refers to diseases that result from a dysfunctional myocardium and is a leading cause of morbidity and mortality worldwide.
- Types of Cardiomyopathy:
- Dilated Cardiomyopathy: Characterized by ventricular dilation, this condition presents symptoms of congestive heart failure. Contributing factors include arterial hypertension, myocarditis, alcohol abuse, and tachyarrhythmias.
- Hypertrophic Cardiomyopathy: This involves hypertrophy, particularly of the left ventricle, and is often genetically inherited through mutations affecting the sarcomere.
- Restrictive Cardiomyopathy: It is marked by scarring and stiffening of the ventricular walls, which impairs diastolic filling of the heart.
- Arrhythmic Cardiomyopathy: Caused by genetically defective desmosomes, this non-ischemic cardiomyopathy is characterized by arrhythmias, primarily affecting the right ventricle but occasionally the left.
- Unclassified Cardiomyopathy: This category includes forms of cardiomyopathy that do not fit into the established classifications.
- Myocardial Infarction (Heart Attack):
- Oxygen Demand: Cardiac tissues have an exceptionally high requirement for oxygen and energy, supplied through coronary arteries.
- Atheroma Formation: These arteries are prone to developing atheromas, abnormal deposits of fatty acids, cholesterol, and cell debris that can obstruct blood flow.
- Consequences: A significant reduction in oxygen supply leads to myocardial ischemia, which can result in the death of cardiac tissue. Although the body attempts to repair this tissue, the formation of fibrous tissue disrupts normal electrical conduction, potentially resulting in arrhythmias such as ventricular fibrillation.
- Types of Cardiomyopathy:
- Ischemic Cardiomyopathy: This develops from diffuse coronary atherosclerosis leading to prolonged cardiac ischemia and often follows silent myocardial infarction episodes.
- Metabolic Cardiomyopathy: High blood glucose levels associated with diabetes can lead to ventricular dysfunction.
- Peripartum Cardiomyopathy: This condition occurs in women within one month post-delivery or up to five months postpartum, characterized by left ventricular systolic dysfunction.
- Tachycardia-Induced Cardiomyopathy: Chronic elevated heart rates (above 110 beats per minute) from conditions like sustained ventricular tachycardia or atrial fibrillation can lead to cardiomyopathy if untreated, ultimately resulting in heart failure.
- Consequences of Untreated Cardiomyopathy:
- Heart Failure: Insufficient heart pumping leads to inadequate blood supply, posing life-threatening risks.
- Blood Clots: These can form due to blood stasis, risking obstruction of blood flow to vital organs, potentially resulting in a stroke.
- Valve Dysfunction: Enlargement of the heart may cause improper closure of heart valves.
- Cardiac Arrest and Sudden Death: Arrhythmias associated with cardiomyopathy can lead to fainting or sudden death.
- Myocarditis:
- Definition: Myocarditis is the inflammation of the myocardium, which can be caused by various factors, including viral infections, toxic substances, drug allergies, and autoimmune disorders.
- Cellular Impact: This inflammation leads to the injury and loss of cardiomyocytes and cardiac vascular endothelial cells, prompting white blood cell infiltration.
- Long-term Effects: The condition can result in interstitial cardiac fibrosis, wall motion abnormalities, arrhythmias, reduced ejection fraction, and may culminate in heart failure or sudden cardiac death. Symptoms can include chest pain, dyspnea, and flu-like manifestations, though it can also be asymptomatic.
- Heart Failure:
- Definition: Heart failure, or congestive heart failure, represents the end-stage pathway of cardiac dysfunction, characterized by the heart’s inability to pump adequate blood.
- Classification: This condition can be categorized as acute versus chronic, right heart versus left heart, or systolic versus diastolic, with each type presenting distinct clinical characteristics.
- Causes: Common causes include myocardial injury or infarction, chronic hypertension, valvular dysfunction, and arrhythmias. Symptoms typically include shortness of breath, fatigue, and leg swelling. Treatment often involves medications like ACE inhibitors and beta-blockers.
- Perioperative Myocardial Injury:
- Definition: This complication occurs after non-cardiac surgery and is distinct from myocardial infarction.
- Risk Factors: Patients aged 65 or older with a history of atherosclerotic disease are particularly susceptible.
- Symptoms and Diagnosis: Perioperative myocardial injury may manifest without typical symptoms like chest pain or dyspnea, complicating diagnosis. Elevated levels of cardiac troponin T (hs-cTn) are indicative. Screening for hs-cTn is critical to assess risk, as this condition significantly increases the likelihood of 30-day mortality following non-cardiac surgery.
Biological Importance of Myocardium
The myocardium, comprising cardiac muscle tissue, is critical to the physiological functioning of the heart and, consequently, the entire body. As the central pumping organ, the heart plays a vital role in circulating blood, which delivers essential oxygen and nutrients to cells and tissues. The myocardium’s ability to rhythmically contract and relax is fundamental to maintaining life and overall health.
- Central Role in Circulation:
- The myocardium’s contractions and relaxations facilitate the pumping of blood throughout the body. This process ensures that every cell receives adequate oxygen and nutrients necessary for their metabolic functions.
- The effective pumping action of the heart is indispensable for sustaining the body’s physiological demands, particularly during periods of increased activity or stress.
- Development and Lifespan:
- Cardiac muscle cells, or cardiomyocytes, are among the earliest organs to develop during embryonic growth. This early formation underscores the myocardium’s significance in establishing life and maintaining cardiovascular integrity throughout an individual’s lifespan.
- The myocardium must remain functional and resilient to adapt to varying physiological conditions, emphasizing its role in long-term health.
- Structural Composition:
- The myocardium constitutes the thickest layer of the heart wall, forming a robust and resilient structure necessary for generating the force required for effective blood circulation.
- The myocardium is intricately linked with the coronary vasculature, cardiac lymphatics, and autonomic nervous system, which together regulate cardiac function, blood flow, and the heart’s response to bodily needs.
- Impact of Dysfunction:
- Dysfunction of the myocardium can lead to severe cardiovascular complications, significantly affecting health outcomes. Myocardial diseases can result in contractile dysfunction, cell damage and death, and ultimately cardiac pump failure.
- Cardiovascular diseases, which prominently involve the myocardium, are the leading cause of mortality worldwide. Such diseases highlight the essential role of the myocardium in maintaining cardiovascular health and the critical need for its proper functioning.
- Pathological Conditions:
- A range of cardiac diseases can impair the myocardium, including various forms of cardiomyopathy, myocardial infarction, and myocarditis. Each of these conditions affects the myocardium’s ability to contract and relax effectively, leading to decreased cardiac output and systemic perfusion.
- The consequences of myocardial dysfunction can manifest as heart failure, arrhythmias, and increased risk of sudden cardiac events, illustrating the myocardium’s vital role in overall cardiac health.