- George Hirst, an American virologist, created the hemagglutination assay or haemagglutination assay (HA) and the hemagglutination inhibition test (HI or HAI) in 1941–1942 as procedures for determining the relative concentration of viruses, bacteria, or antibodies.
- Hemagglutination is a process that causes red blood cells, such as the influenza virus, to clump together in the presence of some enveloped viruses.
- Hemagglutinin, a glycoprotein on the viral surface, interacts with red blood cells, causing red blood cell clustering and the creation of a lattice.
- In the absence of an enveloped virus, red blood cells precipitate to form a red dot at the bottom of a container.
- In the presence of a virus, however, red blood cell clusters are scattered and do not form a red dot. This is the fundamental principle underlying hemagglutination assays.
What is Hemagglutination assay?
- The hemagglutination assay, also known as the haemagglutination assay (HA), and the hemagglutination inhibition assay (HI or HAI), were developed by George Hirst, an American virologist, in the early 1940s. These assays serve as valuable methods for quantifying the relative concentration of viruses, bacteria, or antibodies.
- The hemagglutination assay and hemagglutination inhibition assay utilize a process called hemagglutination, which involves the binding of sialic acid receptors on the surface of red blood cells (RBCs) to the hemagglutinin glycoprotein present on the surface of certain viruses, including the influenza virus and several others. This interaction leads to the formation of a network or lattice structure, where RBCs and virus particles become interconnected.
- As a result of this lattice formation, the RBCs remain suspended in a dispersed reddish solution. The formation of the lattice is dependent on the concentrations of the virus and RBCs. When the virus concentration is too low, the lattice is unable to constrain the RBCs, causing them to settle at the bottom of the well. This observation of hemagglutination is not limited to viruses but can also be seen in the presence of certain bacterial species like staphylococci, vibrios, and others. These bacteria employ a similar mechanism to induce agglutination of erythrocytes.
- To perform HA and HI assays, RBCs obtained from chickens, turkeys, horses, guinea pigs, or humans are used, depending on the selectivity required for the specific virus or bacterium being targeted and the associated surface receptors on the RBCs.
- The hemagglutination assay and hemagglutination inhibition assay have been essential tools in virology and bacteriology for many years. They allow researchers to measure the concentration of viruses, bacteria, or antibodies in a sample, providing valuable information about their presence and activity. These assays continue to be widely used in various scientific and medical fields, contributing to our understanding of infectious diseases and aiding in the development of diagnostic tests and vaccines.
Haemagglutination Test Principle
The fundamental principle underlying the hemagglutination test revolves around the interaction between antigens and antibodies present on the surface of Red Blood Cells (RBCs). When these antigens encounter their corresponding complementary antibodies or vice versa, they bind together, resulting in the agglutination or clumping of the RBCs. This agglutination process is easily observable and serves as a distinct indicator for distinguishing between a positive and a negative test result.
In this test, the presence or absence of agglutination provides valuable information about the interaction between antigens and antibodies. When the specific antigen and its complementary antibody are present in the sample, they will combine, leading to the visible clumping of the RBCs. This clumping is readily distinguishable to the naked eye or under a microscope, allowing for a positive test result to be determined.
On the other hand, if the antigen and its corresponding antibody are not present or do not interact, no agglutination will occur. In such cases, the absence of clumping indicates a negative test result.
The principle of hemagglutination testing is widely utilized in various applications, including the detection and quantification of viruses, bacteria, and antibodies. By exploiting the inherent agglutination property of antigens and antibodies, this test provides a reliable and visually apparent means of assessing the presence or absence of specific substances in a sample.
Overall, the hemagglutination test principle is centered on the ability of antigens and antibodies to bind and agglutinate, resulting in observable clumping. This principle forms the basis for conducting hemagglutination assays and is an essential tool in various scientific, medical, and diagnostic settings.
Materials Required
Several requirements are necessary to perform a hemagglutination assay effectively. These requirements ensure the accurate detection and quantification of antibodies, antigens, or viruses. The following components are typically needed:
- RBC Suspension: The RBC suspension used in the assay serves as a carrier particle. It is coated with either antigens specific to the antibody to be detected or antibodies specific to the antigens to be detected. The choice of RBCs depends on the specific assay and the desired target. RBCs from humans, sheep, chicks, and other sources can be utilized.
- Serum or Blood Sample: A serum or blood sample containing the antibodies, antigens, or viruses under investigation is required. This sample is added to the assay to assess the presence or concentration of the target substance.
- Microtitre Plates: Microtitre plates, such as 96-well V-bottomed plates, are commonly used in hemagglutination assays. These plates allow for the simultaneous testing of multiple samples, increasing efficiency and throughput.
- Diluent: Phosphate Buffered Saline (PBS) is a commonly used diluent in hemagglutination assays. It provides a suitable environment for the reaction between the RBCs and the target substances. PBS helps maintain the pH and ionic balance necessary for optimal hemagglutination.
- Negative and Positive Control Samples: Control samples are essential in hemagglutination assays to validate the accuracy and reliability of the results. Negative control samples do not contain the target substance and serve as a baseline for comparison, while positive control samples contain a known concentration of the target substance to validate the assay’s sensitivity and specificity.
- Rapid Hemagglutination Assay (RDT) Kits: In certain cases, rapid hemagglutination assay kits may be employed. These kits typically include slides, reagents, and control samples specifically designed for rapid and convenient testing.
By ensuring the availability of these requirements, researchers and healthcare professionals can perform hemagglutination assays accurately and reliably. These assays play a crucial role in various fields, including virology, bacteriology, immunology, and diagnostics, providing valuable insights into infectious diseases and facilitating the development of effective diagnostic tools and vaccines.
Procedure of Haemagglutination Test
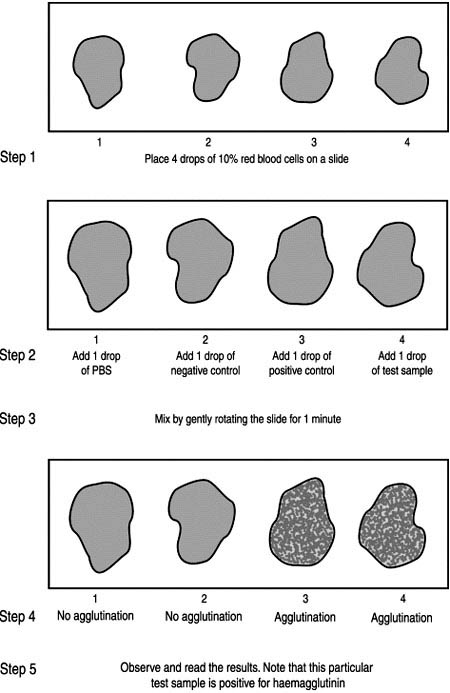
Rapid haemagglutination test
The Rapid Hemagglutination Assay, also known as Rapid Diagnosis Test (RDT), is designed to quickly determine the presence of a hemagglutinating agent. It is named as such because it can provide results in approximately one minute. When conducting this test on multiple samples, it is sufficient to test the negative and positive control samples only once.
During the hemagglutination test, it is important to assess the settling pattern of the red blood cell suspension. This is achieved by mixing the diluent with the red blood cells and allowing them to settle.
Here is the procedure for examining the settling pattern:
- Dispense the diluent into the designated area.
- Add the red blood cells to the diluent and gently mix them to ensure proper combination.
- Allow the red blood cells to settle undisturbed for a brief period.
- Examine the pattern of the settled cells. In the Rapid Hemagglutination Assay, the cells should settle in a normal pattern without any signs of auto-agglutination or clumping. The result should show a distinct button of cells and an even suspension, indicating a negative result.
The Rapid Hemagglutination Assay is advantageous because it provides quick results, allowing for rapid diagnosis of the presence of a hemagglutinating agent. By assessing the settling pattern of the red blood cells, potential issues such as auto-agglutination can be detected, ensuring the accuracy of the assay.
Procedure of Rapid haemagglutination test
To conduct the rapid haemagglutination test, it is important to follow a precise procedure. Here is a step-by-step guide:
- Ensure that all kit components are at room temperature (15-30°C) before starting the test. Allow them to equilibrate for approximately 30 minutes. Gently mix the liquid reagents.
- Determine the total number of samples to be tested and the number of plates required for the assay.
- If necessary, assign a unique plate ID in the upper-middle portion of each plate to differentiate them.
- On the lower left side of each well, label the plate with the last three numbers of the donor’s ID to indicate the well placements. Remember to include one negative control and one positive control for every batch of samples.
- Arrange the samples in a sampling rack according to the plate map to ensure accurate placement.
- Take the first additional well based on the number of samples and add 190 μl of sample diluent.
- Using a fresh pipette tip for each addition, combine 10 μl of specimen with 190 μl of sample diluent in the same position in the extra well or plate.
- Transfer 25 μl of the diluted sample to each of the control and test wells.
- After sampling, place the sample in the same or a different position in the sampling rack.
- Add 25 μl of the control cell suspension to the negative and positive control wells, respectively.
- Gently mix the control and test cell bottles to ensure a homogeneous suspension. Then, add one drop (approximately 75 μl) of the suspension to each well, including the positive and negative control wells.
- Mix the contents of each well by slowly rotating the plate in a circular motion. Keep the plate on a level and stable surface.
- Incubate the plate at room temperature for one hour.
- After the incubation period, examine the results. Look for the presence or absence of agglutination in each well. Agglutination indicates a positive result, while the absence of agglutination suggests a negative result.
By following this standardized procedure, the rapid haemagglutination test can be conducted accurately and reliably. It is an efficient method for detecting and assessing the presence of specific substances in samples within a relatively short time frame.
Interpretation of the test result
The interpretation of the test results in a haemagglutination assay is crucial in determining the presence or absence of specific antibodies or infections. Here’s how to interpret the results:
- Control Well: Each control well should exhibit a distinct button-like structure indicating proper functioning of the test. If any control well lacks button formation, it indicates a technical problem, and the test should be repeated to ensure accurate results.
- Agglutination of Control and Test Cells: If both the control and test cells show agglutination, it suggests the presence of anti-cell antibodies. In such cases, the test is considered invalid, and the serum should undergo absorption. To do this, dilute 1/4 of the test serum with control cells and let it stand at room temperature. After centrifugation for 5 minutes at 1000 rpm, dilute the supernatant one-fifth with the diluent. Test this diluted sample directly, without further dilution, using suspensions of test and control cells.
- Nonreactive Result: If a test well displays a compact button without agglutination, the result is termed nonreactive, indicating the absence of the specific substance being tested for.
- Reactive Result for T. pallidum: In the case of T. pallidum detection, a reactive result is indicated by the presence of a typical ring pattern or net of cells in the test well, while the control well exhibits a compact button formation.
- Confirmation of Positive Results: Positive test results in TPHA (Treponema pallidum hemagglutination assay) should be repeated to confirm the findings.
- Further Testing: If a sample is repeatedly positive, it is important to identify and isolate the sample. Retesting with other specific tests, such as RPR (Rapid Plasma Reagin), can help further assess the presence of infection or antibodies.
It is worth noting that agglutination reactions can be used to determine bacterial infections. For example, in suspected cases of typhoid fever, the patient’s serum is mixed with a culture of Salmonella typhi. If agglutination occurs, characterized by clumping of the bacteria, it indicates a current or past infection with S. typhi. However, the presence of specific antibodies does not necessarily imply an ongoing infection, as antibodies can persist in the bloodstream long after recovery. To assess the current infection status, antibody levels or titers are measured at the onset of disease and again two weeks later.
By carefully interpreting the results of a haemagglutination assay, healthcare professionals can gain valuable insights into the presence or absence of specific antibodies or infections, aiding in accurate diagnosis and appropriate treatment decisions.
Micro haemagglutination test in a V-bottom microwell plate
The Micro-hemagglutination Assay is a valuable method used to determine the presence or absence of hemagglutinin in allantoic fluid obtained from embryonated eggs. While it is a more time-consuming approach compared to the Rapid Diagnosis Test (RDT), it offers its own advantages and specific applications.
In the Micro-hemagglutination Assay, red blood cells are dissolved in a 1% solution. This allows for a standardized suspension of cells for testing. The use of V-bottom plates in this assay is preferred as the cells settle more quickly and efficiently in the V-shaped wells. The settling pattern of the red blood cells is an important factor to consider during the analysis.
One significant advantage of the Micro-hemagglutination Assay is that the difference between positive and negative results is more pronounced compared to U-bottom plates. This enhances the accuracy and reliability of result interpretation. While this method may require more time and attention compared to the Rapid Diagnosis Test, it provides valuable insights into the presence or absence of hemagglutinin in the allantoic fluid.
The Micro-hemagglutination Assay is particularly useful in research settings, where a more detailed analysis of hemagglutinin is required. By utilizing this method, scientists can gather important information about the hemagglutinating properties of samples and better understand the nature of the tested agents.
In summary, the Micro-hemagglutination Assay is a reliable and informative method for testing the presence of hemagglutinin in allantoic fluid. While it may be more time-consuming, its use of standardized red blood cell suspension and V-bottom plates contribute to more distinct and accurate results, making it a valuable tool in various research applications.
Materials Required
- Inoculated eggs, chilled for at least 2 hours, preferably overnight
- Negative and positive control samples
- V-bottom microwell plate and lid
- Micropipette and tips to measure 50 µL
- 1 percent suspension of red blood cells
- 70 percent alcohol solution
- Cotton wool
- Forceps and/or small scissors
- Absolute alcohol
- Discard tray
- Microwell plate recording sheet.
Procedure of Micro haemagglutination test in a V-bottom microwell plate
The micro-hemagglutination assay follows a specific procedure for accurate testing. Here is a step-by-step guide:
- Begin by filling out a recording sheet, providing relevant information about the samples to be tested. This sheet will help track and record the results of the assay.
- Using a micropipette, take a sample of approximately 50 μl and dispense it into a designated well of the microwell plate. It is important to use a new pipette tip for each sample to prevent any potential contamination between samples.
- Place negative and positive controls on one of the plates. These controls are essential for comparison and validation of the test results.
- Add 50 μl of Phosphate Buffered Saline (PBS) to each well. These wells will serve as auto-agglutination controls for the red blood cells.
- Fill each well with 25 μl of 1% red blood cells. The red blood cells will act as the carrier particles in the assay.
- Gently tap the sides of the plate to ensure proper mixing of the contents in each well. This will facilitate the interaction between the samples and the red blood cells.
- Cover the plate with a plate cover to create a controlled environment for the assay.
- Allow the plate to stand for approximately 40 minutes to allow sufficient time for the reaction to occur.
- During this incubation period, observe and carefully record the data. Note any visible agglutination or lack thereof in each well.
Results
The results of the micro-hemagglutination assay are determined based on the settling patterns of red blood cells within the wells. Here’s how to interpret the results:
- Negative HA Outcome: In a negative result, individual red blood cells settle down the sides of the V-shaped well, forming a sharp button at the bottom. This indicates that there is no agglutination or clumping of the red blood cells, and the result is considered negative for the specific antigen or antibody being tested.
- Positive HA Result: A positive result is observed when agglutination occurs. In this case, the red blood cells do not form a distinct button by rolling down the sides of the well. Instead, they settle as a diffuse film, indicating the presence of agglutinated cells. This suggests the presence of the specific antigen or antibody being tested for.
- Control of Red Blood Cells: As part of the assay, a control using red blood cells alone is included. In the control wells, individual red blood cells should settle down the sides of the well, forming a sharp button similar to the negative HA outcome. This control helps ensure that the red blood cells are functioning properly and provides a baseline for comparison with the test results.
- Notating the HA Results: It is important to record the results of the micro-hemagglutination assay on the microwell sheet or a designated recording sheet. The HA outcomes, whether negative (sharp button) or positive (diffuse film), should be clearly notated for each sample tested.
By carefully observing and interpreting the settling patterns of red blood cells, healthcare professionals and researchers can determine the presence or absence of specific antigens or antibodies. Accurate documentation of the results is essential for analysis, comparison, and further decision-making. The micro-hemagglutination assay is a valuable tool in various diagnostic and research settings, providing valuable information about the interaction between samples and red blood cells.
Titration to establish haemagglutinin (HA) titre of a suspension of virus
The haemagglutination test is utilised to determine the concentration of Newcastle disease virus in a suspension. This is accomplished by doing two-fold serial dilutions of the viral suspension in a microwell plate, followed by testing to establish an endpoint. This result is then used to determine the concentration of haemagglutinin in the suspension and is expressed as a HA titre.
Materials Required
To perform the titration procedure for establishing the haemagglutinin (HA) titre of a virus suspension, the following materials are required:
- 96 well V-bottom microwell plate: This specialized plate with V-shaped wells allows for optimal settling and observation of haemagglutination patterns.
- Microwell plate cover: The cover is used to seal the microwell plate during the incubation period, preventing contamination and maintaining a controlled environment.
- 25 mL single and multi-channel micropipettes and tips: These pipettes, along with their corresponding tips, are essential for accurate and precise measurement and transfer of liquid samples and reagents.
- PBS (Phosphate-Buffered Saline): A buffer solution used to dilute the samples and provide the necessary environment for haemagglutination reactions.
- 1 percent chicken red blood cells: A suspension of chicken red blood cells at a concentration of 1 percent is used as a crucial component in the haemagglutination assay.
- Sample to be titrated: The virus suspension or sample being tested for haemagglutinin (HA) activity is a key material required for this procedure.
- Reagent troughs: These shallow containers or reservoirs are used for holding and dispensing the various reagents and diluents required during the titration process.
- Microwell plate recording sheet: This sheet is used to document and record the distribution of samples, controls, and reagents across the microwell plate, facilitating organized and systematic analysis of the results.
These materials are essential for conducting the titration procedure accurately and efficiently, enabling the determination of the haemagglutinin (HA) titre of the virus suspension under investigation.
Procedure
To establish the haemagglutinin (HA) titre of a suspension of virus, a titration procedure is followed. The steps involved in this procedure are as follows:
- Begin by recording the method of sample distribution on the recording sheets for reference and documentation.
- Dispense 25 μL of phosphate-buffered saline (PBS) into each well of the microwell plate.
- In the first well of each row and column in the first row, add 25 μL of the test samples. If needed, duplicate or triplicate testing can be performed.
- Using a multichannel pipette, perform successive two-fold dilutions across the plate until Column 11 is reached. Detailed instructions for carrying out these dilutions can be found in Appendix 4.
- Pour 25 μL of PBS into each well after completing the dilutions.
- Add 25 μL of red blood cells at a concentration of 1% to every well, including Column 12. Column 12 serves as the control wells and contains only PBS and red blood cells.
- Gently tap the sides of the plate to ensure proper mixing of the contents. Cover the plate with a lid.
- Allow the plate to rest undisturbed at room temperature for 45 minutes to allow for haemagglutination to occur.
- Read and record the results for each well. All control wells should show a negative haemagglutination (HA) result.
- HA-negative wells will exhibit a pinpoint of red blood cells at the base of the V-shaped well.
- HA-positive wells will display a hazy layer of red blood cells with either no button or a very small button of red blood cells at the bottom of the V-bottom well.
- Determine the conclusion based on the results. The final well that demonstrates complete haemagglutination represents one haemagglutinating unit, and this information is used to establish the HA titre of the virus suspension.
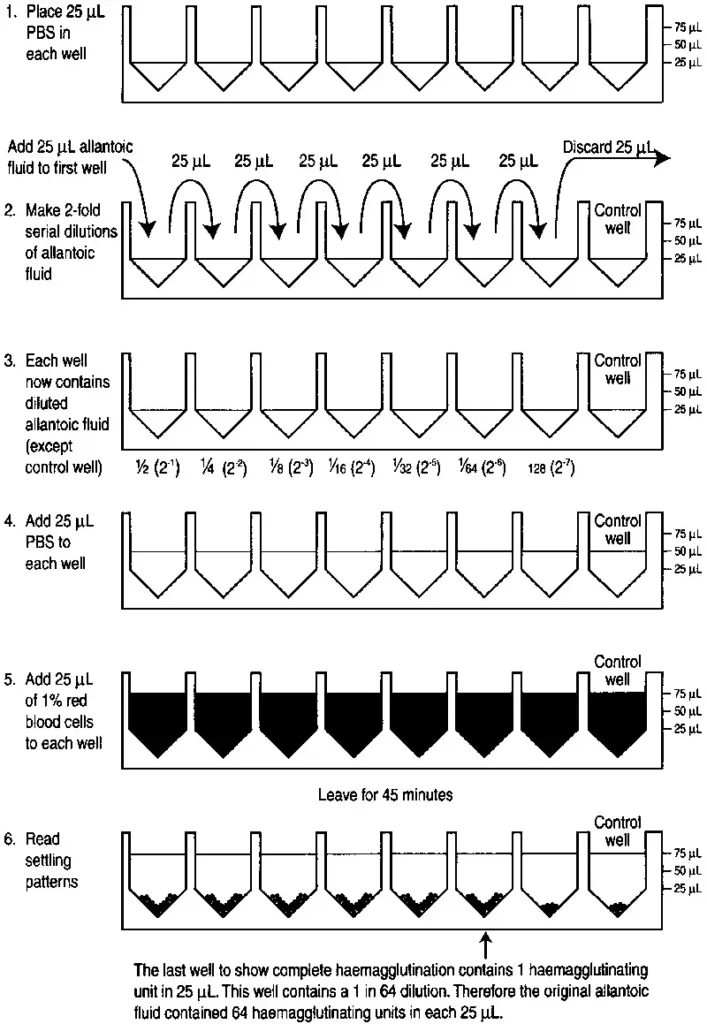
Calculation of the HA titre of the test sample
To calculate the HA titre of the test sample, the reciprocal of the dilution that yields one unit of HA is determined. Here is an example of how the HA titre is calculated:
In the titration shown in the figure, it is observed that a 1 in 64 (1/64) dilution of the test sample yields 1 unit of HA.
Therefore, the HA titre of the test sample can be calculated as follows:
HA titre = Reciprocal of the dilution that yields one unit of HA
HA titre = Reciprocal of 1/64
HA titre = 64
This means that the test sample has an HA titre of 64. Alternatively, it can also be expressed as 26, indicating 26 HA units per 25 mL.
By determining the dilution that produces one unit of HA and taking the reciprocal of that dilution, the HA titre of the test sample can be quantified. In this case, the Newcastle disease virus suspension has an HA titre of either 64 or 26 HA units per 25 mL, depending on the chosen representation.
Applications of Hemagglutination Assay
The hemagglutination assay finds wide applications in various fields due to its versatility and effectiveness. Here are some key applications of the hemagglutination assay:
- Detection of Humoral Immune Response: Hemagglutination assay is valuable in assessing the humoral immune response of the body against diseases or infectious agents. By measuring the agglutination reaction between red blood cells and antibodies, it can provide insights into the presence and quantity of specific antibodies in a patient’s serum. This is crucial in diagnosing and monitoring immune responses.
- Blood Typing and Grouping: Hemagglutination assay plays a significant role in determining different blood cell types or groups. It enables the identification of specific antigens present on red blood cells, allowing for accurate blood typing and matching in blood transfusion procedures and organ transplantation.
- Viral Infection Detection: Hemagglutination assay is employed in the detection and quantification of viral infections. It is particularly useful for viruses like paramyxovirus, influenza, and others that exhibit hemagglutination properties. By measuring the agglutination reaction between the virus and red blood cells, the assay can aid in diagnosing and monitoring viral infections.
- Rapid Diagnosis Test Kits: The principles of hemagglutination have been harnessed to develop rapid diagnostic test kits. These kits utilize hemagglutination-based reactions to detect specific infections or antigens quickly. For example, an RDT kit designed to detect Hepatitis B surface antigen (HbsAg) utilizes hemagglutination as a crucial component in the detection process.
- Bacterial Infection Detection: Hemagglutination assay is also employed in the detection of various bacterial infections. For instance, it is used in the diagnosis of syphilis, where the assay helps detect specific antibodies against the bacteria responsible for the infection.
Advantages of Hemagglutination Assay
The hemagglutination assay offers several advantages that contribute to its widespread use in diagnostics and research. Here are the key advantages of the hemagglutination assay:
- Simplicity: The hemagglutination assay is relatively simple to perform, making it accessible to a wide range of laboratories and healthcare settings. The procedure typically involves mixing the samples, red blood cells, and specific reagents, followed by observing the agglutination reaction. Its straightforward protocol facilitates its implementation and reduces the likelihood of procedural errors.
- Cost-Effectiveness: Compared to many other diagnostic tests, the hemagglutination assay is often more cost-effective. The reagents and equipment required for the assay are generally affordable and readily available, making it a practical option for resource-limited settings or when budget constraints are a consideration.
- Availability of Equipment: The equipment required for hemagglutination assays, such as microtitre plates, pipettes, and centrifuges, are commonly found in laboratories. These equipment are not specialized or exclusive to the assay, enhancing its accessibility and reducing the need for additional investments.
- Rapid Results Interpretation: In certain formats, such as the Rapid Diagnostic Test (RDT), the hemagglutination assay enables fast interpretation of results. RDTs are designed to provide quick and easily readable results, usually within a short period of time. This feature is particularly advantageous in point-of-care settings or situations where prompt decision-making is crucial.
Limitations of Hemagglutination Assay
The hemagglutination assay, despite its advantages, has certain limitations that should be taken into consideration. Here are the key limitations of the hemagglutination assay:
- Sensitivity to Experimental Variables: The hemagglutination assay is sensitive to experimental variables such as the incubation time and concentration of red blood cells (RBCs). Deviations from the recommended conditions can lead to incorrect results. Care must be taken to ensure consistent and accurate incubation times and appropriate RBC concentrations to obtain reliable and reproducible outcomes.
- Requirement for Specific Factors: The success of the hemagglutination assay relies on the specificity of the factors involved, such as antibodies, antigens, and reagents. Non-specific reactions or cross-reactivity can result in false-positive or false-negative results. It is crucial to use well-characterized and specific components to minimize the risk of erroneous interpretations.
- Expertise for Quantitative Analysis: The determination of quantitative values and result interpretation in the hemagglutination assay may require expertise and qualified individuals. The assay often involves titrations and dilutions, and the interpretation of results may necessitate a good understanding of the assay principles and relevant standards. Skilled personnel are needed to ensure accurate and reliable quantitative analysis.
- Manual Result Interpretation: The hemagglutination assay typically relies on manual result interpretation without the aid of digital data analysis. This dependence on visual observation can introduce variability and subjective interpretation. Different observers may have slight variations in their analysis, which can lead to discrepancies or errors in result interpretation. Standardization of interpretation criteria and regular training of personnel can help mitigate this limitation.
FAQ
What is a hemagglutination assay?
A hemagglutination assay is a laboratory technique used to detect the presence of antibodies or antigens by observing the agglutination (clumping) of red blood cells.
How does hemagglutination occur?
Hemagglutination occurs when specific antigens on the surface of red blood cells interact with corresponding antibodies, causing the red blood cells to clump together.
What are the applications of hemagglutination assay?
Hemagglutination assays have various applications, including detecting immune responses, determining blood cell types, quantifying viral infections, and diagnosing bacterial infections such as syphilis.
What are the advantages of hemagglutination assay?
Some advantages of hemagglutination assays include their simplicity, cost-effectiveness, availability of equipment, and rapid interpretation of results, especially in the case of rapid diagnosis tests (RDTs).
What are the limitations of hemagglutination assay?
The limitations of hemagglutination assays include the potential for incorrect results due to errors in incubation time and red blood cell concentration, the requirement for specific and qualified interpretation of results, and the manual nature of result interpretation, which can introduce observer errors.
How is a rapid hemagglutination assay performed?
A rapid hemagglutination assay, also known as an RDT, involves combining samples with red blood cells, observing their settling patterns, and interpreting the results within a minute.
What is a micro-hemagglutination assay?
A micro-hemagglutination assay is a more time-consuming method used to test the presence of hemagglutinin in allantoic fluid from embryonated eggs. It involves dissolving red blood cells in a 1% solution and observing their settling patterns in V-bottom plates.
What is the purpose of titration in hemagglutination assays?
Titration is performed to establish the hemagglutinin (HA) titre of a virus suspension. It involves serial dilutions of the sample and determining the dilution at which one unit of HA is observed.
How are HA titres calculated?
HA titres are calculated by taking the reciprocal of the dilution that yields one unit of HA. For example, if a 1 in 64 dilution produces one unit of HA, the HA titre would be 64.
Can hemagglutination assays be used for diagnostic purposes?
Yes, hemagglutination assays can be used for diagnostic purposes to detect and diagnose various infectious diseases, including viral and bacterial infections. However, the specific application and interpretation of the assay may vary depending on the disease being tested.
References
- S. Miyaishi, F. Moriya, (2005) Encyclopedia of Analytical Science (Second Edition)
Parija S.C., (2009), Textbook of Microbiology and Immunology, 2nd edition, Elsevier, a division of Reed Elsevier India Private Limited, pg. 108 - Sukhadeo B. Barbuddhe and Deepak B. Rawool, Methods in Microbiology, 2020
- Townsend, A., Rijal, P., Xiao, J. et al. A haemagglutination test for rapid detection of antibodies to SARS-CoV-2. Nat Commun 12, 1951 (2021). https://doi.org/10.1038/s41467-021-22045-y
- Thangavelu, C. P., & Koshi, G. (1980). Micro-indirect hemagglutination test for detection of antibodies to the Ibc protein of group B Streptococcus. Journal of clinical microbiology, 12(1), 1–6. https://doi.org/10.1128/jcm.12.1.1-6.1980
- https://nios.ac.in/media/documents/dmlt/Microbiology/Lesson-60.pdf
- https://www.fao.org/3/ac802e/ac802e0d.htm
- https://www.news-medical.net/health/An-Overview-of-Hemagglutination.aspx
- https://www.tandfonline.com/doi/pdf/10.1080/03079457708418208
- http://neradslab.res.in/document/SOP/NDV_HA_HI.pdf