What is Endocrinology?
- Endocrinology is a specialized branch of biology and medicine that focuses on the study of the endocrine system, encompassing the hormones it produces and the physiological processes these hormones regulate. This discipline involves understanding the intricate mechanisms of cell-to-cell signaling mediated by hormones, which are chemical messengers that travel through the bloodstream to exert effects on distant target tissues. The complexity of endocrinology necessitates a multidisciplinary approach, integrating insights from various scientific fields to fully grasp the multifaceted roles of hormones in human physiology.
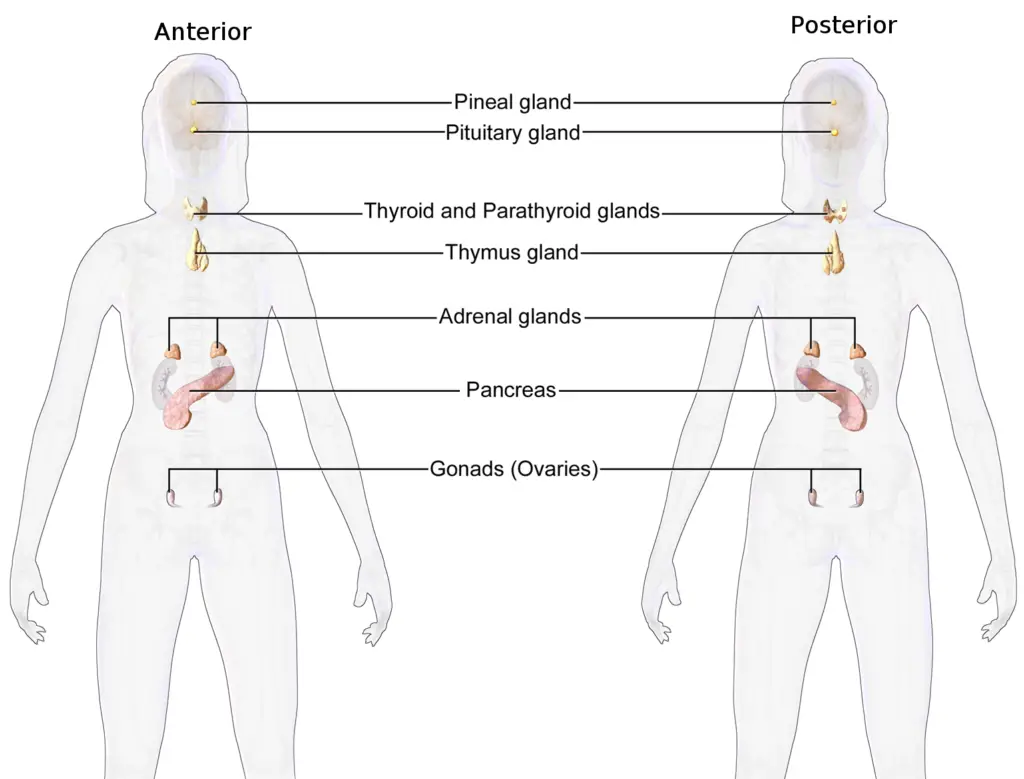
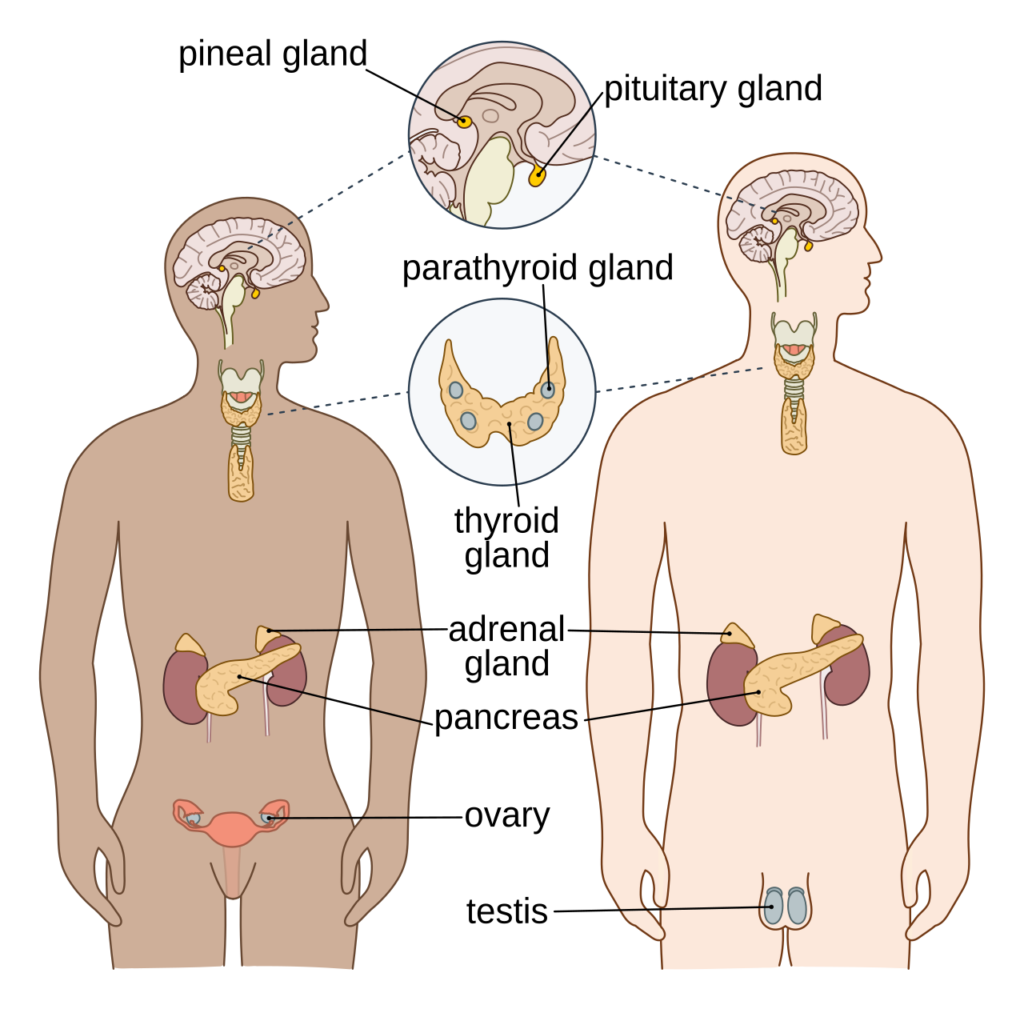
- The endocrine system is composed of several key glands, including the hypothalamus, pituitary, pineal, thyroid, parathyroid, adrenal glands, pancreas, and gonads (testes and ovaries). Each of these glands plays a vital role in maintaining the body’s internal balance, or homeostasis, through the secretion of hormones. Additionally, the gastrointestinal tract and other organs that modify or metabolize hormones also contribute to the overall functionality of the endocrine system. This network of glands operates through a dynamic interplay of feedback regulation, ensuring that hormonal levels remain within a precise range to support various bodily functions.
- Hormones influence a wide array of physiological processes, including metabolism, growth, tissue function, mood regulation, sleep cycles, digestion, and reproductive functions. For instance, one hormone may affect multiple organs and systems, while a single target organ can be influenced by several different hormones. This complexity underscores the need for a thorough understanding of the specific roles each hormone plays and how they interact with their respective receptors on target cells.
- Moreover, endocrinology also explores the integration of developmental processes, examining how hormonal actions guide proliferation, growth, and differentiation throughout various stages of life. The discipline extends beyond mere hormonal functions, encompassing behavioral endocrinology, which investigates the influence of hormones on behavior and psychological processes, as well as comparative endocrinology, which studies the hormonal systems across different species.
Definition of Endocrinology
Endocrinology is the branch of medicine and biology that studies the endocrine system, its glands, and the hormones they produce. It focuses on how hormones regulate various physiological processes, including growth, metabolism, reproduction, and behavior, as well as the diagnosis and treatment of hormonal disorders.
History of endocrinology
Endocrinology, the branch of physiology and medicine that studies the endocrine system and its hormones, has a rich and complex history characterized by a series of significant discoveries and the evolution of understanding regarding hormone functions. The development of this field can be categorized into three main phases: the initial descriptive phase of endocrines, the analytical phase, and the subsequent phase of synthetic endocrinology.
- Early Practices and Initial Observations:
- The origins of endocrinology can be traced back to the 17th and 18th centuries with the practice of castration, often performed on boys to preserve their singing voices and enhance certain physical traits. Although this practice was eventually abandoned due to severe side effects, it represented early interactions with hormonal influence on physiology.
- Berthold’s Experimentation (1849):
- In 1849, German physiologist Arnold Berthold conducted pioneering experiments involving the transplantation of testes from intact roosters to capons (castrated males). His work demonstrated that such transplants could restore typical male characteristics, though it did not receive widespread recognition at the time.
- Brown-Séquard and the Concept of Replacement Therapy (1889):
- The notion of hormonal replacement therapy emerged with French physician Charles Édouard Brown-Séquard, who famously injected himself with extracts derived from animal testes. He claimed enhanced physical and mental vitality from this practice, laying the groundwork for future hormone replacement concepts.
- Victor Horsley’s Advances:
- British surgeon Victor Horsley advanced the understanding of thyroid function when he observed that thyroid removal in monkeys led to myxedema. He proposed the transplantation of sheep thyroids to alleviate the symptoms, a concept later explored by George Murray, who developed an extract from sheep thyroids, significantly improving patient outcomes.
- The Definition of Hormones (1902):
- A pivotal moment in endocrinology occurred in 1902 when William Bayliss and Ernest Starling discovered secretin, the first hormone defined in scientific literature. They identified that secretin was released into the bloodstream in response to acidic gastric fluid entering the intestine, highlighting the intricate relationship between the digestive system and endocrine function.
- Formation of Professional Organizations (1916):
- The establishment of the Association for the Study of Internal Secretions in 1916, now known as the Endocrine Society, marked a significant step in formalizing the field and promoting research and collaboration among endocrinologists.
- Insulin Discovery and Its Clinical Application (1921):
- The journey to discover insulin began in the 19th century with observations of diabetes following pancreatic dissection in dogs. In 1921, Frederick Banting and Charles Best successfully extracted insulin from the pancreases of healthy dogs and treated diabetic dogs with it, leading to the first human insulin injection in Leonard Thompson. This monumental event transformed diabetes management and underscored the therapeutic potential of hormones.
- Sex Hormones and Their Functions:
- The late 19th and early 20th centuries also witnessed advances in understanding sex hormones, primarily through the work of Eugen Steinach, who explored the effects of testicular removal and subsequent transplantation in rats. His research established the role of interstitial cells in producing male sex hormones and revealed potential methods for manipulating testosterone levels through surgical interventions, such as vasectomy.
- Continued Innovations in Endocrinology:
- The field has since expanded to include numerous discoveries, including leptin, a hormone linked to body weight regulation and obesity. These advances highlight the ongoing exploration of hormone functions and their implications for health.
- Historical Context:
- The journey of endocrinology reflects a fascinating evolution from primitive practices based on superstition, such as the consumption of organs believed to impart strength, to a sophisticated understanding of hormonal interactions in health and disease.
What is Endocrine system?
- The endocrine system functions as a complex messenger system within an organism, utilizing hormones released from glands directly into the circulatory system. This system is essential for regulating and coordinating various physiological processes across different organs and tissues.
- The primary components of the endocrine system in humans include major glands such as the thyroid, parathyroid, pituitary, pineal, and adrenal glands, along with the testes in males and ovaries in females. Additionally, the hypothalamus, pancreas, and thymus also serve endocrine functions, contributing to the overall regulatory mechanisms of the body. The hypothalamus plays a critical role as the neural control center for the endocrine system, linking it with the nervous system through its connection to the pituitary gland.
- The hormonal secretions from these glands are crucial for maintaining homeostasis and regulating growth, metabolism, reproduction, and stress responses. For instance, the thyroid gland secretes thyroxine, which regulates metabolism, while the pituitary gland releases growth hormone, influencing growth and development. Furthermore, the pineal gland secretes melatonin, which regulates circadian rhythms, and the gonads produce sex hormones such as testosterone and estrogen.
- In addition to the specialized glands, several other organs, including the kidneys, liver, and heart, possess secondary endocrine functions. For example, the kidneys secrete erythropoietin, a hormone that stimulates red blood cell production in response to low oxygen levels. The interconnectedness of these glands can be illustrated through various hormonal axes, such as the hypothalamic-pituitary-adrenal axis, which illustrates how glands signal each other in a sequence to coordinate responses.
- Unlike exocrine glands, which secrete substances outside the body through ducts, endocrine glands release hormones directly into the bloodstream. This ductless characteristic, along with their vascular nature, facilitates efficient hormone distribution throughout the body. Endocrine glands contain intracellular vacuoles or granules that store hormones until they are needed, allowing for rapid release in response to physiological signals.
- Furthermore, hormones produced by the endocrine system can be categorized into various chemical structures, including amino acid derivatives, steroids, eicosanoids, leukotrienes, and prostaglandins. Each of these hormone types plays distinct roles in signaling and regulation within the body.
Structure of Endocrine system
Glands of endocrine systems:
The glands of the endocrine system are specialized organs that secrete hormones directly into the bloodstream, thereby influencing a multitude of physiological processes. Each gland plays a distinct and critical role in maintaining homeostasis and regulating various bodily functions.
- Pineal Gland: This small gland is located in the brain and produces melatonin, a hormone that regulates sleep-wake cycles and circadian rhythms. Melatonin secretion is influenced by light exposure, thereby playing a vital role in synchronizing the body’s internal clock.
- Hypothalamus: Positioned below the thalamus in the brain, the hypothalamus is often considered the master regulator of the endocrine system. It produces several releasing and inhibiting hormones that control the anterior pituitary’s secretions. The hypothalamus is also integral to the autonomic nervous system and influences functions such as temperature regulation, thirst, and hunger. It operates via three main endocrine outputs: the magnocellular system, which produces oxytocin and vasopressin; the parvocellular system, which regulates anterior pituitary hormones; and autonomic intervention.
- Pituitary Gland: Known as the “master gland,” the pituitary gland is divided into the anterior and posterior sections. The anterior pituitary secretes tropic hormones, including Thyroid-Stimulating Hormone (TSH), Adrenocorticotropic Hormone (ACTH), Growth Hormone (GH), Luteinizing Hormone (LH), and Follicle-Stimulating Hormone (FSH). These hormones have widespread effects on various target organs, influencing growth, metabolism, and reproductive functions. The posterior pituitary, although it does not produce hormones, stores and releases oxytocin and vasopressin synthesized in the hypothalamus.
- Thyroid Gland: Located in the neck, the thyroid gland is responsible for producing Thyroxine (T4) and Triiodothyronine (T3), hormones that regulate metabolism, energy production, and growth. The secretion of these hormones is stimulated by TSH from the anterior pituitary, illustrating the interdependence between the hypothalamus, pituitary, and thyroid gland.
- Parathyroid Glands: These small glands, located on the posterior aspect of the thyroid gland, secrete Parathyroid Hormone (PTH), which regulates calcium levels in the blood. PTH increases blood calcium levels by promoting calcium reabsorption in the kidneys, stimulating calcium release from bones, and enhancing dietary calcium absorption in the intestines.
- Adrenal Glands: Situated atop each kidney, the adrenal glands consist of two main parts: the adrenal cortex and the adrenal medulla. The adrenal cortex produces corticosteroids, including cortisol, which is critical for stress response and metabolism, and aldosterone, which regulates sodium and potassium levels. The adrenal medulla secretes catecholamines like epinephrine and norepinephrine, which are involved in the body’s fight-or-flight response.
- Pancreas: The pancreas serves both endocrine and exocrine functions. Its endocrine component consists of clusters of cells known as the Islets of Langerhans, which include alpha cells that secrete glucagon and beta cells that secrete insulin. These hormones are pivotal in regulating blood glucose levels, with insulin lowering blood sugar and glucagon increasing it.
- Gonads (Ovaries and Testes): The ovaries in females and testes in males produce sex hormones, including estrogen and progesterone in females and testosterone in males. These hormones are essential for reproductive functions, secondary sexual characteristics, and overall health.
Cells of endocrine systems:
The endocrine system comprises a diverse array of specialized cells that collectively form various glands and tissues responsible for hormone production and regulation. Each type of cell plays a unique role in maintaining physiological balance and facilitating communication throughout the body.
- Hypothalamic Cells: Located in the hypothalamus, these neuroendocrine cells produce critical hormones that regulate the release of hormones from the pituitary gland. Two primary groups of hypothalamic cells are involved in this process:
- Magnocellular Neurons: These neurons synthesize oxytocin and vasopressin (also known as antidiuretic hormone, ADH). Oxytocin plays essential roles in childbirth and lactation, while ADH regulates water retention by the kidneys, thereby maintaining blood volume and pressure.
- Parvocellular Neurons: These neurons release hormones that regulate the anterior pituitary’s secretion, affecting various physiological processes throughout the body.
- Pituitary Cells: The pituitary gland consists of two main sections: the anterior and posterior pituitary, each containing distinct cell types.
- Anterior Pituitary Cells: This portion produces tropic hormones, including:
- Thyrotrophs: Secrete Thyroid-Stimulating Hormone (TSH), which stimulates the thyroid gland to produce T3 and T4, regulating metabolism.
- Corticotrophs: Produce Adrenocorticotropic Hormone (ACTH), which stimulates cortisol production in the adrenal cortex.
- Gonadotrophs: Secrete Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH), which regulate reproductive functions.
- Somatotrophs: Produce Growth Hormone (GH), crucial for growth, metabolism, and tissue repair.
- Anterior Pituitary Cells: This portion produces tropic hormones, including:
- Pineal Gland Cells: The pineal gland is primarily composed of pinealocytes, which synthesize and secrete melatonin, a hormone that regulates circadian rhythms and sleep patterns.
- Thyroid Gland Cells: The thyroid gland is largely made up of follicular cells that produce Thyroxine (T4) and Triiodothyronine (T3). These hormones are vital for regulating metabolic rates and influencing growth and development. The secretion of T3 and T4 is stimulated by TSH from the anterior pituitary.
- Parathyroid Gland Cells: The parathyroid glands contain chief cells that secrete Parathyroid Hormone (PTH). PTH regulates calcium levels in the blood by promoting calcium reabsorption in the kidneys, stimulating osteoclast activity in bones, and increasing intestinal calcium absorption.
- Adrenal Gland Cells: The adrenal glands are comprised of two main regions, the cortex and the medulla, each with specialized cells:
- Adrenal Cortex Cells: These cells produce corticosteroids, including cortisol (regulated by ACTH) and aldosterone, which is essential for sodium and potassium homeostasis.
- Adrenal Medulla Cells: Chromaffin cells in the adrenal medulla secrete catecholamines, such as epinephrine and norepinephrine, which mediate the body’s stress response.
- Pancreatic Cells: The pancreas houses the Islets of Langerhans, which contain several types of endocrine cells:
- Alpha Cells: These cells secrete glucagon, which increases blood glucose levels by stimulating glycogenolysis in the liver.
- Beta Cells: Comprising approximately 60% of the islet population, beta cells secrete insulin, which lowers blood glucose levels by facilitating cellular glucose uptake.
- Delta Cells: These cells produce somatostatin, which regulates the secretion of both insulin and glucagon.
- Gonadal Cells: The gonads (ovaries and testes) contain specific cell types responsible for hormone production:
- Ovarian Granulosa Cells: These cells produce estrogen and progesterone, essential for regulating the menstrual cycle and supporting pregnancy.
- Testicular Leydig Cells: Located in the testes, Leydig cells produce testosterone, which is crucial for male reproductive functions and secondary sexual characteristics.
Examples of Endocrine glands
The endocrine glands play a pivotal role in the regulation and coordination of various physiological functions in the body by secreting hormones directly into the bloodstream. This system establishes and maintains homeostasis, regulates growth and development, and enables the body to respond to environmental changes. The following points elaborate on the major endocrine glands, the hormones they produce, their molecular characteristics, target organs, and their functions.
- Hypothalamus
- Hormones: Hypothalamic releasing and inhibiting hormones
- Molecular Characteristics: Peptide
- Target Organs: Anterior pituitary
- Functions: Regulates the secretion of hormones from the anterior pituitary.
- Anterior Pituitary
- Hormones:
- Thyroid Stimulating Hormone (TSH)
- Adrenocorticotropic Hormone (ACTH)
- Gonadotropic Hormones (FSH, LH)
- Prolactin (PRL)
- Growth Hormone (GH)
- Molecular Characteristics: Glycoprotein (TSH, FSH, LH), Protein (ACTH, PRL, GH)
- Target Organs:
- Thyroid (TSH)
- Adrenal cortex (ACTH)
- Gonads (FSH, LH)
- Mammary glands (PRL)
- Soft tissues, bones (GH)
- Functions:
- Stimulates the thyroid gland (TSH)
- Stimulates adrenal cortex (ACTH)
- Promotes sex hormone production and gamete formation (FSH, LH)
- Induces milk production (PRL)
- Facilitates cell division and protein synthesis (GH)
- Hormones:
- Posterior Pituitary
- Hormones:
- Oxytocin
- Anti-diuretic Hormone (Vasopressin)
- Molecular Characteristics: Peptide
- Target Organs:
- Uterus, mammary glands (Oxytocin)
- Kidneys (Anti-diuretic Hormone)
- Functions:
- Stimulates uterine contractions and milk ejection (Oxytocin)
- Promotes water reabsorption in the kidneys (Vasopressin)
- Hormones:
- Pineal Gland
- Hormone: Melatonin
- Molecular Characteristics: Serotonin-derived
- Target Organs: Various tissues
- Functions: Regulates circadian rhythms and reproductive functions.
- Thyroid Gland
- Hormones:
- Thyroxine (T4)
- Triiodothyronine (T3)
- Calcitonin
- Molecular Characteristics: Iodinated amino acids (T4, T3), Peptide (Calcitonin)
- Target Organs:
- All tissues (T4, T3)
- Bones, kidneys, intestine (Calcitonin)
- Functions:
- Increases metabolic rate and regulates growth (T4, T3)
- Lowers blood calcium levels (Calcitonin)
- Hormones:
- Parathyroid Glands
- Hormone: Parathyroid Hormone (PTH)
- Molecular Characteristics: Peptide
- Target Organs: Bones, kidneys, intestine
- Functions: Raises blood calcium levels.
- Adrenal Glands
- Cortex:
- Hormones:
- Glucocorticoids (Cortisol)
- Mineralocorticoids (Aldosterone)
- Molecular Characteristics: Steroid
- Target Organs:
- All tissues (Cortisol)
- Kidneys (Aldosterone)
- Functions:
- Raises blood glucose levels and promotes protein breakdown (Cortisol)
- Regulates sodium and potassium balance (Aldosterone)
- Hormones:
- Medulla:
- Hormones: Epinephrine and Norepinephrine
- Molecular Characteristics: Catecholamines
- Target Organs: Cardiac and other muscles
- Functions: Facilitates the “fight or flight” response, raising blood glucose levels during stress.
- Cortex:
- Pancreas
- Hormones:
- Insulin
- Glucagon
- Somatostatin (Growth Hormone-Inhibiting Hormone)
- Molecular Characteristics: Protein
- Target Organs:
- Liver, muscles, adipose tissue (Insulin, Glucagon)
- All tissues (Somatostatin)
- Functions:
- Lowers blood glucose levels and promotes glycogen formation (Insulin)
- Raises blood glucose levels (Glucagon)
- Inhibits various physiological functions (Somatostatin)
- Hormones:
- Gastrointestinal Tract (Duodenum and Jejunum)
- Hormones:
- Secretin
- Cholecystokinin
- Molecular Characteristics: Protein
- Target Organs:
- Pancreas, stomach (Secretin)
- Gallbladder (Cholecystokinin)
- Functions:
- Regulates water homeostasis (Secretin)
- Stimulates the release of digestive enzymes and bile; acts as a hunger suppressant (Cholecystokinin)
- Hormones:
- Ovaries
- Hormones: Estrogen, Androgen, Progesterone
- Molecular Characteristics: Steroid
- Target Organs: Gonads, skin, muscles, bone
- Functions: Stimulates female secondary sex characteristics.
- Testes
- Hormone: Androgens (Testosterone)
- Molecular Characteristics: Steroid
- Target Organs: Gonads, skin, muscles, bone
- Functions: Stimulates male secondary sex characteristics.
Chemical Signaling
Chemical signaling is a fundamental process through which cells communicate, allowing them to respond effectively to changes in their environment. This mechanism, often referred to as signal transduction, involves the transmission of information from the cell surface to the cytoplasm, ultimately leading to alterations in gene expression within the nucleus. The complexity of chemical signaling encompasses a vast network of communication both between cells and within individual cells, varying significantly in purpose and response.
- Chemical Signals:
- Cells utilize a variety of chemical signals, including proteins, short peptides, amines, nucleotides, steroids, and even gases.
- These molecules are produced by signaling cells and released into the extracellular fluid, where they can interact with specific receptor proteins on target cells.
- Receptors:
- Receptors can be categorized into two main types: cell surface receptors and intracellular receptors.
- The binding of a signaling molecule to its receptor initiates a series of intracellular events, which can lead to significant cellular changes.
- Signaling Cascade Steps:
- Reception: The target cell detects a signaling molecule outside its membrane.
- Transduction: The binding event alters the three-dimensional structure of the receptor, triggering a series of downstream signaling events.
- Response: The final output of this cascade is a specific cellular response, which may include changes in gene expression, enzyme activity, or cellular metabolism.
- Cell-Specific Responses:
- While a cell is exposed to numerous signaling molecules, its response is determined by the specific receptors it possesses.
- If a cell lacks a receptor for a particular signal, it cannot respond to that signal.
- Different cells express unique sets of receptors, allowing them to respond selectively to various signals.
- Diversity of Responses:
- A single signaling molecule can produce multiple effects in a target cell, depending on the context.
- Additionally, the same signal may elicit different responses in different cell types, reflecting the importance of cellular context in signaling.
- Cells can also integrate multiple signals simultaneously, allowing for nuanced responses based on the combination of signals received.
- Modes of Cell Signaling:
- Local Signaling:
- Cell-Cell Contact: This requires direct interaction between membrane proteins of adjacent cells.
- Gap Junctions: These structures allow for direct cytoplasmic connections between neighboring cells, facilitating rapid communication.
- Autocrine Signaling: In this mode, a cell produces a signaling molecule that it can also respond to, creating a self-regulatory mechanism.
- Paracrine Signaling: Here, a signaling molecule released by one cell diffuses locally to affect nearby target cells. For example, cytokines released during inflammation and neurotransmitters at synapses exemplify this mode.
- Long-Distance Signaling:
- Endocrine Signaling: Hormones are secreted into the bloodstream and travel through the circulatory system to distant target cells, allowing for systemic effects.
- Neural Signaling: In this type of signaling, neurotransmitters are released from the axon terminal of a presynaptic neuron and bind to receptors on the dendrites of a postsynaptic neuron, enabling rapid communication over long distances.
- Local Signaling:
Chemical classification of hormones
The classification of hormones based on their chemical properties is essential for understanding their synthesis, storage, mechanism of action, and physiological effects. Hormones can be grouped primarily by their solubility, which affects how they interact with target cells and their biological functions.
- Functional Classification:
- Hormones can be classified according to their action in target cells:
- Surface-acting Hormones: These hormones do not penetrate the cell membrane. Instead, they interact with receptors located on the cell surface. Examples include polypeptide hormones such as growth hormone, monoamines like serotonin, and prostaglandins like prostaglandin E2.
- Intracellular Hormones: These hormones can cross the cell membrane and bind to intracellular receptors, typically found in the cytoplasm or nucleus. Classic examples include steroid hormones and thyroid hormones, which regulate gene expression.
- Hormones can be classified according to their action in target cells:
- Chemical Classification:
- Hormones can also be categorized based on their chemical nature into two major groups:
- Lipid-soluble Hormones:
- Comprising steroid hormones (e.g., cortisol) and lipids (e.g., prostaglandins).
- Their lipophilic nature allows them to pass through cell membranes easily.
- Water-soluble Hormones:
- Including protein, peptide, catecholamine, and amino acid-derived hormones.
- These hormones typically signal through transmembrane receptors due to their hydrophilic nature.
- Lipid-soluble Hormones:
- Hormones can also be categorized based on their chemical nature into two major groups:
- Impact of Chemical Nature:
- The chemical structure of a hormone dictates several key aspects of its biology:
- The method of synthesis and storage within endocrine glands.
- The mechanism of release into circulation and transport in the bloodstream.
- The biological half-life, mode of clearance, and overall mechanism of action on target cells.
- The chemical structure of a hormone dictates several key aspects of its biology:
- Protein and Peptide Hormones:
- These hormones can be classified further based on their amino acid chain length:
- Protein Hormones: Comprising 50 or more amino acids (e.g., adrenocorticotropin).
- Peptide Hormones: Consisting of two or more amino acids (e.g., vasopressin).
- Monoamines: Derived from the amino acid tyrosine (e.g., norepinephrine).
- Amino Acid Derivatives: Such as triiodothyronine.
- Key features include:
- Synthesized as prehormones or preprohormones.
- Hydrophilic, signaling through transmembrane receptors.
- Stored in membrane-bound secretory vesicles until released.
- Released via exocytosis in response to specific stimuli.
- Predominantly circulate in the bloodstream in an unbound form.
- These hormones can be classified further based on their amino acid chain length:
- Receptors for Protein Hormones:
- Protein and peptide hormones bind to receptors embedded in the target cell membrane, characterized by three domains:
- Extracellular Domain: Contains the ligand-binding site and protrudes outside the cell.
- Transmembrane Domain: Anchors the receptor within the plasma membrane.
- Intracellular Domain: Resides within the cytoplasm, triggering intracellular signaling cascades upon hormone binding.
- The binding of a hormone to its receptor initiates a conformational change, leading to signal transduction via second messengers such as cAMP and calcium ions. This process allows even a minute quantity of hormone to amplify cellular responses, which can manifest in seconds to minutes.
- Protein and peptide hormones bind to receptors embedded in the target cell membrane, characterized by three domains:
- Steroid Hormones:
- These hormones are synthesized from cholesterol and include diverse classes:
- Progestins: 21-carbon steroids.
- Corticosteroids: 21-carbon steroids.
- Androgens: 19-carbon steroids (male sex steroids).
- Estrogens: 18-carbon steroids (female sex steroids).
- Characteristics include:
- Being lipophilic, requiring protein carriers for transport in the bloodstream.
- Unable to be stored in secretory vesicles due to their lipid solubility.
- Synthesized from cholesterol obtained from the extracellular environment or produced intracellularly.
- These hormones are synthesized from cholesterol and include diverse classes:
- Receptors for Steroid Hormones:
- Steroid hormone receptors are located within the cytoplasm or nucleus of target cells.
- Upon hormone binding, a conformational change occurs in the receptor, revealing a DNA-binding domain that interacts with specific regions of steroid-responsive genes.
- This interaction regulates gene transcription, influenced by various cofactors present in different cell types. Consequently, the same hormone can elicit varied effects across different cells.
- The action of steroid hormones typically requires more time (at least 30 minutes) to manifest, as they initiate transcription and translation processes, resulting in long-lasting physiological effects.
Transport and metabolism of hormones
The transport and metabolism of hormones are vital processes that ensure hormones effectively reach their target cells and elicit appropriate physiological responses. Once synthesized by endocrine cells, hormones undergo a series of events before they can exert their biological effects. Understanding these processes provides insight into the regulation and action of hormones within the body.
- Secretion of Hormones:
- After production, hormones must be secreted from the endocrine cells.
- Steroid and thyroid hormones, being hydrophobic, cannot circulate freely in the bloodstream. Instead, they require specific binding proteins to facilitate their transport.
- Conversely, protein and peptide hormones, which are hydrophilic and water-soluble, can circulate in the bloodstream without the need for binding proteins.
- Binding Proteins for Lipid-soluble Hormones:
- Certain hormones, such as steroid and thyroid hormones, rely on specific serum binding proteins for circulation, including:
- Corticosteroid-binding globulin (CBG).
- Thyroxine-binding globulin (TBG).
- Sex hormone-binding globulin (SHBG).
- Vitamin D-binding protein.
- These proteins serve to solubilize the hormones in the plasma and extend their half-life by preventing rapid degradation.
- Certain hormones, such as steroid and thyroid hormones, rely on specific serum binding proteins for circulation, including:
- Storage and Release of Protein/Peptide Hormones:
- Protein and peptide hormones, unlike their lipid-soluble counterparts, are synthesized and stored in membrane-bound secretory vesicles within endocrine cells.
- For instance, insulin is produced in pancreatic β-cells and is released in response to stimuli, such as elevated blood glucose levels.
- Upon secretion, these hormones generally do not bind to carrier proteins in the bloodstream and are instead directly soluble in aqueous environments.
- Half-life and Stability:
- The half-life of a hormone in circulation is influenced by its binding status:
- Protein and peptide hormones typically have shorter half-lives due to their rapid degradation by serum proteases.
- In contrast, steroid and thyroid hormones exhibit longer half-lives as they are protected from degradation while bound to their carrier proteins.
- Some protein and peptide hormones, such as growth hormone (GH) and insulin-like growth factors (IGF-1 and IGF-2), may circulate with binding proteins, prolonging their half-lives.
- The half-life of a hormone in circulation is influenced by its binding status:
- Hormone Clearance Mechanisms:
- The concentration of hormones in the plasma is regulated by both the rate of synthesis and secretion from endocrine glands and the rate of removal from circulation.
- Key organs involved in the excretion and metabolism of hormones include:
- Liver: Plays a significant role in metabolizing hormones.
- Kidneys: Essential for the excretion of hormonal metabolites.
- Hormones may also be removed via endocytosis, where hormone-receptor complexes are internalized by target cells, allowing for rapid degradation within the cell.
- Enzymatic Breakdown:
- Certain enzymes in the bloodstream facilitate the breakdown of hormones, which can contribute to their clearance.
- The metabolism of steroid and thyroid hormones tends to be slower, often taking hours to days, because their binding proteins shield them from immediate degradation.
Characteristic of Hormones
Here are the key characteristics of hormones:
- Chemical Composition:
- Hormones can be classified based on their chemical structure. They include:
- Peptide Hormones: Composed of chains of amino acids (e.g., insulin, glucagon).
- Steroid Hormones: Derived from cholesterol and lipid-soluble (e.g., cortisol, estrogen, testosterone).
- Amine Hormones: Derived from amino acids (e.g., epinephrine, norepinephrine, thyroid hormones).
- Hormones can be classified based on their chemical structure. They include:
- Specificity:
- Hormones act on specific target cells or tissues that possess the appropriate receptors. This specificity ensures that the effects of hormones are precise and context-dependent.
- Mechanism of Action:
- Hormones exert their effects by binding to receptors on target cells, which can be located on the cell membrane (for peptide hormones) or within the cell (for steroid hormones). This binding initiates a cascade of biochemical events, leading to a specific physiological response.
- Regulation and Feedback Mechanisms:
- Hormone levels are tightly regulated through feedback loops:
- Negative Feedback: Most hormonal systems operate via negative feedback, where an increase in hormone levels inhibits further production. For example, increased blood glucose levels stimulate insulin secretion, which lowers blood glucose, thus reducing further insulin release.
- Positive Feedback: Some hormonal responses are governed by positive feedback, where an increase in hormone levels promotes further secretion. An example is oxytocin during childbirth, which increases contractions, leading to more oxytocin release.
- Hormone levels are tightly regulated through feedback loops:
- Pulsatile Secretion:
- Many hormones are secreted in a pulsatile manner, meaning their release occurs in bursts rather than continuously. This pattern helps prevent desensitization of target cells and ensures an appropriate response to physiological needs.
- Half-Life:
- Hormones vary in their half-lives, which is the time taken for half of the hormone to be metabolically inactivated or eliminated from the body. Hormones with short half-lives, such as epinephrine, act quickly but require frequent secretion, while those with longer half-lives, such as cortisol, have prolonged effects.
- Physiological Effects:
- Hormones regulate numerous bodily functions, including:
- Metabolism
- Growth and development
- Reproductive processes
- Homeostasis (e.g., fluid balance, electrolyte levels)
- Response to stress and environmental changes
- Hormones regulate numerous bodily functions, including:
- Interaction with Other Hormones:
- Hormones often interact with each other, leading to synergistic, antagonistic, or permissive effects. For example, cortisol can enhance the effect of glucagon on blood sugar levels, while insulin acts to lower them.
- Site of Action:
- Hormones can act locally (paracrine signaling) or at distant sites (endocrine signaling). This characteristic allows for both localized responses in tissues and systemic regulation of physiological processes.
What are Neurohormones?
Neurohormones are a specific type of hormone produced and released by neurosecretory cells in the nervous system. Unlike traditional hormones that are secreted by endocrine glands, neurohormones are synthesized in neurons and released into the bloodstream or interstitial fluid, where they can exert effects on distant target cells or organs. Here are key aspects of neurohormones:
- Synthesis and Release:
- Neurohormones are typically synthesized in the cell body of a neuron and transported along its axon to storage sites. When the neuron is activated, these neurohormones are released into the blood or surrounding tissues in response to various stimuli.
- Examples of Neurohormones:
- Some well-known neurohormones include:
- Oxytocin: Produced in the hypothalamus and released from the posterior pituitary gland, it plays roles in social bonding, reproductive behaviors, and uterine contractions during childbirth.
- Vasopressin (Antidiuretic Hormone, ADH): Also produced in the hypothalamus and released from the posterior pituitary, vasopressin regulates water balance in the body by promoting water reabsorption in the kidneys.
- Corticotropin-Releasing Hormone (CRH): Synthesized in the hypothalamus, CRH stimulates the release of adrenocorticotropic hormone (ACTH) from the anterior pituitary, which in turn stimulates cortisol release from the adrenal glands.
- Some well-known neurohormones include:
- Mechanism of Action:
- Neurohormones exert their effects by binding to specific receptors on target cells, triggering a cascade of cellular responses. These responses can include changes in gene expression, alterations in cellular metabolism, and modifications in the activity of other hormones.
- Function and Regulation:
- Neurohormones play critical roles in various physiological processes, including:
- Stress Response: They help regulate the body’s reaction to stress by influencing the hypothalamic-pituitary-adrenal (HPA) axis.
- Reproductive Functions: They are involved in reproductive behaviors, such as the initiation of labor and lactation.
- Fluid Balance: They maintain homeostasis by regulating water retention and electrolyte balance.
- The secretion of neurohormones is often regulated by feedback mechanisms, ensuring that hormone levels remain within a specific range to maintain physiological balance.
- Neurohormones play critical roles in various physiological processes, including:
- Neuroendocrine Interaction:
- Neurohormones exemplify the integration of the nervous and endocrine systems, facilitating communication between these two systems. This interaction is essential for coordinating complex bodily functions, such as growth, metabolism, and response to environmental changes.
What is Neurosecretions?
Neurosecretions refer to the release of hormones and other signaling molecules from specialized neurons, particularly those in the neuroendocrine system. This process involves the synthesis, storage, and secretion of these substances, which play critical roles in regulating various physiological functions. The following points outline the key aspects of neurosecretions:
- Origin: Neurosecretions are primarily produced by neurosecretory cells, which are neurons that have the ability to synthesize hormones and release them into the bloodstream or interstitial fluid. This process occurs mainly in specific regions of the brain, such as the hypothalamus.
- Types of Neurosecretions: The two main types of neurosecretions are:
- Hormones: These are chemical messengers that are secreted into the bloodstream and travel to distant target organs or tissues to elicit specific physiological responses. Examples include oxytocin and vasopressin (antidiuretic hormone), both produced in the hypothalamus.
- Neurotransmitters: These are signaling molecules released at synapses to communicate between neurons. While neurotransmitters generally act locally, some can also have systemic effects when released by neurosecretory cells.
- Mechanism of Action: Neurosecretions involve several steps:
- Synthesis: Neurosecretory cells synthesize hormones or neurotransmitters from precursor molecules.
- Storage: The synthesized substances are often stored in vesicles until they are needed.
- Release: Upon receiving specific signals (e.g., neural stimulation, changes in blood composition), neurosecretory cells release their contents into the bloodstream or synaptic cleft.
- Regulation: The release of neurosecretions is tightly regulated by feedback mechanisms, often involving interactions with other hormones or physiological conditions. For example, the hypothalamus secretes releasing and inhibiting hormones that control the activity of the anterior pituitary gland.
- Functions: Neurosecretions play a vital role in various bodily functions, including:
- Regulating the body’s stress response (e.g., through corticotropin-releasing hormone, which stimulates the release of adrenocorticotropic hormone from the pituitary).
- Controlling water balance (e.g., through the release of vasopressin, which promotes water reabsorption in the kidneys).
- Influencing reproductive processes (e.g., through gonadotropin-releasing hormone, which stimulates the release of luteinizing hormone and follicle-stimulating hormone).
- Neuroendocrine System: The concept of neurosecretions is integral to understanding the neuroendocrine system, which links the nervous and endocrine systems. This integration allows for a coordinated response to various stimuli, maintaining homeostasis and regulating complex physiological processes.
Functions of Endocrine system
Below are the primary functions of the endocrine system:
- Regulation of Metabolism: Hormones such as insulin and glucagon from the pancreas regulate blood glucose levels, thereby influencing energy metabolism. Thyroid hormones (T3 and T4) also play a vital role in metabolic rate and energy expenditure.
- Growth and Development: Growth Hormone (GH) from the anterior pituitary stimulates growth in tissues and bones. Additionally, sex hormones, such as estrogen and testosterone, are crucial for the development of secondary sexual characteristics and reproductive organs during puberty.
- Homeostasis of Blood Composition: Hormones regulate key parameters such as blood glucose, calcium, and electrolyte levels. For example, Parathyroid Hormone (PTH) maintains calcium homeostasis by acting on bones, kidneys, and the intestines, while aldosterone from the adrenal cortex regulates sodium and potassium levels.
- Stress Response: The adrenal glands produce hormones like cortisol and adrenaline (epinephrine), which prepare the body for a “fight or flight” response during stressful situations. These hormones increase heart rate, blood pressure, and energy availability.
- Reproductive Function: The endocrine system regulates reproductive processes through sex hormones. In females, estrogen and progesterone regulate the menstrual cycle and pregnancy. In males, testosterone is essential for sperm production and the development of male traits.
- Regulation of Water and Electrolyte Balance: Antidiuretic Hormone (ADH), produced by the hypothalamus and stored in the posterior pituitary, helps the kidneys conserve water, thereby influencing blood volume and pressure. Aldosterone also contributes by regulating sodium retention.
- Control of Mood and Cognitive Functions: Hormones can influence mood, behavior, and cognitive functions. For example, serotonin, although primarily produced in the gastrointestinal tract, is linked to mood regulation, while cortisol affects stress responses and can impact mood.
- Immune Function Regulation: Certain hormones, such as thymosin produced by the thymus gland, are involved in the development and regulation of the immune system. Hormonal signals can enhance or suppress immune responses.
- Circadian Rhythms: The endocrine system regulates the sleep-wake cycle through melatonin produced by the pineal gland. Melatonin secretion increases in darkness, promoting sleep, and decreases in light, helping regulate circadian rhythms.
- Adaptation to Environmental Changes: Hormones enable the body to adapt to various environmental conditions, such as temperature changes or nutritional status. For instance, the endocrine response to cold includes the secretion of thyroid hormones to increase metabolic activity and generate heat.
- https://egyankosh.ac.in/bitstream/123456789/81429/3/Block-1.pdf
- https://www.news-medical.net/health/Endocrinology-History.aspx
- https://resident360.nejm.org/content-items/history-of-endocrinology
- https://en.wikipedia.org/wiki/Endocrinology
- https://en.wikipedia.org/wiki/Endocrine_system