| Kingdom: | Fungi |
| Division: | Ascomycota |
| Class: | Saccharomycetes |
| Order: | Saccharomycetales |
| Family: | Saccharomycetaceae |
| Genus: | Candida |
| Species: | C. glabrata |
What is Candida glabrata?
- Previously known as Torulopsis glabrata, Candida glabrata is a species of haploid yeast in the genus Candida. Despite the fact that this species’ sexual life cycle has not been documented, both mating forms of C. glabrata strains are commonly found.
- C. glabrata is typically a commensal of human mucosal tissues; however, in the current era of widespread human immunodeficiency due to various causes (such as therapeutic immunomodulation, longer survival with various comorbidities such as diabetes, and HIV infection), C. glabrata is frequently the second or third most common opportunistic pathogen causing candidiasis.
- In immunocompromised patients, C. glabrata infections can affect the urogenital tract or even induce systemic infections through the entry of fungal cells into the bloodstream (Candidemia).
- Candida glabrata is of particular importance in nosocomial infections due to its inherent resistance to antifungal agents, particularly the azoles.
- In addition to its inherent tolerance to antifungal drugs, other putative virulence factors contribute to the pathogenicity of C. glabrata.
- The expression of a series of adhesins genes is one of them.The expression of these genes, which in C. glabrata are predominantly encoded in the subtelomeric region of the chromosome, is highly induced by environmental stimuli, allowing the organism to adhere to biotic and abiotic surfaces in microbial mats.
- Adhesin expression, which is believed to be the first mechanism by which C. glabrata forms fungal biofilms, was found to be more antifungal-resistant than planktonic cells.
- The genome of Candida glabrata undergoes frequent rearrangements that are hypothesized to contribute to the enhancement of this yeast’s fitness in response to exposure to stressful conditions, and some authors believe that this property is associated with the virulence potential of this yeast.
Habitat of Candida glabrata
Candida glabrata is a common yeast found in a variety of habitats, including human hosts and the environment. Here are the principal environments in which Candida glabrata is found:
- Human Body: Candida glabrata is an opportunistic pathogen that is capable of colonizing various areas of the human body. It is prevalent in the digestive tract, oral cavity, respiratory tract, and female genital tract. Additionally, it can be found on the epidermis, especially in moist areas such as the armpits and groin.
- Hospital Environments: Candida glabrata is frequently linked to hospital-acquired infections, especially in immunocompromised patients or those undergoing invasive medical procedures. It can colonize catheters, intravenous lines, and central venous catheters.
- Water Sources: Candida glabrata has been isolated from a variety of water sources, including tap water, potable water, and natural bodies of water such as rivers and lakes. It can endure and persist in water environments, making it a potential source of infection.
- Plants and Soil: Candida glabrata has been detected on the surfaces of plants and sediment. It is not as prevalent in these habitats as it is in the human body or hospital settings, but studies have uncovered its presence.
- Animals: Candida glabrata has been isolated from animals, including domesticated pets and livestock. It can colonize the epidermis, ear canals, and mucosal surfaces of animals, just as it does with humans.
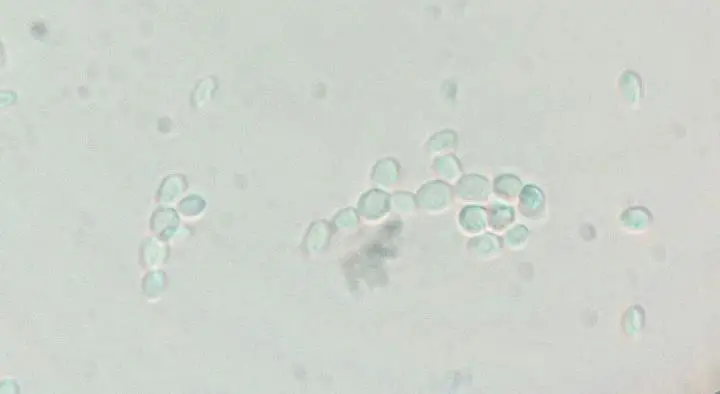
Morphology of Candida glabrata
Candida glabrata is a yeast species belonging to the genus Candida. Here is a description of Candida glabrata’s morphology:
- Cellular Shape: Candida glabrata cells are typically ovoid or spherical in shape, similar to other yeast cells. When dividing, it may appear as single cells or form brief chains or clusters.
- Size: In general, the diameter of Candida glabrata cells ranges between 2 and 4 micrometers.
- Cell Wall: Candida glabrata, like other Candida species, has a cell wall composed of carbohydrates, proteins, and lipids. The yeast cell’s cell wall provides structural support and protection.
- Budding: Candida glabrata reproduces asexually by means of branching. A small outgrowth or bud forms on the parent cell during budding, progressively enlarges, and eventually separates to become a new cell.
- Yeast form: The yeast form of C. glabrata is small, spherical cells that are about 2-3 micrometers in diameter. They are non-motile and reproduce by budding.
- Pseudohyphae Formation: Under certain conditions, Candida glabrata can form pseudohyphae, which are chains of attached, elongated cells. It should be noted, however, that Candida glabrata is predominately a non-filamentous yeast and does not typically form genuine hyphae like other Candida species. The pseudohypha form of C. glabrata is elongated cells that are about 5-10 micrometers in length. They are also non-motile and reproduce by budding.
- Color and Staining: Candida glabrata cells are typically transparent and colorless. To improve their visibility under a microscope, they can be stained with various laboratory dyes, such as Gram stain or fungal stains such as calcofluor white.
| Morphological Characteristic | Description |
|---|---|
| Cellular Shape | Oval or spherical cells |
| Size | Approximately 2 to 4 micrometers in diameter |
| Cell Wall | Composed of carbohydrates, proteins, and lipids |
| Reproduction Method | Asexual reproduction through budding |
| Pseudohyphae Formation | Can form chains of elongated cells (pseudohyphae) |
| Filamentous Growth | Predominantly non-filamentous, does not form true hyphae |
| Color and Staining | Colorless and transparent, can be stained with dyes |
Pathogenesis of Candida glabrata
Candida glabrata is an opportunistic fungal pathogen that can infect humans, especially those with compromised immune systems or underlying medical conditions. Pathogenesis of Candida glabrata is characterized by a complex interaction between host factors and virulence characteristics of the fungus. Here are some important aspects of Candida glabrata’s pathogenesis:
- Adherence and Colonization: Candida glabrata possesses adhesion molecules on its cell surface that allow it to adhere to host tissues, such as epithelial cells, and colonize them. This initial adherence permits the fungus to colonize and establish infection in various sites, including the epidermis, oral cavity, digestive tract, and genitourinary system.
- Invasion of host cells: C. glabrata can invade host cells through a number of mechanisms, including the production of enzymes that break down the cell wall and the use of surface receptors to enter the cell.
- Immune Evasion: Candida glabrata has mechanisms to evade host immune responses. It modulates the host immune system by interfering with phagocytosis, inhibiting complement activation, and inhibiting the production of specific immune molecules. This evasion may allow the fungus to persist and cause persistent or recurrent infections. C. glabrata can evade the immune system through a number of mechanisms, including the production of surface proteins that mask the fungus from the immune system and the production of enzymes that destroy immune cells.
- Biofilm Formation: Candida glabrata is capable of forming biofilms, which are complex communities of microorganisms surrounded by a protective matrix. Infections are more difficult to treat as a result of biofilms’ increased resistance to antifungal agents and host immune defenses. Candida glabrata biofilms are frequently linked to infections caused by medical devices, such as catheter-associated urinary tract infections.
- Antifungal Resistance: Candida glabrata is notorious for its inherent or acquired resistance to several antifungal medications, including azoles, that are commonly used for treatment. This resistance can restrict treatment options and make the management of Candida glabrata infections more complicated.
- Virulence Factors: Candida glabrata produces numerous virulence factors that contribute to its pathogenesis. Included in this category are proteases, which can degrade host tissues and facilitate invasion, as well as phospholipases and hemolysins, which can damage host cell membranes and cause tissue injury.
- Host Susceptibility: Candida glabrata infections are more prevalent in patients with immunosuppression (e.g., HIV/AIDS, organ transplantation, chemotherapy), protracted use of broad-spectrum antibiotics, diabetes, and indwelling medical devices.
- Site-Specific Infections: Candida glabrata is capable of causing a variety of infections, including bloodstream infections (candidemia), urinary tract infections, vaginal infections (vulvovaginal candidiasis), oral infections (thrush), and invasive candidiasis in multiple organs.
Virulence Factors of Candida glabrata
- Adhesins: C. glabrata produces a number of adhesins, which are proteins that allow the fungus to adhere to host cells. These adhesins include:
- C. glabrata agglutinin (CagA): CagA is a cell surface adhesin that binds to epithelial cells.
- Adhesin cell-like protein (ACLP): ACLP is a cell surface adhesin that binds to fibronectin.
- Fibronectin-binding adhesin (Fba): Fba is a cell surface adhesin that binds to fibronectin.
- Surface receptors: C. glabrata also has a number of surface receptors that allow it to interact with host cells. These receptors include:
- Dectin-1 receptor: Dectin-1 is a receptor that binds to β-glucans, which are components of the fungal cell wall.
- β-glucan receptor: β-glucan receptor is a receptor that binds to β-glucans.
- Enzymes: C. glabrata produces a number of enzymes that can damage host cells. These enzymes include:
- Proteases: Proteases are enzymes that break down proteins. C. glabrata produces a number of proteases, including:
- Aspartyl protease: Aspartyl protease is a protease that breaks down aspartic acid residues in proteins.
- Cysteine protease: Cysteine protease is a protease that breaks down cysteine residues in proteins.
- Serine protease: Serine protease is a protease that breaks down serine residues in proteins.
- Phospholipases: Phospholipases are enzymes that break down phospholipids. C. glabrata produces a number of phospholipases, including:
- Phospholipase A2: Phospholipase A2 is a phospholipase that breaks down phospholipids.
- Phospholipase C: Phospholipase C is a phospholipase that breaks down phospholipids.
- Hemolysins: Hemolysins are enzymes that break down red blood cells. C. glabrata produces a number of hemolysins, including:
- Candidalysin: Candidalysin is a hemolysin that breaks down red blood cells.
- Saprophyticuslysin: Saprophyticuslysin is a hemolysin that breaks down red blood cells.
- Proteases: Proteases are enzymes that break down proteins. C. glabrata produces a number of proteases, including:
- Resistance to antifungal medications: C. glabrata is more likely to be resistant to antifungal medications than other Candida species. This is due to a number of factors, including:
- The ability of C. glabrata to develop resistance to antifungal medications through mutation.
- The ability of C. glabrata to acquire resistance genes from other fungi.
Clinical Manifestations of Candida glabrata
Candida glabrata is a pathogenic yeast that can produce a variety of clinical symptoms in humans. Candida glabrata infections can manifest clinically differently depending on the site of infection and the individual’s immune status. The following are some prevalent clinical manifestations of Candida glabrata:
- Vulvovaginal Candidiasis (VVC): Candida glabrata can cause vaginal infections in women, resulting in symptoms such as vaginal itching, burning, redness, swelling, and aberrant vaginal discharge (Vulvovaginal Candidiasis, or VVC). Candida glabrata-induced VVC is frequently more resistant to antifungal treatment than VVC caused by other Candida species. Vulvovaginal candidiasis symptoms can range from mild to severe. Mild symptoms may include itching, stinging, and a white discharge resembling cottage cheese. Severe symptoms may include vaginal and vulvar irritation, swelling, and redness.
- Oral Thrush: Candida glabrata is capable of infecting the buccal cavity, resulting in oral thrush. This condition is characterised by the appearance of white, creamy regions on the tongue, inner cheeks, palate, and other areas of the mouth. Pain, difficulty ingesting, and altered taste perception may accompany this condition.
- Urinary Tract Infections (UTIs): Candida glabrata is a frequent cause of urinary tract infections (UTIs), particularly in patients with indwelling urinary catheters or other urinary tract abnormalities. Candida glabrata urinary tract infections are characterised by frequent urination, urgency, dysuria (painful urination), turbid urine, and hematuria (blood in urine).
- Candidemia: Candida glabrata is a major source of bloodstream infections (candidemia). It can infiltrate the bloodstream through other sites of infection or intravascular devices. Candidemia can cause fever, shivers, hypotension (low blood pressure), organ dysfunction, and disseminated infection to organs including the liver, spleen, and kidneys.
- Surgical Site Infections (SSI): Candida glabrata can cause surgical site infections, particularly in patients undergoing abdominal or gastrointestinal surgery. Infections at the surgical site may manifest as wound redness, edoema, pain, drainage, and delayed wound healing.
- Systemic Infections: Candida glabrata can cause invasive candidiasis, which entails the spread of the infection to multiple organs, in immunocompromised individuals. Systemic infections can cause fever, sepsis, endocarditis, meningitis, and other severe complications.
Clutural Characteristics of Candida glabrata
Colony Characteristics of Candida glabrata
- Colonies on Sabouraud dextrose agar (SDA) are uniform and cream-colored.
- Colonies develop at 42 degrees Celsius.
- Germ cells are not produced by colonies.
- Colonies do not form pseudohyphae.
- Colonies are oxidase negative.
- Colonies are catalase positive.
- Colonies ferment glucose, maltose, and sucrose.
- Colonies do not metabolise lactose.
- Colonies are resistant to fluconazole.
- Colonies are susceptible to voriconazole.
Cultural characteristics of Candida glabrata
- Colonies on SDA: Candida glabrata colonies on SDA are white and silky. After twenty-four hours, their diameter is approximately 1-2 millimetres.
- Growth at 42 degrees Celsius: Candida glabrata can grow at 42 degrees Celsius. This distinguishes it from other species of Candida, such as Candida albicans, which cannot thrive at 42 degrees Celsius.
- Germ tubes: Candida glabrata does not produce germ tubes. Germ tubes are protrusions that form from yeast cells and aid in the spread of fungi.
- Colonies Texture: The colonies often have a moist or shiny texture.
- Colonies Color: Candida glabrata colonies can vary in color, ranging from creamy white to light pink or pale yellow.
- Pseudohyphae: Candida glabrata does not form pseudohyphae. Pseudohyphae are yeast cells that are elongated and connected by thin filaments.
- Oxidase: Candida glabrata is oxidase negative. Oxidase is an enzyme used to metabolise oxygen. Candida glabrata is incapable of producing oxidase, so it will not react to an oxidase test.
- Catalase: Candida glabrata is catalase positive. Catalase is an enzyme utilised in the destruction of hydrogen peroxide. Candida glabrata produces catalase, so it will produce bubbles during a catalase test.
- Fermentation: Candida glabrata ferments glucose, maltose, and sucrose. During fermentation, yeast cells transform carbohydrates into alcohol and carbon dioxide. Candida glabrata is able to ferment these carbohydrates, providing it with an energy source.
- Lactose fermentation: Candida glabrata does not ferment lactose. Lactose is a type of sugar present in milk. Candida glabrata is incapable of fermenting lactose, so it cannot thrive on lactose-containing media.
- Resistance to fluconazole: Candida glabrata is resistant to fluconazole. Fluconazole is a popular antifungal medication used to treat candidiasis. However, Candida glabrata is frequently resistant to fluconazole, making treatment more challenging.
- Susceptibility to voriconazole: Candida glabrata is susceptible to voriconazole. Voriconazole is an antifungal medication frequently used to treat fluconazole-resistant candidiasis.
Optimum Growth Conditions:
- Temperature: Candida glabrata grows well at human body temperature, which is around 37°C (98.6°F).
- pH: The optimum pH for Candida glabrata growth is slightly acidic to neutral, ranging from pH 5.0 to 7.0.
- Oxygen Requirements: Candida glabrata is a facultative anaerobe, meaning it can grow in both aerobic (with oxygen) and anaerobic (without oxygen) conditions. However, it generally prefers aerobic conditions.
- Incubation Time: Candida glabrata cultures are typically incubated for 24 to 48 hours to allow sufficient time for visible growth and colony development.
Media Used for Growth
- Sabouraud Dextrose Agar (SDA): SDA is a commonly used medium for the cultivation of Candida species, including Candida glabrata. It contains dextrose and peptones that support fungal growth.
- Chromogenic Agar: Chromogenic media, such as CHROMagar Candida, are also used to facilitate the identification of Candida species. These selective and differential media contain chromogenic substrates that produce characteristic colony colors for different Candida species, aiding in their differentiation.
Laboratory Diagnosis of Candida glabrata
Several methods are used to identify and confirm the presence of Candida glabrata in clinical specimens during the laboratory diagnosis of Candida glabrata. Here are some typical laboratory procedures used to diagnose Candida glabrata:
- Microscopic Examination: Clinical specimens, such as vaginal samples, urine, or other bodily fluids, can be examined microscopically for initial indications of the presence of Candida species. Direct microscopy employing a potassium hydroxide (KOH) solution or Gramme staining can reveal the yeast cells and budding forms of Candida glabrata. However, microscopic examination alone is insufficient to conclusively identify Candida glabrata and is frequently followed by additional tests.
- Culture: Culture is the method of choice for isolating and identifying Candida species, including Candida glabrata. Clinical specimens, including biopsies, urine, blood, and tissue samples, can be cultured on specific fungal culture media, such as Sabouraud agar and chromogenic agar. On these media, Candida glabrata typically forms uniform, cream-colored colonies. Biochemical assays or automated identification systems can be used to identify individuals further.
- Biochemical Tests: Biochemical tests, such as carbohydrate assimilation assays (e.g., using the API 20C system) or enzymatic tests, can assist in distinguishing Candida glabrata from other Candida species. Frequently, Candida glabrata exhibits biochemical profiles that facilitate its identification.
- Chromogenic Media: Chromogenic media, such as CHROMagar Candida, use specific chromogenic substrates to distinguish Candida species based on colony colour. Candida glabrata colonies on CHROMagar Candida typically appear pallid or pink, which aids in distinguishing it from other Candida species.
- Molecular Methods: Molecular methods, such as polymerase chain reaction (PCR), can be used to identify Candida glabrata quickly and precisely. PCR assays can accurately and rapidly identify the species by targeting specific genetic regions of the Candida genome.
- Antifungal Susceptibility Testing: The purpose of antifungal susceptibility testing is to determine the susceptibility of Candida glabrata isolates to various antifungal drugs. This testing aids in guiding treatment decisions. Using standardised techniques, such as the broth microdilution method, the minimum inhibitory concentration (MIC) of antifungal agents such as azoles and echinocandins is determined.
Treatment of Candida glabrata infections
Candida glabrata infections are typically treated with antifungal medications. The choice of antifungal agent depends on the infection’s severity and location. Here are some typical therapeutic options:
- Fluconazole: Fluconazole is an antifungal drug that is frequently used as the initial treatment for Candida glabrata infections. However, it is important to observe that some Candida glabrata strains may be fluconazole-resistant.
- Echinocandins: Echinocandins, including caspofungin, micafungin, and anidulafungin, are an antifungal drug class that is efficacious against Candida glabrata and other Candida species. They function by preventing the development of the fungal cell wall. When fluconazole is ineffective or when infections are severe, echinocandins are frequently used as an alternative therapy.
- Amphotericin B: Amphotericin B is a potent antifungal agent used to treat severe Candida glabrata infections, particularly those involving the circulation. It is typically administered intravenously and may be combined with other antifungal drugs.
- Combination therapy: In certain instances, a combination of antifungal medications may be prescribed to enhance efficacy or combat drug resistance. For instance, an echinocandin and fluconazole combination may be used to treat severe or recurrent Candida glabrata infections.
Prevention and Control of Candida glabrata infections
Prevention and control of Candida glabrata infections entail a number of measures that can reduce the likelihood of infection or its recurrence. Here are some strategies:
- Good hygiene practices: Good hygiene is essential for the prevention of Candida glabrata infections. This includes frequent handwashing with soap and water, particularly before and after handling medical devices or touching potentially infectious areas.
- Catheter care: If you have a urinary catheter or any other type of indwelling catheter, it is crucial to adhere to appropriate catheter care protocols to reduce the risk of infection. This includes practising good hygiene, cleaning the catheter insertion site on a regular basis, and reporting any symptoms of infection to your healthcare provider immediately.
- Antibiotic stewardship: Candida glabrata infections are frequently associated with a history of antibiotic use. Antibiotics can disrupt the natural equilibrium of microorganisms in the body, permitting Candida species to proliferate. Therefore, it is crucial to use antibiotics prudently and only when necessary, per the recommendations of a healthcare provider.
- Controlling underlying conditions: Candida glabrata infections are more prevalent in individuals with compromised immune systems or certain underlying medical conditions, such as diabetes or HIV/AIDS, that must be managed. Effective management of these conditions, including appropriate treatment and routine medical monitoring, can reduce the risk of infection.
- Probiotics: Some studies suggest that probiotics, which are beneficial bacteria, may aid in maintaining a healthy microbial balance within the body and reduce the risk of Candida overgrowth. However, additional research is required to determine their efficacy against Candida glabrata infections.
- Antifungal prophylaxis: Antifungal prophylaxis may be considered in high-risk situations, such as protracted neutropenia (low white blood cell count) in cancer patients or organ transplant recipients. This involves the administration of antifungal medications to prevent fungal infections. A healthcare professional should determine the need for antifungal prophylaxis based on patient-specific factors.
FAQ
What is Candida glabrata?
Candida glabrata is a type of yeast or fungus that can cause infections in humans. It is considered an opportunistic pathogen and is commonly associated with healthcare settings and individuals with weakened immune systems.
How common are Candida glabrata infections?
Candida glabrata infections have been on the rise in recent years. It is now recognized as one of the leading causes of Candida infections, especially in healthcare-associated settings and among individuals who have received broad-spectrum antibiotics or have compromised immune systems.
What are the symptoms of a Candida glabrata infection?
The symptoms of Candida glabrata infections can vary depending on the site of infection. Common manifestations include vaginal itching and discharge in vaginal infections, urinary frequency and discomfort in urinary tract infections, and fever, chills, and bloodstream infection in severe cases.
How is Candida glabrata diagnosed?
Candida glabrata infections can be diagnosed through various methods. These may include microscopic examination of clinical samples, culture and identification of the yeast, and, in some cases, molecular testing or antifungal susceptibility testing to determine the most effective treatment.
What factors increase the risk of developing Candida glabrata infections?
Several factors can increase the risk of developing Candida glabrata infections. These include recent use of broad-spectrum antibiotics, prolonged hospitalization or stay in healthcare facilities, compromised immune system (such as in HIV/AIDS or organ transplant patients), diabetes, and the presence of indwelling medical devices like catheters.
Can Candida glabrata infections be sexually transmitted?
Candida glabrata infections are typically not considered sexually transmitted. However, sexual activity can sometimes disrupt the balance of microorganisms in the genital area, increasing the risk of yeast overgrowth and potential infection.
Are there any specific treatments for Candida glabrata infections?
The treatment of Candida glabrata infections often involves antifungal medications. Fluconazole is commonly used as the first-line treatment, but in cases of resistance or severe infections, echinocandins or amphotericin B may be prescribed. Treatment should be tailored to the individual patient’s condition and guided by antimicrobial susceptibility testing.
Can Candida glabrata infections be prevented?
While complete prevention may not be possible, certain measures can help reduce the risk of Candida glabrata infections. These include practicing good hygiene, proper catheter care, judicious use of antibiotics, controlling underlying conditions, and considering antifungal prophylaxis in high-risk situations.
Are there any natural remedies or alternative treatments for Candida glabrata infections?
Natural remedies and alternative treatments for Candida glabrata infections have not been extensively studied or proven to be effective. It is generally recommended to rely on medically prescribed antifungal medications for the treatment of these infections.
What should I do if I have recurrent Candida glabrata infections?
If you have recurrent Candida glabrata infections, it is important to consult with a healthcare professional. They can evaluate your specific situation, assess for any underlying factors contributing to the recurrences, and determine the most appropriate treatment plan, which may involve longer courses of antifungal therapy or additional investigations to identify potential causes.
References
- Pfaller, M. A., & Diekema, D. J. (2007). Epidemiology of invasive candidiasis: a persistent public health problem. Clinical Microbiology Reviews, 20(1), 133-163.
- Silva, S., Negri, M., Henriques, M., Oliveira, R., Williams, D. W., & Azeredo, J. (2012). Candida glabrata, Candida parapsilosis and Candida tropicalis: biology, epidemiology, pathogenicity and antifungal resistance. FEMS Microbiology Reviews, 36(2), 288-305.
- Chakrabarti, A., Sood, P., & Rudramurthy, S. M. (2011). Epidemiology, pathogenesis, and management of Candida glabrata infections. Journal of Fungi, 1(3), 87-101.
- Asmundsdottir, L. R., Erlendsdottir, H., & Gottfredsson, M. (2011). Increasing incidence of candidemia: results from a 20-year nationwide study in Iceland. Journal of Clinical Microbiology, 49(3), 1165-1173.
- Pfaller, M. A., Diekema, D. J., Gibbs, D. L., Newell, V. A., Ellis, D., Tullio, V., … & Rodloff, A. (2010). Results from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997 to 2007: a 10.5-year analysis of susceptibilities of Candida species to fluconazole and voriconazole as determined by CLSI standardized disk diffusion. Journal of Clinical Microbiology, 48(4), 1366-1377.
- Chen, S. C., & Sorrell, T. C. (2007). Antifungal agents. Medical Journal of Australia, 187(7), 404-409.
- Shields, R. K., Nguyen, M. H., Press, E. G., Clancy, C. J., & Arias, C. A. (2015). A guide to the treatment of Candidal infections in patients with advanced HIV infection. HIV Therapy, 6(2), 149-161.
- Clinical and Laboratory Standards Institute (CLSI). (2020). Reference method for broth dilution antifungal susceptibility testing of yeasts (4th ed.). CLSI standard M27.
- Fidel Jr, P. L. (2006). History and update on host defense against vaginal candidiasis. American Journal of Reproductive Immunology, 57(1), 2-12.
- Kaur, R., Ma, B., & Cormack, B. P. (2007). A family of glycosylphosphatidylinositol-linked aspartyl proteases is required for virulence of Candida glabrata. Proceedings of the National Academy of Sciences, 104(18), 7628-7633.
- Fidel PL Jr, Vazquez JA, Sobel JD. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev. 1999 Jan;12(1):80-96. doi: 10.1128/CMR.12.1.80. PMID: 9880475; PMCID: PMC88907.
- Kumar K, Askari F, Sahu MS, Kaur R. Candida glabrata: A Lot More Than Meets the Eye. Microorganisms. 2019 Jan 30;7(2):39. doi: 10.3390/microorganisms7020039. PMID: 30704135; PMCID: PMC6407134.