What is Cancer Cell?
- Cancer cells are cells that escape the body’s natural growth regulation systems, dividing uncontrollably to form masses known as tumors or, in some cases, infiltrating the blood or lymphatic system with abnormal cells. Typically, cells follow a structured cycle involving growth, division, and self-destruction (or apoptosis) once they are no longer needed. However, cancer cells bypass these checkpoints, allowing them to reproduce continuously without the natural signals that would normally stop division.
- This unregulated growth leads to tissue masses, often referred to as tumors, when the cells are in solid tissues. When these cells enter the bloodstream or lymphatic system, they can circulate throughout the body, leading to metastasis, a process by which cancer cells spread to distant organs. Unlike normal cells, which only divide in response to specific growth signals, cancer cells can proliferate independently, making them exceptionally difficult to control.
- The distinguishing features of cancer cells include their ability to ignore growth-inhibiting signals and their tendency to invade surrounding tissues. Their evasion of programmed cell death allows them to persist far longer than normal cells, contributing to the spread and growth of cancerous tissue. This resistance to the body’s usual regulatory mechanisms is a key challenge in treating cancer effectively, and much research focuses on finding ways to target and inhibit these cells’ specific behaviors.
Definition of Cancer Cell
A cancer cell is an abnormal cell that divides uncontrollably, ignores natural growth regulation, and can invade surrounding tissues or spread to other parts of the body.
Characteristics of Cancer Cells
Characteristics of Cancer Cells
Cancer cells are fundamentally different from normal cells in ways that make them dangerous and difficult to treat. They have the ability to bypass many of the body’s natural control systems, allowing them to grow uncontrollably, evade the immune system, and spread throughout the body. Here’s a breakdown of the core characteristics that define cancer cells:
- Uncontrolled Growth and Division
- Normal Cells: They grow and divide in a controlled manner, responding to signals that regulate their proliferation.
- Cancer Cells: They ignore these regulatory signals. Cancer cells can divide rapidly without external instructions and lack contact inhibition, meaning they continue growing even when surrounded by other cells, leading to tumor formation.
- Immortality
- Normal Cells: These have a limited lifespan and can only divide a certain number of times before undergoing programmed cell death.
- Cancer Cells: They bypass this limit, often by activating telomerase, which prevents telomere shortening during division. This lets them replicate indefinitely.
- Evading Apoptosis (Programmed Cell Death)
- Normal Cells: They undergo apoptosis when they are damaged or no longer needed.
- Cancer Cells: They resist apoptosis, allowing damaged or mutated cells to survive and keep proliferating. This evasion is usually due to mutations in key genes, like TP53, which regulates the cell cycle and apoptosis.
- Altered Metabolism
- Normal Cells: Typically rely on oxidative phosphorylation for energy, using oxygen efficiently.
- Cancer Cells: Many cancer cells use glycolysis for energy, even in the presence of oxygen (the Warburg effect). This shift supports rapid cell growth and helps them thrive in low-oxygen environments.
- Genomic Instability
- Normal Cells: Their DNA is relatively stable, and any mutations are usually repaired.
- Cancer Cells: They often exhibit genetic instability, with mutations, chromosomal duplications, and deletions. This increases the likelihood of further mutations, fueling tumor growth and resistance to treatment.
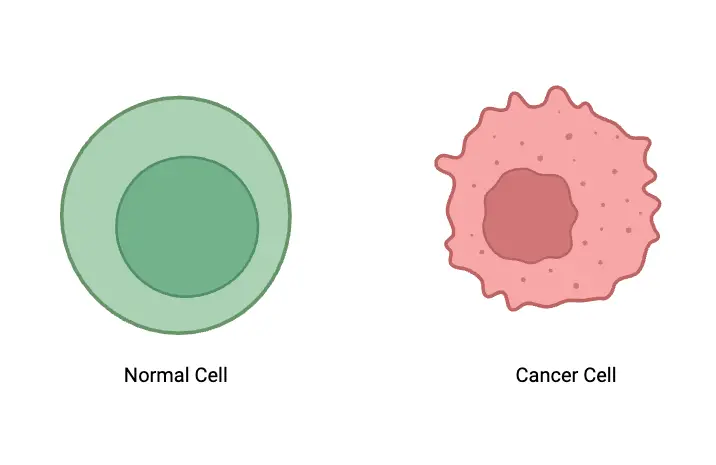
- Irregular Morphology
- Normal Cells: They have a uniform, smooth shape, and their nuclei are typically round with evenly distributed chromatin.
- Cancer Cells: These cells have irregular shapes, enlarged or misshapen nuclei, and coarse, clumped chromatin. They may even have multiple nucleoli.
- Angiogenesis (New Blood Vessel Formation)
- Normal Cells: Blood vessels form only when needed for growth or repair.
- Cancer Cells: They can induce angiogenesis, creating a new blood supply to provide oxygen and nutrients to support their rapid growth, especially when tumors exceed a certain size.
- Invasion and Metastasis
- Normal Cells: They stay in their designated areas within tissues and do not invade surrounding areas.
- Cancer Cells: These cells can invade nearby tissues and spread to distant organs through the bloodstream or lymphatic system, forming secondary tumors (metastasis).
Morphology of Cancer Cells
The morphology of cancer cells shows distinct deviations from normal cells, with changes in structure, organization, and function that support their uncontrolled growth and invasiveness. These alterations are observed across nuclear, cytoplasmic, and cellular membrane structures, contributing to the aggressive behavior of cancer cells.
- Nuclear Morphology
- Size and Shape: Cancer cell nuclei are often larger and irregularly shaped, contrasting with the smooth, spherical nuclei seen in healthy cells. This irregularity is often due to increased DNA content and faster cell division.
- Prominent Nucleoli: These cells feature multiple, enlarged nucleoli, reflecting an elevated rate of ribosomal RNA synthesis for increased protein production.
- Chromatin Structure: Chromatin in cancer cells appears coarse and unevenly distributed, forming aggregates, unlike the fine, evenly distributed chromatin in normal cells. This disorganization includes reduced heterochromatin and increased nuclear membrane pores.
- Ultrastructural Changes: Cancerous nuclei may show features like invaginations, segmentation, and inclusions, indicating genomic instability and higher malignancy potential.
- Cytoplasmic Changes
- Volume and Composition: The cytoplasm in cancer cells is reduced in volume and appears basophilic due to an accumulation of ribosomal and messenger RNA, supporting the rapid division of these cells.
- Organelle Alterations: Cancer cells exhibit a poorly developed Golgi apparatus and reduced mitochondrial volume as the tumor advances. The endoplasmic reticulum, both granular and agranular, appears fragmented and simplified, with reduced granulation.
- Cytoskeletal Modifications: The arrangement of microfilaments, intermediate filaments, and microtubules varies in cancer cells. These cytoskeletal alterations enhance cell motility, helping cancer cells invade surrounding tissues.
- Cell Membrane Characteristics
- Surface Receptors: Cancer cell membranes show modified surface receptors that alter signaling pathways and immune response, including the presence of abnormal antigens and molecules that may trigger immune reactions.
- Reduced Adhesion: Due to lower expression of adhesion molecules, such as E-cadherin, cancer cells have less attachment to each other and to the extracellular matrix, making it easier for them to spread.
- Enzyme Activity: The cell membrane is highly active in enzyme production, further enabling cancer cell growth and spread.
- Metabolic Changes
- Energy Metabolism: Cancer cells frequently exhibit the “Warburg effect,” relying on glycolysis for energy production even when oxygen is available. This abnormal energy pathway enables rapid energy generation, essential for their growth and proliferation.
- Metabolic Parasites: These cells behave like metabolic parasites, consuming high amounts of glucose and displaying abnormal glycolysis on mitochondrial membranes.
- Heterogeneity Among Cancer Cells
- Intra-tumor Variability: Morphological differences within a tumor, such as nucleus size and shape, can vary among clusters of cancer cells. This heterogeneity is linked to genomic instability and can influence the prognosis of the disease.
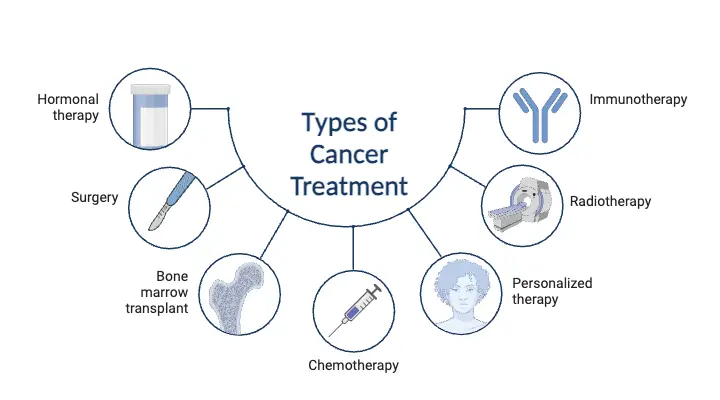
Types of Cancer Cells
Cancer cells are classified based on the type of tissue they originate from. These categories help define the characteristics and behavior of cancer, influencing treatment and prognosis. Below are the key types of cancer cells:
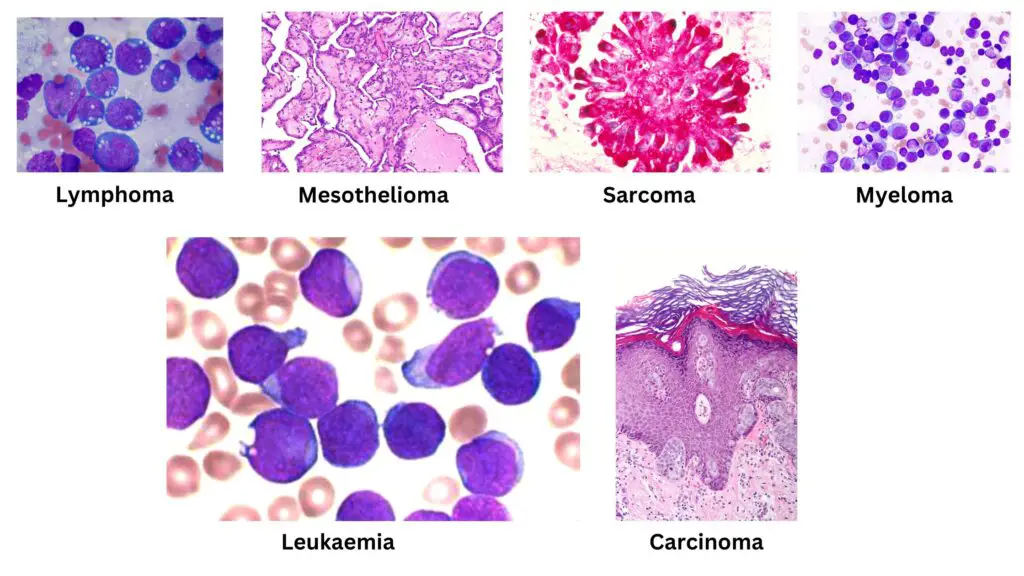
- Carcinomas
- Origin: Carcinomas start in the epithelial cells, which line the organs and body surfaces. They are the most common type, representing about 90% of all cancers.
- Subtypes:
- Adenocarcinoma: Arises from glandular cells that produce fluids, commonly affecting organs like the breast, prostate, and pancreas.
- Squamous Cell Carcinoma: Develops from squamous cells, which are flat cells found in the skin and lining of various organs, including the lungs and esophagus.
- Basal Cell Carcinoma: Originates from basal cells in the deeper layers of the skin and is often associated with sun exposure.
- Transitional Cell Carcinoma: Found in the transitional epithelium of the bladder and other parts of the urinary tract.
- Sarcomas
- Origin: Sarcomas develop from connective tissues like bone, cartilage, fat, and muscle. They are less common than carcinomas.
- Subtypes:
- Osteosarcoma: A type of bone cancer, often seen in teenagers and young adults.
- Chondrosarcoma: Cancer that arises from cartilage cells.
- Liposarcoma: A cancer of fat tissue, typically occurring in deep tissues.
- Leukemias
- Origin: Leukemias are cancers of the blood-forming tissues, particularly the bone marrow. They mainly affect white blood cells and do not form solid tumors.
- Subtypes:
- Acute Lymphoblastic Leukemia (ALL): Rapidly progressing leukemia that affects lymphoid cells.
- Acute Myeloid Leukemia (AML): Also fast-growing, involving myeloid cells.
- Chronic Lymphocytic Leukemia (CLL): A slower-growing leukemia, often affecting older adults.
- Lymphomas
- Origin: Lymphomas begin in the lymphatic tissues and primarily affect the immune system.
- Subtypes:
- Hodgkin Lymphoma: Characterized by the presence of Reed-Sternberg cells, a distinct feature in the cancer cells.
- Non-Hodgkin Lymphoma: A diverse group of blood cancers that includes many different subtypes, each with varying growth rates and behavior.
- Central Nervous System (CNS) Cancers
- Origin: CNS cancers start in the brain or spinal cord tissues. They are complex and can have a wide variety of types depending on their cell origin.
- Subtypes:
- Gliomas: Arise from glial cells that support and protect neurons.
- Meningiomas: Develop from the meninges, the protective layers surrounding the brain and spinal cord.
- Mesothelioma
- Origin: Mesothelioma originates in the mesothelium, a thin layer of tissue that covers many internal organs. It is most commonly linked to asbestos exposure and primarily affects the lungs, heart, or abdomen.
Cancer Cells Development Process
Cancer cell development follows a complex sequence that transforms normal cells into malignant ones, primarily driven by genetic mutations and environmental influences. This process consists of several stages: initiation, promotion, progression, and metastasis, each contributing to the aggressive characteristics of cancer cells.
- Initiation
- Genetic Mutations: The initial stage, or initiation, begins when a cell sustains irreversible DNA changes due to exposure to carcinogens like chemicals, UV radiation, or viruses, or through natural errors in DNA replication.
- Oncogenes and Tumor Suppressors: These mutations typically involve the activation of oncogenes, which push cells toward unregulated growth, or the deactivation of tumor suppressor genes, removing their role in controlling cell division.
- Clonal Expansion: Once a cell is initiated, it begins to proliferate uncontrollably, producing a clone of genetically altered cells that form the groundwork for a tumor.
- Promotion
- Non-Genetic Growth Factors: Promotion is driven by factors that increase the growth of initiated cells without altering DNA. This stage may involve substances or environmental conditions that enhance cell division.
- Hyperplasia and Dysplasia: As promoted cells divide rapidly, they experience hyperplasia, an increase in cell number. These cells may also undergo dysplasia, taking on abnormal shapes and organization, gradually departing from their original function.
- Reversible Changes: Since promotion affects gene expression rather than DNA structure, its effects can sometimes be reversed if the promoting factors are removed.
- Progression
- Malignant Transformation: At this stage, the cells undergo further genetic changes, acquiring characteristics that enhance their malignancy, like rapid growth, ability to invade, and resistance to apoptosis.
- Chromosomal Instability: Cancer cells in progression often display karyotypic instability, with irregular chromosome numbers (aneuploidy), which contributes to their aggressive behavior.
- Invasiveness: Progressing cancer cells produce enzymes that degrade surrounding tissues, aiding their spread and establishing new footholds in adjacent areas.
- Angiogenesis
- Formation of Blood Supply: Cancer cells stimulate angiogenesis, attracting new blood vessels to supply the tumor with nutrients and oxygen. This step is crucial for tumor growth beyond a minimal size and enables further spread.
- Metastasis
- Tissue Invasion: In the metastatic phase, cancer cells invade nearby tissues, breaking past barriers like the basal lamina.
- Circulation and Colonization: Entering the bloodstream or lymphatic system, cancer cells migrate to distant organs, where they establish secondary tumors. This stage complicates treatment and worsens prognosis due to the widespread nature of the disease.
Types of Cell Death in Cancer Cells
Cancer cells can undergo various forms of cell death. Each type affects tumor progression differently, and understanding them can offer valuable insights into cancer treatment strategies. Here’s a breakdown of the major types of cell death observed in cancer cells:
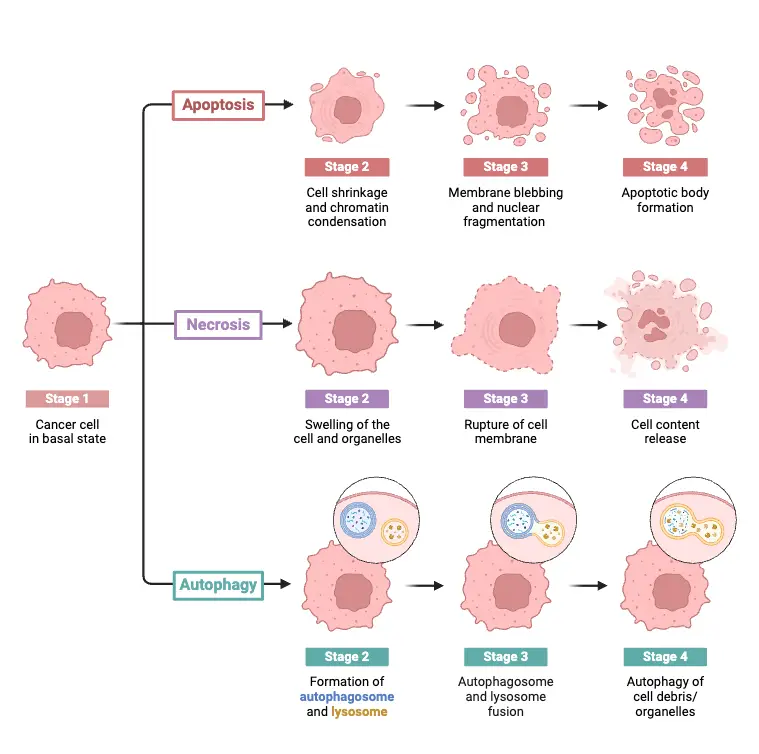
- Apoptosis
Apoptosis is the regulated process where cells self-destruct to prevent damage from spreading. It can be triggered through two pathways:- Intrinsic Pathway: Internal stress signals like DNA damage or oxidative stress cause mitochondrial changes, leading to caspase activation.
- Extrinsic Pathway: External signals from death ligands bind to receptors on the cell surface, setting off caspase activation as well.
In cancer, apoptosis is often blocked by overexpression of anti-apoptotic proteins like BCL-2, or by losing pro-apoptotic factors like BAX, allowing cancer cells to survive and accumulate genetic mutations.
- Autophagy
Autophagy is a cell’s survival mechanism where it breaks down and recycles its own components. Under stress, such as nutrient deprivation, cancer cells may activate autophagy to stay alive.- Pro-survival: Cancer cells use autophagy to endure tough conditions, like lack of oxygen or nutrients.
- Cell Death: When autophagy becomes excessive, it can lead to a form of cell death distinct from apoptosis, referred to as autophagic or type II cell death.
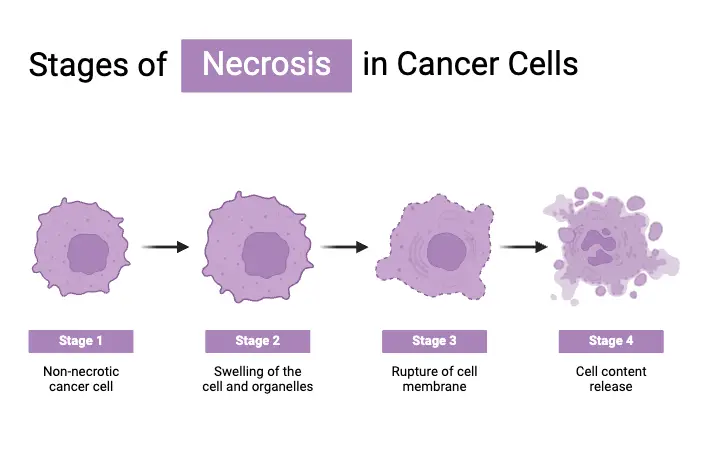
- Necrosis
Necrosis is an uncontrolled form of cell death typically caused by severe injury, lack of blood flow, or oxygen deprivation. It results in cell swelling, membrane rupture, and inflammation. In tumors, necrosis often occurs due to rapid growth that outpaces the blood supply, leaving parts of the tumor deprived of nutrients. - Necroptosis
Necroptosis is a programmed form of necrosis. When apoptosis is blocked, necroptosis kicks in. It’s regulated by proteins like RIPK1 and RIPK3 and involves swelling and membrane rupture, similar to necrosis. However, it’s distinct because it’s a controlled process that also activates inflammation, making it a potential target in cancers that avoid apoptosis. - Pyroptosis
Pyroptosis is an inflammatory form of programmed cell death. It’s driven by caspase-1 and results in the release of pro-inflammatory cytokines, which can trigger immune responses. While typically seen in response to infections, pyroptosis has been linked to cancer contexts, particularly where inflammation plays a role in tumor progression. - Ferroptosis
Ferroptosis is an iron-dependent form of cell death characterized by lipid peroxidation and failure of antioxidant defenses. It’s gaining attention as a potential target for cancer therapy, especially in tumors resistant to traditional treatments. - Parthanatos
Parthanatos is associated with the overactivation of poly(ADP-ribose) polymerase (PARP). This overactivation leads to severe DNA damage and energy depletion, driving the cell toward death. Parthanatos is typically observed under conditions of extreme stress. - Entosis
Entosis is a unique form of cell death where one cell engulfs another. This “cell-in-cell” phenomenon can occur during nutrient deprivation, and it’s believed to influence tumor growth and metastasis by enabling cells to survive in adverse conditions.
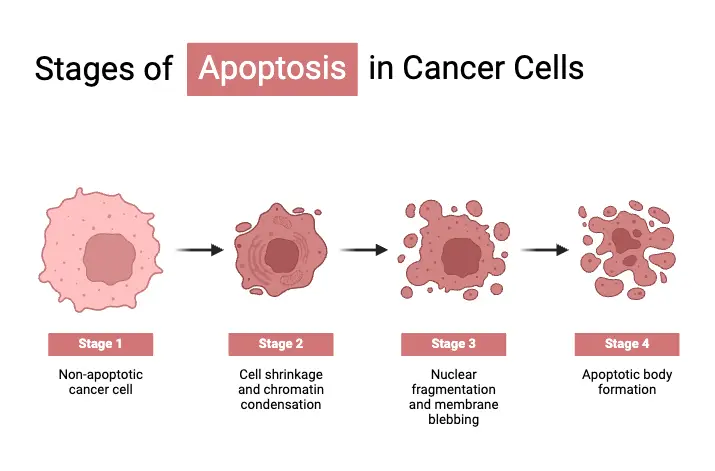
Stages of Apoptosis in Cancer Cells
Apoptosis is the body’s natural way of eliminating damaged or unwanted cells. It’s a tightly regulated process, but cancer cells often find ways to bypass it, which contributes to their uncontrolled growth. Here’s a detailed look at how apoptosis progresses and how cancer cells disrupt these stages to survive longer than they should.
- Initiation Phase
Apoptosis can be triggered in two major ways:- Extrinsic Pathway: This pathway starts when external signals, like ligands, bind to death receptors on the cell surface (e.g., TNF receptors). This kick-starts a cascade that activates initiator caspases, including caspase-8.
- Intrinsic Pathway: Internal signals, often from DNA damage or stress, activate this pathway. Pro-apoptotic proteins, such as Bax and Bak, initiate mitochondrial outer membrane permeabilization (MOMP), releasing cytochrome c. This sets off a chain reaction leading to caspase activation.
- Execution Phase
Once apoptosis is triggered, the execution phase takes over. Here, the cell begins to break down:- Caspase Activation: Executioner caspases (mainly caspase-3, -6, and -7) dismantle key cell structures, leading to the hallmark signs of apoptosis.
- Cell Shrinkage: The cell reduces in size, and its cytoplasmic volume decreases.
- Nuclear Fragmentation: The cell’s nucleus condenses and ultimately fragments.
- Apoptotic Bodies: The cell breaks apart into smaller vesicles known as apoptotic bodies. These are quickly identified and engulfed by nearby phagocytes, like macrophages, to prevent inflammation.
- Phagocytosis (Clearance Phase)
Once the cell has fragmented, the apoptotic bodies are removed through phagocytosis. This ensures that there’s no unnecessary release of harmful cellular contents, preventing tissue damage and inflammation.- Engulfment by Phagocytes: Macrophages or nearby epithelial cells engulf the apoptotic bodies, clearing the debris without causing harm.
- Evasion of Apoptosis in Cancer Cells
Cancer cells often develop strategies to escape apoptosis, allowing them to survive longer and accumulate mutations:- Loss of p53 Function: p53 is a tumor suppressor protein that plays a major role in triggering apoptosis when DNA is damaged. Mutations in the TP53 gene, which codes for p53, are common in cancers, preventing the cell from undergoing normal self-destruction.
- Upregulation of Anti-apoptotic Proteins: Cancer cells often overproduce anti-apoptotic proteins from the BCL-2 family, such as Bcl-2, which prevents pro-apoptotic signals from being effective.
- Inhibition of Caspases: Some cancer cells express inhibitors of apoptosis proteins (IAPs) that block caspase activity, preventing the execution phase of apoptosis from happening.
Differences Between Cancer Cells and Normal Cells – Cancer Cells vs. Normal Cells
Cancer cells differ from normal cells in several crucial ways, impacting their behavior and how they interact with the body. These differences help define how cancer develops, grows, and spreads. Here are the key distinctions between cancer cells and normal cells:
- Growth and Division
- Normal Cells: Normal cells grow and divide in a controlled manner. They respond to signals that indicate when to stop dividing. Once they reach their full size, they typically stop growing and maintain proper function.
- Cancer Cells: Cancer cells ignore these signals and continue to divide uncontrollably. They bypass the natural growth control mechanisms, even when unnecessary, leading to the formation of tumors.
- Lifespan and Cell Death
- Normal Cells: These cells have a defined lifespan. When they are damaged or no longer needed, they undergo programmed cell death, known as apoptosis.
- Cancer Cells: Cancer cells evade apoptosis. This allows them to survive longer than normal cells, even under abnormal conditions, and contributes to unchecked growth and metastasis.
- Cell Structure and Appearance
- Normal Cells: Normal cells generally have a smooth, uniform appearance. Their nuclei are typically round, with evenly distributed chromatin.
- Cancer Cells: Cancer cells often exhibit irregular shapes. Their nuclei may be enlarged or misshapen, with chromatin that appears clumped or coarse. These cells may also have multiple nucleoli.
- Communication and Adhesion
- Normal Cells: Normal cells communicate with each other through signaling pathways. These signals regulate growth and maintain tissue organization. Cells adhere to one another, preventing uncontrolled movement.
- Cancer Cells: Cancer cells lose the ability to communicate properly with neighboring cells. They do not adhere as tightly to each other, allowing them to migrate and invade other tissues, leading to metastasis.
- Metastasis
- Normal Cells: Normal cells remain in their designated location and do not invade surrounding tissues.
- Cancer Cells: Many cancer cells detach from the primary tumor, invade nearby tissues, and spread through the bloodstream or lymphatic system to distant organs. This spread is called metastasis.
- Energy Production
- Normal Cells: Normal cells primarily rely on oxidative phosphorylation for energy production, which is more efficient.
- Cancer Cells: Cancer cells often rely on glycolysis for energy, even in the presence of oxygen. This process is less efficient but supports rapid cell growth.
- Blood Supply and Nutrient Utilization
- Normal Cells: Normal cells attract blood vessels when necessary, such as during growth or repair, ensuring they receive sufficient nutrients and oxygen.
- Cancer Cells: Cancer cells can stimulate angiogenesis (formation of new blood vessels) to create a constant blood supply, even when not needed, which supports their accelerated growth.
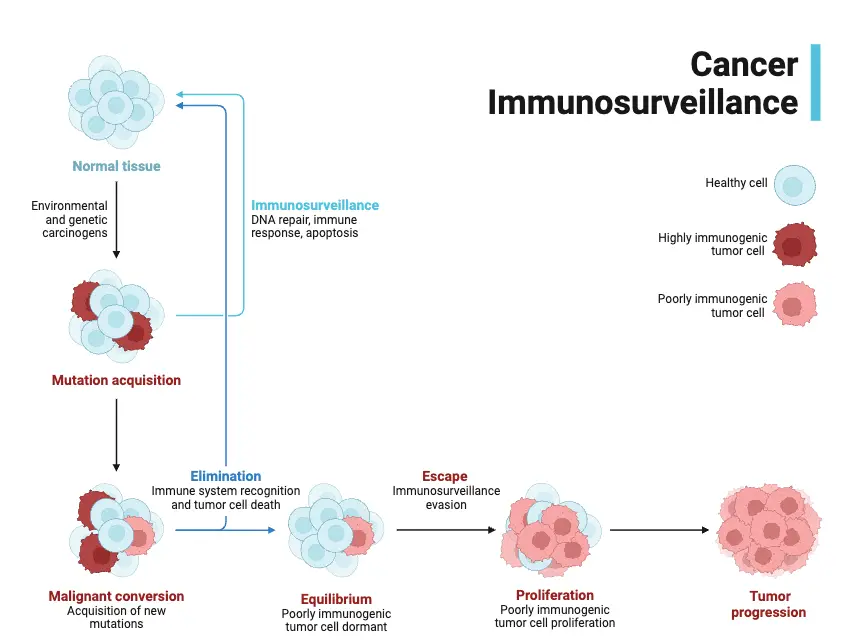
- Immune System Evasion
- Normal Cells: Damaged or abnormal normal cells are recognized and eliminated by the immune system.
- Cancer Cells: Cancer cells can evade the immune system by producing signals that suppress immune responses or altering their surface proteins to avoid detection.
- Cooper GM. The Cell: A Molecular Approach. 2nd edition. Sunderland (MA): Sinauer Associates; 2000. The Development and Causes of Cancer. Available from: https://www.ncbi.nlm.nih.gov/books/NBK9963/
- American Cancer Society. (2023). Cancer facts & figures 2023. American Cancer Society.Baker, S. G., & Karp, J. E. (2022). The biology of cancer: A comprehensive overview. Journal of Cancer Research, 78(4), 123-145. https://doi.org/10.1007/s12345-022-01234-5
- Hanahan, D., & Weinberg, R. A. (2011). Hallmarks of cancer: The next generation. Cell, 144(5), 646-674. https://doi.org/10.1016/j.cell.2011.02.013
- Kumar, V., Abbas, A. K., Aster, J. C., & Fausto, N. (2018). Pathologic basis of disease (10th ed.). Elsevier.National Cancer Institute. (2023). Types of cancer. National Institutes of Health. https://www.cancer.gov/about-cancer/understanding/typesR
- osenberg, S. A., & Yang, J. C. (2020). The role of the immune system in cancer development and therapy: A review of recent advances. Nature Reviews Cancer, 20(9), 567-579. https://doi.org/10.1038/s41571-020-0378-x
- Seymour, L., & Ghosh, S. (2019). Understanding the mechanisms of cancer cell proliferation and survival: Implications for therapy. Cancer Biology & Therapy, 20(6), 764-775. https://doi.org/10.1080/15384047.2019.1577112
- https://en.wikipedia.org/wiki/Cancer_cell
- https://microbenotes.com/cancer-cells/
- https://www.cancer.gov/about-cancer/understanding
- https://www.verywellhealth.com/cancer-cells-vs-normal-cells-2248794
- https://karger.com/acy/article/64/6/511/9923/Nuclear-Morphology-and-the-Biology-of-Cancer-Cells
- https://karger.com/acy/article-pdf/64/6/511/3897849/000508780.pdf
- https://www.cancerresearchuk.org/about-cancer/what-is-cancer/how-cancer-starts/cancer-cells
- https://www.verywellhealth.com/what-are-cancer-cells-2248795
- https://www.baptisthealth.com/blog/cancer-care/what-s-the-difference-between-cancer-cells-normal-cells
- https://www.bioted.es/protocolos/MORPHOLOGY-CANCER-CELLS-ENG.pdf