Antibiotic resistance or Drug resistance to bacteria is a modern enemy of the new generation. Before we know about antibiotic resistance, we must first know what bacteria are?
Bacteria is a type of germs, which is found inside or outside of human or animal bodies. Most of the bacteria are harmless, and some of them can even be helpful to humans, but some can cause disease or infection such as strep throat and urinary tract infections.
Example: A group of Streptococcus bacteria cause strep throat infection.
Now, we need to know what is antibiotics?
Antibiotic refers to those powerful drugs which are used for treatment for the prevention of infection which is caused by bacteria on animal plants for the human body.
Example: Amoxicillin is an antibiotic, which is used for treatments of many different types of bacterial infections such as tonsillitis, bronchitis, pneumonia, and infections of the ear, nose, throat, skin, or urinary tract.
Remember bacteria and other microorganisms are constantly searching for new ways to avoid the effects of the antibiotics, which are design to kill them.
What is Antibiotic Resistance or Drug resistance?
- Antibiotic resistance or Drug resistance define as when a microorganism or fungi develop a resistant property against an antibiotic or drug which is design to kill them, Means the antibiotic is no longer to act against this bacterial infection.
- Example of Antibiotic resistance is, penicillin-resistant Enterococcus, methicillin-resistant Staphylococcus aureus (MRSA), multidrug-resistant Mycobacterium tuberculosis (MDR-TB
- Antibiotic resistance can be occurred by misuse and overuse of antibiotics.
- An important reason behind the development of drug resistance strain is that many antibiotics are bacteriostatic rather than bactericidal.
- If once a bacteria or microorganism develop a resistant property against an antibiotic or drug then it will be difficult to inhibit or kill that particular bacteria, which can cause life-threatening diseases.
What causes Antibiotic Resistance?
A bacteria or microorganism acquire the drug-resistant or Antibiotic resistance property by two mechanism,
- Nongenetic Resistance.
- Genetic Resistance.
1. Nongenetic resistance
Noangenetic Drug Resistance occurs by two different way;
- The first type of nongenetic antibacterial resistance develops when microorganisms for example causative agents of tuberculosis persist in the tissues and get out of reach of antimicrobial agents. If this microorganism started to multiply and release their progeny, the progeny are still susceptible to the antibiotic. This type of resistance is called evasion.
- The second type of antibacterial resistance develops when bacteria temporarily converted into L forms which lack the cell walls, and they can resist those antibiotics that act on cell walls.
2. Genetic resistance
- Genetic resistance to antimicrobial drugs can be occurred by natural selection (mutation).
Antibiotic Resistance Mechanism
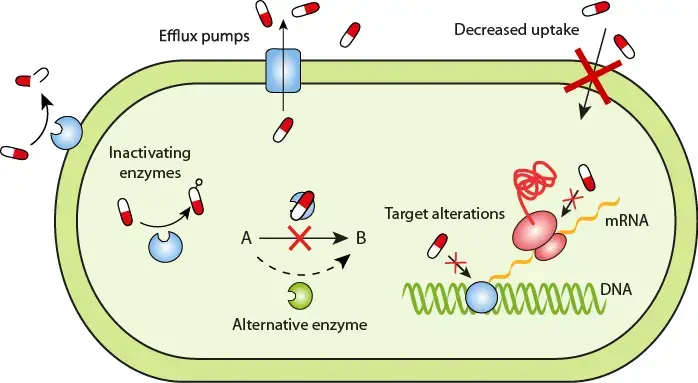
There are present five Mechanism of antibiotic resistance;
- Antibiotic resistance can be occurred by altering the target, this mechanism usually affect the ribosome. For Example, Resistance to erythromycin, rifamycin, and antimetabolites has developed by this mechanism.
- Bacteria can show antibiotic resistance by altering the membrane permeability. The alteration of membrane permeability can occur when new genetic information changes the nature of proteins in the membrane and as a result, it changes a membrane transport system or pores (Efflux pump) in membrane, so an antimicrobial agent can no longer cross the membrane. For Example, tetracyclines, quinolones, and some aminoglycosides resistant has occurred by this mechanism
- Bacteria also can do antibiotic resistance by developing an enzyme that can inactivate or destroy the antibiotic. For Example, Enzyme beta-lactam exist in various bacteria which has capability to destroy or inactivate beta-lactam ring in penicillins and some cephalosporins.
- Antibiotic resistance can occur by altering enzymes. For Example, sulfonamide resistant bacteria.
- Antibiotic resistance can be occurred by altering the Metabolic Pathway. For Example, sulfonamide-resistant bacteria follow these mechanisms. These bacteria have acquired the ability to use ready-made folic acid from their environment and no longer need to make it from PABA.
Newly Discovered Antibiotic resistance Gene
- Aminoglycoside antibiotics are important for tratment of several types infections with multi-resistant bacteria. A completely new resistance gene, they called it gar, because it provide resistance against garosamine group containing aminoglycoside antibiotics.This is the case for the newest aminoglycoside drug, plazomycin, developed to circumvent most existing aminoglycoside resistance mechanisms. This was recently discovered by scientists in Gothenburg, Sweden.
Journal Reference: https://doi.org/10.1186/s40168-020-00814-z
- A new drug resistance gene, rfaF was discovered in Helicobacter pylori, which can changes the permeability of cell membrane to confer cross-resistance to AMO, TET, CLA, and CHL and is involved in clinical strain drug resistance. It can be used as a drug target. This research was conducted by a group of chines sientist of Lin J, Zhang X, Wen Y, Chen H, She F
Journal Reference: https://doi.org/10.2147/IDR.S231152
Important Viva Questions Related to Antibiotic resistance
What Is Multidrug Resistance (MDR)?
Multidrug resistance (MDR) also known as Intrinsic resistance. It defines as when a species of microorganism exhibits antibacterial resistance to at least one antimicrobial drug in three or more antimicrobial categories.
Example: Mycobacterium tuberculosis to rifampicin and isoniazid or Candida spp. to fluconazole.
What Is Extensive drug resistance (XDR)?
Extensive drug resistance defines as when a microorganism shows antibacterial resistance to at least one or two most effective antimicrobial drugs.
Example: XDR-TB resistance against fluoroquinolone.
What Is MRSA?
The full form of MRSA is Methicillin-resistant Staphylococcus aureus, it is a type of bacteria that resistant to several antibiotics. It is a type of staph infection that is difficult to treat because of resistance to some antibiotics.
What is NDM1?
NDM1 stands for New Delhi metallo-beta-lactamase 1, it is an enzyme which show bacterial resistance property against a broad range of beta-lactam antibiotics.
Reference
- https://www.drugs.com/amoxicillin.html
- https://www.healthline.com/health/strep-throat
- https://www.britannica.com/science/antibiotic-resistance
- http://www.reading.ac.uk/news-archive/press-releases/pr597734.html
- https://futurism.com/neoscope/scientists-have-found-a-way-to-reverse-antibiotic-resistance
- https://www.cdc.gov/antibiotic-use/community/about/antibiotic-resistance-faqs.html
- https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance
- https://www.cdc.gov/mrsa/index.html