What is Amniocentesis? (Amniotic Fluid Test)
- Amniocentesis, also known as the amniotic fluid test, is a medical procedure used for prenatal genetic testing and diagnosis of various conditions. It involves obtaining a sample of amniotic fluid from a pregnant woman for analysis.
- During amniocentesis, a long sterile needle is carefully inserted through the abdominal wall and into the amniotic sac, which surrounds the developing fetus. The needle punctures the amnion, the membrane that holds the amniotic fluid. The amniotic fluid, which fills the amniotic sac, contains fetal cells that can be used for genetic testing.
- The primary purpose of amniocentesis is the prenatal diagnosis of genetic conditions. It is considered the gold-standard procedure for diagnosing genetic disorders after 15 weeks of gestation. The collected amniotic fluid is analyzed using techniques such as karyotyping and DNA analysis to detect genetic abnormalities.
- Amniocentesis is typically performed during the second trimester, specifically between the 15th and 20th week of gestation. It is commonly recommended for women who are at an increased risk of genetic or chromosomal problems. However, the American College of Obstetricians and Gynecologists suggests that all women should be offered prenatal assessment for chromosomal abnormalities, regardless of age or risk factors.
- While amniocentesis is generally safe, it is an invasive procedure and carries a small risk of pregnancy loss. Physicians evaluate the relative contraindications before performing amniocentesis, but there are no absolute contraindications identified for the procedure.
- The history of using needle insertion into the uterus for extracting amniotic fluid dates back to the late 1800s when physicians used a similar technique to manage hydramnios, an excess of amniotic fluid.
- Amniocentesis plays a crucial role in prenatal genetic testing, providing valuable information about the health and development of the fetus. It allows for early detection, diagnosis, and informed decision-making for expectant parents and healthcare providers.
Sample for Amniotic fluid Examination (Amniocentesis)
- Amniocentesis is a medical procedure used to collect a sample of amniotic fluid for examination. The collected amniotic fluid provides valuable information about the health and development of the fetus.
- During amniocentesis, a thin needle is inserted through the abdominal wall of the pregnant woman and into the amniotic sac. The amniotic sac surrounds the developing fetus and contains the amniotic fluid. This fluid serves as a protective cushion for the fetus and contains important substances that can be analyzed for diagnostic purposes.
- Once the amniotic fluid is collected, proper handling and storage are essential. It is recommended to refrigerate the amniotic fluid to maintain its integrity and prevent any potential degradation of cellular components. Additionally, it is important to protect the amniotic fluid from light when estimating bilirubin levels, as exposure to light can alter the accuracy of the results.
- Amniocentesis is typically performed during specific weeks of gestation, namely the 14th, 16th, and 18th weeks. This timing allows for optimal collection of amniotic fluid and sufficient fetal development for accurate diagnostic testing.
- While amniocentesis is a widely used procedure, it is worth noting that chorionic villus sampling (CVS) is an alternative method for obtaining fetal genetic material. CVS involves collecting a sample of chorionic villi, which are tiny projections on the placenta. CVS is considered advantageous over amniotic fluid for karyotyping and genetic analysis due to its early timing (around 10-13 weeks of gestation) and the direct sampling of fetal genetic material. However, the choice between amniocentesis and CVS depends on various factors, including gestational age, specific testing requirements, and the risks associated with each procedure.
- Both amniocentesis and CVS serve as important diagnostic tools in prenatal care, allowing for the detection of genetic abnormalities and chromosomal disorders. The collected samples are sent to a laboratory for analysis, including karyotyping and genetic testing, which provide crucial information for expectant parents and healthcare providers in making informed decisions about the health and well-being of the fetus.
The purpose of the test
Amniocentesis, the examination of amniotic fluid, serves various purposes in prenatal diagnosis and assessment. The test provides valuable information about the fetus, allowing healthcare providers to make informed decisions regarding the health and well-being of both the mother and the unborn child.
The indications or purposes of amniotic fluid examination (amniocentesis) include:
- Diagnosing Genetic Disorders: Amniocentesis is commonly used for cytogenetic analysis, which involves examining the chromosomes of the fetus. This helps in diagnosing genetic disorders and identifying chromosomal abnormalities.
- Diagnosing Inherited Metabolic Disorders: Amniocentesis can aid in diagnosing inherited metabolic disorders, such as cystic fibrosis, by analyzing the presence of specific genetic markers or enzymes in the amniotic fluid.
- Detecting Neural Tube Defects: Amniocentesis is used to diagnose neural tube defects, including conditions like myelomeningocele, anencephaly, and spina bifida, which affect the development of the spinal cord or brain.
- Assessing Rh Sensitization: In cases of Rh sensitization, where the mother’s immune system may react against the fetus’ blood cells, amniocentesis can be performed to measure bilirubin levels in the amniotic fluid, providing information about the severity of erythroblastosis fetalis.
- Diagnosing Chorioamnionitis: Amniocentesis may be used to diagnose chorioamnionitis, an infection of the placenta and the amniotic sac, by analyzing the presence of bacteria or other indicators of infection in the amniotic fluid.
- Assessing Fetal Lung Maturity: Amniotic fluid can be sampled after 32 weeks of gestation to assess fetal lung maturity. The lecithin/sphingomyelin (L/S) ratio, as well as the measurement of phospholipids, can help determine the maturity of the fetal lungs.
- Assessing Postmature Pregnancy: Amniocentesis may be used to assess pregnancies that have extended beyond the estimated due date (postmature pregnancies), providing information about the well-being of the fetus.
- Detecting Intrauterine Growth Restriction: Amniocentesis can aid in identifying intrauterine growth restriction, a condition where the fetus does not grow at the expected rate, potentially indicating underlying health issues.
- Diagnosing Congenital Infections: Amniocentesis can help diagnose certain congenital infections, such as toxoplasmosis and cytomegalovirus (CMV), by analyzing the presence of specific markers or performing cultures for bacterial infections.
- Assisting with Elective Abortion: In cases where a fetus is found to have severe abnormalities or genetic disorders, amniocentesis can provide information to support the decision-making process for elective abortion.
- Diagnosing Respiratory Distress Syndrome (RDS): Amniocentesis may be used to diagnose respiratory distress syndrome, a condition that affects premature newborns. Analysis of the amniotic fluid can provide insights into fetal lung maturity and the risk of developing RDS.
It is important to note that the decision to undergo amniocentesis is based on individual circumstances, medical history, and consultation with healthcare professionals. The procedure carries certain risks, including a small risk of pregnancy loss, which should be carefully considered and discussed with a healthcare provider.
What is amniotic fluid?
- Amniotic fluid is the clear, straw-colored fluid that fills the amniotic sac and surrounds the developing fetus during pregnancy. It plays a crucial role in the growth and protection of the fetus throughout gestation.
- The amniotic fluid is composed of various components derived from different sources. A portion of the amniotic fluid is produced by the fetal respiratory system, which includes the lungs, as the fetus practices breathing movements. This fluid is released into the amniotic sac through the fetal airways. Additionally, the fetal kidneys contribute to the production of amniotic fluid through the excretion of urine. The amniotic membrane, which surrounds the fetus, also secretes small amounts of fluid. Furthermore, the umbilical cord, which connects the fetus to the placenta, may contribute to the fluid by releasing small amounts of fetal blood.
- The volume of amniotic fluid changes throughout pregnancy. At term, which refers to the end of the pregnancy period, the average volume of amniotic fluid is approximately 500 to 1100 milliliters. This volume is considered normal and provides a sufficient cushioning and protective environment for the fetus.
- Amniotic fluid serves several essential functions during pregnancy. It acts as a shock absorber, protecting the developing fetus from external pressure and impact. It also helps maintain a stable temperature for the fetus and allows for unrestricted movement, promoting proper musculoskeletal development. Furthermore, amniotic fluid enables the exchange of nutrients, oxygen, and waste products between the fetus and the mother’s bloodstream.
- The level and composition of amniotic fluid can be evaluated through medical procedures such as amniocentesis or ultrasound examinations. These assessments help monitor the well-being of the fetus and can provide valuable information about fetal development, lung maturity, and the presence of certain abnormalities.
- Overall, amniotic fluid plays a vital role in supporting the growth and development of the fetus, providing a protective and nurturing environment throughout pregnancy.
Pathophysiology of Amniotic fluid
Amniotic fluid plays a crucial role in maintaining a healthy intrauterine environment for the developing fetus. The pathophysiology of amniotic fluid involves its formation, regulation, and potential imbalances that can occur during pregnancy.
Amniotic fluid is contained within the amnion, a membranous sac that surrounds and protects the fetus. The formation of amniotic fluid is a dynamic process involving contributions from various sources:
- Fetal Respiratory Tract: The fetal respiratory system, including the lungs, contributes to the production of amniotic fluid. As the fetus practices breathing movements, small amounts of fluid are released into the amniotic sac through the fetal airways.
- Fetal Urine: The fetal kidneys play a significant role in the production of amniotic fluid. The excretion of urine by the fetus adds to the volume of fluid in the amniotic sac.
- Amniotic Membrane: The amniotic membrane itself secretes a certain amount of fluid, contributing to the overall volume of amniotic fluid.
- Umbilical Cord: The umbilical cord, which connects the fetus to the placenta, may also release small amounts of fluid into the amniotic sac.
Throughout pregnancy, the volume of amniotic fluid gradually increases, reaching its peak during the third trimester, at approximately one liter (1 L). As the due date approaches, the volume of amniotic fluid gradually decreases.
During the first trimester, around 30 mL of amniotic fluid is derived from the maternal circulation. Its composition is similar to the mother’s plasma, with the addition of fetal cells. These fetal cells present in the amniotic fluid can provide the basis for cytogenetic analysis, which involves examining the chromosomes for genetic abnormalities.
After the first trimester, the major contributor to the amniotic fluid volume is fetal urine. As the fetus swallows amniotic fluid, it helps regulate the balance between fluid production and absorption.
Imbalances in amniotic fluid volume can occur and have clinical implications:
- Hydramnios (Polyhydramnios): Hydramnios refers to an excessive accumulation of amniotic fluid. It can occur when there is a failure in swallowing amniotic fluid by the fetus. Hydramnios is often associated with conditions such as neural tube defects and can lead to fetal distress.
- Oligohydramnios: Oligohydramnios is characterized by a decreased volume of amniotic fluid. It can be caused by increased swallowing of fluid by the fetus, urinary tract abnormalities in the fetus, or membrane leakage. Oligohydramnios may indicate a compromised intrauterine environment and can be associated with fetal growth restrictions and other complications.
Monitoring the volume and composition of amniotic fluid is important in assessing the well-being of the fetus during pregnancy. Ultrasound examinations and other diagnostic tests can help evaluate amniotic fluid levels and detect any abnormalities that may require further evaluation or management.
Composition of Amniotic fluid
Amniotic fluid, the fluid present in the amniotic sac surrounding the fetus, has a specific composition that undergoes changes throughout pregnancy. The composition of amniotic fluid is influenced by various factors, including the contribution from different sources and the physiological processes occurring within the fetus.
The composition of amniotic fluid changes significantly with the onset of fetal urine formation. As the fetus develops and its renal system matures, the concentrations of certain substances in the amniotic fluid are altered. Here are some key aspects of the composition of amniotic fluid:
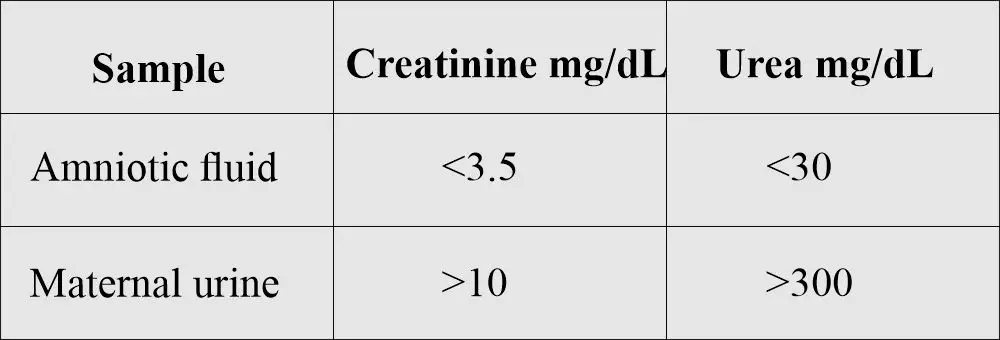
- Substances Affected by Urine Formation: When fetal urine production begins, the concentrations of certain substances in the amniotic fluid are influenced. Creatinine, urea, and uric acid concentrations tend to increase, while glucose and protein concentrations decrease. The presence of these substances reflects the metabolic activity and waste elimination processes of the developing fetus.
- Comparison to Maternal Urine: The concentration of urea and creatinine in the amniotic fluid is generally lower than in maternal urine. This difference indicates that the fetal kidneys are still developing and have limited filtration and excretory capabilities compared to the maternal kidneys.
- Sources of Amniotic Fluid: Amniotic fluid is derived from several sources within the developing fetus. These sources include the fetal respiratory system, amniotic membrane, urine produced by the fetus, and contributions from the umbilical cord. Each of these sources contributes to the overall volume and composition of the amniotic fluid.
- Protective Functions: Amniotic fluid plays a crucial role in the development and protection of the fetus. It surrounds and cushions the fetus, providing a protective barrier against external forces and mechanical shocks. The presence of amniotic fluid allows the fetus to move freely within the amniotic sac, which helps prevent compression of the umbilical cord and ensures adequate blood flow and oxygen supply to the developing fetus.
- Temperature Regulation: Amniotic fluid also helps regulate the temperature of the fetus during gestation. The fluid acts as an insulating medium, helping to maintain a stable and optimal temperature environment for the developing fetus.
The composition of amniotic fluid is complex and dynamic, influenced by various factors related to fetal development and physiological processes. Monitoring the composition and volume of amniotic fluid is important for assessing the well-being of the fetus and identifying any potential abnormalities or complications during pregnancy.
Significance of Amniotic fluid analysis
Amniotic fluid analysis holds significant importance in prenatal care and diagnosis. By examining the composition and characteristics of amniotic fluid, healthcare professionals can gather valuable information about the well-being of the fetus and assess various aspects of its development. Here are some key areas where amniotic fluid analysis holds significance:
- Diagnosis of Erythroblastosis Fetalis: Amniotic fluid analysis can help diagnose erythroblastosis fetalis, a condition that occurs when there is an incompatibility between the blood types of the mother and fetus. This condition can lead to the destruction of fetal red blood cells and cause complications. By analyzing the amniotic fluid, healthcare providers can assess the levels of bilirubin, a marker of red blood cell breakdown, and determine the severity of erythroblastosis fetalis. This information guides the management and treatment of the condition to ensure the well-being of the fetus.
- Assessment of Fetal Maturity: Amniotic fluid analysis provides valuable insights into the maturity of the fetus, especially its lung development. The presence of certain substances, such as surfactant proteins and phospholipids, in the amniotic fluid indicates the maturity of fetal lungs. This information is crucial in determining the readiness of the fetus for delivery. If the lungs are deemed mature, it suggests that the fetus has a lower risk of respiratory complications after birth.
- Genetic Counseling: Amniotic fluid analysis plays a vital role in genetic counseling and prenatal genetic testing. By examining the genetic material present in the amniotic fluid, such as cells and DNA, healthcare professionals can conduct various tests to assess the presence of genetic abnormalities, chromosomal disorders, and inherited metabolic disorders. This information helps expectant parents make informed decisions about their pregnancy and plan for the future, including potential medical interventions or specialized care for the child.
Amniotic fluid analysis is typically performed through procedures like amniocentesis, where a sample of the fluid is collected and examined in a laboratory setting. The analysis involves various techniques, including biochemical assays, cytogenetic testing, and molecular genetic analysis. These diagnostic tools provide valuable information about the health, development, and genetic makeup of the fetus, enabling healthcare providers to offer appropriate interventions, support, and counseling to expectant parents.
It is important to note that amniotic fluid analysis is an invasive procedure and carries a small risk of complications, including miscarriage. Therefore, it is typically offered to individuals with specific indications, such as advanced maternal age, abnormal prenatal screening results, or a family history of genetic disorders. The decision to undergo amniotic fluid analysis is made through careful consideration of the potential benefits and risks, in consultation with healthcare professionals and genetic counselors.
Facts on Amniotic fluid
Amniotic fluid is a complex fluid that plays a crucial role in supporting and protecting the developing fetus during pregnancy. Here are some important facts about amniotic fluid:
- Composition: Amniotic fluid contains various components, including proteins, hormones, nutrients, antibodies, and electrolytes. These substances are essential for fetal growth and development.
- Water Transfer: Water moves between different compartments within the uterus, including the placenta, fetus, and amniotic fluid. This transfer helps maintain the appropriate balance of fluids and nutrients for the fetus’s well-being.
- Changes during Gestation: As pregnancy progresses, the composition of amniotic fluid undergoes changes. For instance, after 25 weeks of gestation, there is an increase in the levels of amylase, alkaline phosphatase, urea, uric acid, creatinine, and phospholipids. On the other hand, there is a decrease in chloride, bilirubin, protein, glucose, and sodium levels.
- Diagnostic Indicators: Amniotic fluid analysis can provide important diagnostic indicators for certain conditions. An increased level of alpha-fetoprotein (AFP) in amniotic fluid suggests a neural tube defect in the fetus, while a decreased AFP level is associated with an increased risk of trisomy 21 (Down syndrome). These indicators help healthcare professionals assess the health and development of the fetus.
- Lung Maturity Assessment: The lecithin/sphingomyelin (L/S) ratio is used to measure fetal lung maturity. Lecithin is a major surfactant required for proper lung function, while sphingomyelin has no role in lung maturity. As the L/S ratio increases, it indicates increasing lung maturity, reducing the risk of respiratory distress syndrome (RDS) in newborns.
- Phosphatidylglycerol (PG): Another component involved in lung maturity assessment is phosphatidylglycerol. It is a minor lung surfactant synthesized by mature lung alveolar cells. The presence of PG in amniotic fluid indicates lung maturity.
- Bilirubin Level: Analysis of amniotic fluid for bilirubin levels can be helpful in Rh-negative mothers to assess the severity of anemia due to Rh incompatibility. This information aids in managing and monitoring the condition for the well-being of both the mother and fetus.
It is important to note that amniotic fluid analysis, including the assessment of lung maturity and other diagnostic indicators, requires specialized testing and interpretation. Healthcare professionals and laboratories perform these tests to provide valuable information for prenatal care and decision-making.
The understanding and analysis of amniotic fluid have significantly contributed to improving prenatal care and the management of various conditions during pregnancy. Continuous research and advancements in technology further enhance our knowledge of amniotic fluid and its significance in ensuring a healthy pregnancy and the well-being of the fetus.
Procedure for amniotic fluid collection
The procedure for collecting amniotic fluid, known as amniocentesis, involves the following steps:
- Transabdominal Procedure: Amniocentesis is primarily performed using a transabdominal approach. A long, sterile needle is carefully inserted through the abdominal wall into the amniotic sac, from which the amniotic fluid is aspirated. This procedure is typically safe when performed after the 14th week of gestation.
- Transvaginal Amniocentesis: In some cases, a transvaginal approach may be used for amniocentesis. However, it carries a higher risk of infection compared to the transabdominal method and is generally not the preferred route for fluid collection.
- Timing of Fluid Collection: The timing of amniotic fluid collection depends on the specific purpose of the analysis. For chromosomal analysis, fluid is usually collected after the 16th week of gestation. Fetal distress and maturity assessments are typically done in the third trimester.
- Collection of Amniotic Fluid: Approximately 30 mL of amniotic fluid is collected using sterile syringes. The first 2 to 3 mL of fluid collected are discarded to minimize the potential contamination from maternal blood, tissue fluid, and cells.
- Handling for Different Tests: The handling and storage of amniotic fluid samples depend on the specific tests being conducted:
- Hemolytic Disease of the Newborn: In cases of hemolytic disease, the sample should be protected from light. It is typically placed in an amber-colored bottle or test tube to prevent light-induced degradation.
- Fetal Lung Maturity: Samples for assessing fetal lung maturity should be kept on ice for transportation to the laboratory and stored in a refrigerator until analysis.
- Cytogenetic Testing: Samples intended for cytogenetic analysis can be maintained at room temperature (37 °C) before analysis.
- Biochemical Testing: When amniotic fluid is collected for biochemical testing, it should be separated from cellular elements and debris as soon as possible. This helps to minimize the influence of cellular metabolism on the test results.
It is important to note that amniocentesis is a specialized medical procedure that should be performed by trained healthcare professionals in appropriate clinical settings. The handling and processing of amniotic fluid samples should adhere to strict sterile techniques to ensure accurate and reliable results for diagnostic purposes.
Complications of the amniocentesis procedure
The amniocentesis procedure, although generally considered safe, carries a risk of certain complications. These potential complications include:
- Miscarriage: One of the most significant risks associated with amniocentesis is the potential for miscarriage. However, it’s important to note that the risk is relatively low, occurring in about 1 in 400 to 1 in 500 procedures.
- Fetal Injury: There is a small risk of unintentional injury to the fetus during the amniocentesis procedure. This risk is minimized by the skill and expertise of the healthcare professional performing the procedure.
- Amniotic Fluid Leak: In some cases, amniocentesis can cause a leak of amniotic fluid from the amniotic sac. While the body can often replenish the fluid, in certain situations, a significant fluid leak can lead to complications.
- Abortion: Although rare, there is a small risk of spontaneous abortion or pregnancy loss following an amniocentesis procedure. This risk is higher when the procedure is performed earlier in pregnancy.
- Premature Labor: Amniocentesis carries a slight risk of triggering premature labor. This risk is more pronounced when the procedure is performed earlier in pregnancy.
- Infections: Like any invasive medical procedure, amniocentesis carries a risk of infection. However, this risk is relatively low, and healthcare professionals take precautions to minimize the chance of infection.
- Amniotic Fluid Embolism: A rare but potentially serious complication is amniotic fluid embolism, which occurs when amniotic fluid enters the maternal bloodstream and triggers an allergic or immune reaction. This can lead to severe respiratory distress and cardiovascular collapse.
- Maternal Rh Isoimmunization: If a pregnant woman is Rh-negative and the fetus is Rh-positive, there is a small risk of Rh isoimmunization. This occurs when the mother’s immune system produces antibodies against the Rh factor in the fetal blood, potentially leading to complications in subsequent pregnancies.
- Damage to Urinary Bladder or Intestine: In very rare cases, there is a risk of accidental damage to the urinary bladder or intestine during the amniocentesis procedure. This risk is minimized by using ultrasound guidance to visualize the needle insertion.
It’s essential for healthcare professionals to thoroughly discuss the risks and benefits of amniocentesis with the pregnant individual before the procedure. They will consider the individual’s specific circumstances, medical history, and the indications for the test to determine the appropriateness and potential risks involved.
Precaution and contraindications of amniocentesis:
Precautions and contraindications for amniocentesis are important to ensure the safety and appropriateness of the procedure. Some key precautions and contraindications include:
- Fetal Blood Contamination: Fetal blood contamination during the procedure can lead to falsely elevated levels of alpha-fetoprotein (AFP). This should be taken into consideration when interpreting the results.
- Contraindications: a. Placenta Previa: Amniocentesis should not be performed in cases of placenta previa, where the placenta partially or completely covers the cervix. b. Placental Abruption: If there is a known or suspected placental abruption, amniocentesis should be avoided. c. Incompetent Cervix: Patients with an incompetent cervix, which may increase the risk of premature labor or miscarriage, should not undergo amniocentesis. d. History of Premature Labor: Individuals with a history of previous premature labor may have an increased risk of complications and should be carefully evaluated before considering amniocentesis.
- Normal Values of Amniotic Fluid: It is important to be aware of the normal values of amniotic fluid volume and various components during different stages of gestation. These values can help in interpreting the findings accurately.
| General test | Result |
|---|---|
| Appearance | clear, pale to straw yellow |
| AFP | 14 to 16 weeks = <5.2 mg/dL, 22 weeks = <3.0 mg/dL |
| Bilirubin | < 0.2 mg/dL |
| Creatinine | >2.0 mg/dL after 37 weeks |
| Chromosomal abnormality | absent |
| phosphatidylglycerol | positive (negative in immature) |
| Lecithin/sphingomyelin ratio | mature >2.0 , immature <2.0 , Diabetic mother >3.5 |
| Microscopic examination | There are amniotic epithelial cells from the lining of the sac.Fetal squamous cells originate from fetal skin, oral mucosa, and vagina. |
- Precautions during Sample Collection: a. Handling Maternal Blood Contamination: The initial 2 to 3 mL of amniotic fluid collected may be contaminated with maternal blood, tissue fluid, and cells. Therefore, this initial portion is usually discarded to prevent inaccurate results. b. Protection from Light: In cases of hemolytic disease of the newborn, where bilirubin levels are of interest, the amniotic fluid sample should be protected from light by storing it in an amber-colored bottle or test tube. c. Storage and Transport: Samples for specific tests, such as fetal lung maturity assessment, may require specific storage and transport conditions. For example, samples for fetal lung maturity assessment should be placed on ice and delivered to the laboratory promptly.
- Abnormal Findings: It is important to be familiar with abnormal findings in amniotic fluid analysis, as they can indicate various clinical conditions and guide further management.
| Lab findings | Findings | Clinical significance |
| Appearance | Yellow | Erythroblastosis (due to the presence of bilirubin) |
| Red-brown (dark red-brown) | Indicate fetal death | |
| Amber color | Indicates bilirubin | |
| Green color | Due to meconium, fetal hypoxia | |
| Pink-red (blood-streaked) | Blood contamination, traumatic tap, intra-amniotic hemorrhage | |
| Volume | Increased | Hydramnios due to fetal abnormality |
| Decrease | Oligohydramnios is associated with rupture membranes and, fetal abnormality, urinary tract deformities. | |
| Presence of cells | Long bipolar cells, multiple filamentous pseudopodia, large vacuolated cells with inclusions | Neural tube defect |
| Bilirubin | At 28 weeks = >0.075 | Erythroblastosis fetalis, hepatitis |
| At 40 weeks | Maternal infection, Sickle cell crises | |
| Saturated phosphatidylcholine | >500 µg/L | Respiratory distress syndrome |
| AFP | Increased,>2.5 MoM | Open spinal defects (neural tube defect) |
| Creatinine | >2.0 mg/dL | Indicates fetal maturity, and the maternal level is normal |
Adherence to these precautions and contraindications helps minimize the risks and ensures the safety and accuracy of the amniocentesis procedure. It is essential for healthcare professionals to carefully assess each individual’s specific situation and discuss the potential benefits and risks before proceeding with the procedure.
Amniotic fluid analysis Interpretation
Interpretation of amniotic fluid analysis involves assessing the various components and their levels to identify potential abnormalities and diagnose certain conditions. Key points for interpretation are as follows:
- Hemolytic Anemia and Rh Immunization: Increased levels of bilirubin in the amniotic fluid can indicate hemolytic anemia or Rh immunization, which is important to evaluate for fetal well-being.
- Neural Tube Defects: Elevated levels of alpha-fetoprotein (AFP) in the amniotic fluid may suggest a neural tube defect. Confirmatory testing, such as measuring acetylcholinesterase, can further support the diagnosis.
- Sacrococcygeal Teratoma: Raised AFP levels can also be observed in cases of sacrococcygeal teratoma, a tumor arising from the tailbone area.
- Fetal Distress: The presence of meconium, which gives a greenish color to the amniotic fluid, may indicate fetal distress.
- Fetal Lung Maturity: Amniotic fluid analysis can help determine fetal lung maturity. Immature lung findings may suggest an increased risk of respiratory complications.
- Hereditary Metabolic Disorders: Amniotic fluid analysis can aid in the diagnosis of hereditary metabolic disorders such as cystic fibrosis, Tay-Sachs disease, and galactosemia.
- Sex-Linked Disorders: Certain sex-linked disorders like hemophilia can be diagnosed through amniotic fluid analysis.
- Genetic Abnormalities: Chromosomal anomalies and genetic disorders like sickle cell anemia, thalassemia, and Down syndrome can be identified through amniotic fluid analysis, enabling appropriate genetic counseling and management.
- Polyhydramnios: Excessive amniotic fluid volume (polyhydramnios) in diabetic patients may increase the likelihood of congenital abnormalities.
- Oligohydramnios: Insufficient amniotic fluid volume (oligohydramnios) during gestation, particularly if less than 300 mL at 25 weeks, can be associated with fetal renal disease.
- Chromosomal Anomalies: Amniotic fluid analysis can provide a diagnosis for certain chromosomal anomalies:
- Trisomy 21: Down syndrome
- Trisomy 13: Patau syndrome
- XO 45: Turner syndrome
- XXY 47: Klinefelter syndrome
- Trisomy 18: Edwards syndrome
Interpreting the results of amniotic fluid analysis requires clinical correlation, and further diagnostic tests or consultations may be necessary to confirm and guide subsequent management decisions. It is essential for healthcare professionals to carefully evaluate and interpret the findings in the context of the individual patient’s clinical presentation and history.
Medical uses
Amniocentesis has several medical uses, including:
- Genetic Diagnosis: Amniocentesis is commonly used in early pregnancy to diagnose chromosomal abnormalities and other fetal problems. It can detect conditions such as neural tube defects (e.g., anencephaly and spina bifida) by measuring alpha-fetoprotein levels.
- Infection Detection: Amniocentesis can help identify infections in the amniotic fluid. Decreased glucose levels, the presence of bacteria seen through Gram staining, or abnormal white blood cell counts can indicate an infection.
- Lung Maturity: Amniocentesis can predict fetal lung maturity, which is crucial for assessing the risk of infant respiratory distress syndrome. One test used is the lecithin/sphingomyelin (L/S) ratio. If the L/S ratio is less than 2:1, it suggests surfactant deficiency in the fetal lungs.
- Decompression of Polyhydramnios: In cases of polyhydramnios, where there is an excessive accumulation of amniotic fluid, amniocentesis can be performed to relieve the pressure by removing some of the fluid. Additionally, it can help diagnose the underlying causes of polyhydramnios.
- Rh Incompatibility: Amniocentesis is used to diagnose Rh incompatibility, a condition where the mother has Rh-negative blood and the fetus has Rh-positive blood. Early detection is important to administer Rh immunoglobulin to the mother and provide appropriate treatment for the baby to prevent hemolytic anemia.
These medical uses of amniocentesis play a crucial role in diagnosing genetic disorders, identifying infections, assessing fetal lung maturity, managing polyhydramnios, and detecting Rh incompatibility. It is important to consider the potential risks and benefits of the procedure in each specific case and make informed decisions in consultation with healthcare professionals.