Sourav Pan
Transcript
Hey everyone! Today we’re diving into schistosomiasis, a disease you might also hear called bilharzia or snail fever.
This is what we call a neglected tropical disease, or NTD. It’s caused by tiny parasitic flatworms that have a big impact on human health.
These blood flukes are particularly sneaky because they can cause both acute problems that happen quickly, and chronic issues that develop over time.
Here’s something really important to understand: schistosomiasis is what we call a poverty-related disease. It hits hardest in communities that don’t have access to clean water and proper sanitation.
So to sum up: schistosomiasis is a parasitic disease caused by blood flukes that particularly affects vulnerable communities. Understanding this foundation helps us see why it’s such an important global health challenge.
Schistosomiasis has a very specific geographic pattern around the world. Understanding where this disease occurs helps us see why it remains such a significant global health challenge.
Africa is by far the most affected continent. An estimated 90 percent of all people who need treatment for schistosomiasis live in African countries.
Let’s look at the numbers. In 2021, at least 251.4 million people worldwide required preventive treatment for schistosomiasis.
However, only 75.3 million people actually received treatment in 2021. This means there’s a huge treatment gap – millions of people who need help but aren’t getting it.
The global impact is severe. Schistosomiasis affects more than 270,000 people worldwide and causes an estimated 11,792 deaths every year.
The key takeaway is clear: schistosomiasis is primarily an African health crisis, with the vast majority of cases concentrated in sub-Saharan Africa. The large treatment gap shows we still have much work to do.
Now we need to understand exactly what causes schistosomiasis. The culprits are a group of parasitic worms called blood flukes, and they belong to the genus Schistosoma.
These blood flukes are microscopic parasites that have evolved specifically to live inside human blood vessels. They’re quite different from other types of worms you might know about.
There are three main species of Schistosoma that cause most human infections worldwide. Each has its own characteristics and preferred locations in the body.
First is Schistosoma haematobium. This species causes urogenital schistosomiasis and is found mainly in Africa and the Middle East. It specifically targets the blood vessels around the bladder.
Second is Schistosoma mansoni. This one causes intestinal schistosomiasis and has a wider geographic distribution, found in Africa, South America, and the Caribbean. It prefers the blood vessels around the intestines.
Third is Schistosoma japonicum. This species also causes intestinal schistosomiasis but is found mainly in Asia, particularly China and the Philippines. It’s notable for producing many more eggs than the other species.
There are also several other Schistosoma species that can infect humans, though they’re less common. These include S. mekongi found in Southeast Asia, S. intercalatum in Central and West Africa, and S. guineensis in West Africa.
Interestingly, scientists have discovered that even hybrid schistosomes that normally infect cattle can sometimes cross over and infect humans. This shows just how adaptable and diverse this group of parasites can be.
The key takeaway is that schistosomiasis is caused by a diverse group of blood flukes, each with unique characteristics, geographic distributions, and preferred locations in the human body. Understanding these differences is crucial for proper diagnosis and treatment.
Now we’ll examine the physical structure of schistosomiasis worms under the microscope. Understanding their morphology is crucial for identification and diagnosis.
Adult schistosomes are elongated, tubular worms with a unique characteristic – they have separate sexes, unlike many other parasitic worms. The male and female worms live together in a remarkable partnership.
The male worm has a special groove called the gynecophoral canal. The slender female worm resides permanently within this canal, creating an intimate pairing that allows for continuous reproduction.
Now let’s examine the eggs, which are the key diagnostic feature. Each schistosome species produces eggs with distinctive shapes and spine locations that help doctors identify the specific type of infection.
Schistosoma mansoni eggs are oval-shaped with a prominent lateral spine projecting from the side. This distinctive side spine makes them easily recognizable under microscopic examination.
Schistosoma haematobium eggs are slightly more rounded and feature a terminal spine at one end. This spine points straight out from the tip of the egg, distinguishing it from other species.
Schistosoma japonicum eggs are more circular and have a very small, less conspicuous spine that can be difficult to see. This subtle spine requires careful microscopic examination for proper identification.
These morphological differences are crucial for medical diagnosis. By identifying the specific egg type in patient samples, doctors can determine which schistosome species is causing the infection and choose the most appropriate treatment approach.
Understanding schistosomiasis symptoms is crucial for early detection and treatment. However, this disease can be tricky because many people show no symptoms at all.
The first important fact about schistosomiasis is that many infected people are completely asymptomatic. This means they have no visible signs of illness, making the disease particularly dangerous because it can go undetected for years.
For those who do develop symptoms, schistosomiasis follows a predictable timeline. Symptoms appear in distinct phases, starting with early skin reactions and progressing to more serious complications.
Early symptoms typically appear within days to weeks of infection. The most common early signs are itchy skin and a rash where the parasites entered the body. This happens because the immune system is reacting to the foreign invaders.
Two to eight weeks after infection, some people develop what’s called Katayama fever. This is a more serious phase with flu-like symptoms including fever, chills, cough, muscle aches, and abdominal pain. This represents the body’s intense immune response to the parasites.
If left untreated, schistosomiasis can develop into a chronic condition with serious complications. These include persistent abdominal pain, bloody diarrhea, blood in urine, liver enlargement, kidney damage, infertility, and in severe cases, even bladder cancer.
The key takeaway is that schistosomiasis symptoms can range from completely absent to life-threatening. Early detection and treatment are crucial to prevent serious complications. If you’ve been in areas where schistosomiasis is common and experience any of these symptoms, seek medical attention promptly.
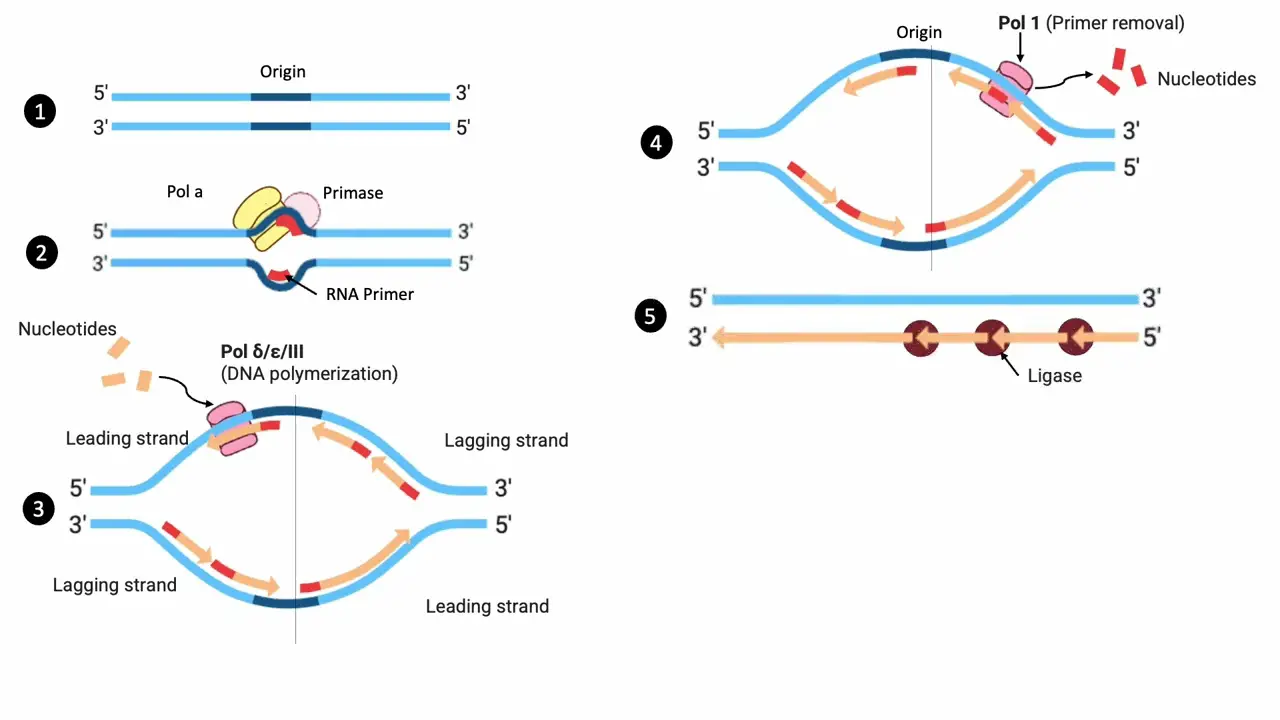
Understanding the schistosomiasis life cycle is crucial for grasping how this parasitic disease spreads and perpetuates itself. This complex cycle involves multiple stages and two different hosts.
The cycle begins when infected humans release schistosome eggs into freshwater through their feces or urine. These microscopic eggs are the starting point of the entire transmission cycle.
Once in water, these eggs hatch and release free-swimming larvae called miracidia. These tiny organisms are equipped with cilia that help them move through the water in search of their next host.
The miracidia must find and penetrate specific species of freshwater snails within hours, or they will die. Once they successfully infect a snail, they begin the next phase of development.
Inside the snail, miracidia transform into sporocysts. These sporocysts then reproduce asexually, producing hundreds of new larvae called cercariae. This amplification stage is critical for the parasite’s success.
After several weeks of development, mature cercariae are released from the infected snail back into the water. These fork-tailed larvae can survive in water for up to 48 hours while searching for a human host.
When humans come into contact with contaminated water, cercariae penetrate the skin within minutes. They can penetrate intact skin, making any water contact potentially dangerous in endemic areas.
Once inside the human body, cercariae lose their tails and become schistosomulae. These juvenile worms migrate through the bloodstream to the liver, where they mature into adult worms over several weeks.
Adult worms then migrate to their final destination – either the mesenteric venules around the intestines or the venous plexus of the bladder, depending on the species. Here they mate and begin producing eggs, completing the cycle.
The cycle continues as these adult worms can live for years, constantly producing eggs that are released back into the environment through human waste, perpetuating the transmission cycle.
This complex life cycle explains why schistosomiasis is so persistent in endemic areas and why breaking the cycle requires comprehensive control measures targeting both human treatment and environmental factors.
Understanding how schistosomiasis spreads is crucial for prevention. The transmission occurs through a specific pathway involving contaminated freshwater and human contact.
Infected freshwater snails are the key to transmission. These snails release microscopic larvae called cercariae into the water. These tiny parasites are invisible to the naked eye but are actively swimming and seeking human hosts.
People become infected when they come into contact with this contaminated water during various daily activities. Let’s look at the main ways humans are exposed to these parasites.
Agricultural activities are a major source of exposure. Farmers working in rice paddies, irrigation channels, or crop fields often wade through contaminated water. The parasites can penetrate skin within minutes of contact.
Domestic activities also pose significant risks. Washing clothes, collecting water for household use, or bathing in rivers and lakes can lead to infection. Women and children are often at higher risk due to these daily water-related tasks.
Recreational water activities are particularly dangerous because people often spend extended time in the water. Swimming, wading, fishing, or playing in contaminated freshwater gives parasites ample opportunity to penetrate the skin.
The actual transmission happens when cercariae penetrate human skin. These parasites can burrow through intact skin in just a few minutes. They don’t need cuts or wounds – healthy skin provides no barrier against these microscopic invaders.
The key takeaway is that any contact with contaminated freshwater poses a risk. Even brief exposure can lead to infection. The parasites are invisible, so contaminated water looks exactly like clean water, making this disease particularly dangerous for communities that depend on natural water sources.
Diagnosing schistosomiasis requires detective work. Doctors use several methods to find evidence of these parasitic worms in the human body.
The most common diagnostic method is finding parasite eggs in stool or urine samples. This is like looking for fingerprints – the eggs are direct evidence that worms are present in the body.
Under the microscope, doctors look for the distinctive eggs of schistosoma worms. Each species has uniquely shaped eggs – some with spines on the side, others with spines at the end.
The second method detects antibodies or antigens in blood or urine samples. When the body fights schistosoma infection, it produces specific antibodies that can be measured in laboratory tests.
For urogenital schistosomiasis, doctors use a special filtration technique. Urine is passed through a fine filter that traps the eggs, making them easier to see under a microscope.
The quickest screening method uses chemical reagent strips. These strips detect microscopic blood in urine, which often indicates schistosoma infection. It’s like a pregnancy test but for parasites – quick, easy, and gives immediate results.
Doctors have multiple tools in their diagnostic toolkit. Egg detection provides definitive proof, antibody tests show immune response, filtration concentrates evidence, and reagent strips offer quick screening. Together, these methods help doctors accurately diagnose schistosomiasis and start treatment promptly.
When it comes to treating schistosomiasis, there’s one medication that stands out as the gold standard: praziquantel. This remarkable drug has revolutionized the treatment of this parasitic disease.
Praziquantel is the recommended treatment for all forms of schistosomiasis. What makes it so special? It’s highly effective against the parasites, remarkably safe for patients, and importantly, it’s low-cost, making it accessible in resource-limited settings.
Praziquantel demonstrates remarkable effectiveness with cure rates between 85 to 95 percent. Here we can see the dramatic reduction in parasites before and after treatment with a single dose.
A major breakthrough in schistosomiasis treatment is the development of arpraziquantel, a new pediatric formulation specifically designed for young children. Unlike traditional tablets, this is a dispersible tablet that dissolves easily.
Arpraziquantel offers three major advantages. First, it’s child-friendly and palatable, making it much easier for young children to take. Second, it’s stable in tropical climates where schistosomiasis is most common. Third, as a dispersible tablet, it can be mixed with water or food.
This breakthrough makes treatment accessible for preschool-aged children, a population that was previously difficult to treat effectively. The European Medicines Agency has given it a positive scientific opinion, and it’s included in the World Health Organization’s list of prequalified medicines.
Praziquantel and its new pediatric formulation represent a powerful tool in the fight against schistosomiasis. With high effectiveness, excellent safety profile, and now improved accessibility for children, these treatments are truly rescuing millions from this debilitating disease.
Preventing schistosomiasis requires a comprehensive approach with multiple strategies working together. Think of it like building a strong defense system with several layers of protection.
The first and most important strategy is periodic, large-scale population treatment with praziquantel. This involves treating entire communities at regular intervals, typically once or twice per year.
Improving access to safe water and sanitation is crucial for breaking the transmission cycle. Clean water sources and proper toilets prevent contamination of freshwater bodies where the snails live.
Snail control measures target the intermediate host in the parasite’s life cycle. By reducing snail populations in freshwater bodies, we can break the transmission chain and prevent new infections.
Hygiene education and promoting behavior change are essential for long-term prevention. Teaching communities about the risks and how to avoid contaminated water helps people protect themselves and their families.
The most effective prevention strategy combines all these approaches into an integrated control program. When mass treatment, improved sanitation, snail control, and education work together, they create a powerful defense against schistosomiasis transmission.
The World Health Organization plays a crucial role in coordinating global efforts to combat neglected tropical diseases. For schistosomiasis specifically, WHO has established clear, ambitious goals to reduce the burden of this disease worldwide.
WHO established specific timeline goals for schistosomiasis. The first major target was to achieve control of schistosomiasis as a public health problem by 2020. The ultimate goal is complete elimination as a public health problem by 2025.
These schistosomiasis goals are part of a much larger initiative. In 2021, WHO launched an ambitious roadmap covering the decade from 2021 to 2030. This comprehensive strategy targets 20 different neglected tropical diseases with four main approaches.
The roadmap addresses 20 major neglected tropical diseases affecting over 1.7 billion people worldwide. Schistosomiasis is prominently featured as one of the priority diseases, alongside conditions like lymphatic filariasis, trachoma, and soil-transmitted helminths.
The roadmap establishes specific, measurable targets for schistosomiasis. These include reducing disease-related morbidity by 75 percent by 2030, eliminating transmission in all endemic villages, and expanding treatment programs to include preschool-aged children who were previously underserved.
The WHO roadmap represents more than just goals on paper. It provides a comprehensive framework for coordinated global action, bringing together countries, international partners, and local communities in the fight against schistosomiasis and other neglected tropical diseases.
A major breakthrough in schistosomiasis treatment has emerged specifically for our youngest patients. Arpraziquantel represents a significant advancement in pediatric care for preschool-aged children.
Traditional praziquantel tablets pose challenges for young children. They are hard to swallow, have a bitter taste, and are not suitable for preschool-aged children who need treatment.
Arpraziquantel solves these problems with its innovative design. It’s a dispersible tablet that dissolves easily in water, has a child-friendly taste, and is specifically formulated for preschool-aged children.
The first key feature is that arpraziquantel is dispersible. The tablet easily dissolves in water, creating a liquid medicine that young children can drink without difficulty.
Arpraziquantel is specifically designed to remain stable in tropical climates. Unlike many medications that degrade in heat and humidity, this formulation maintains its effectiveness in challenging environmental conditions.
Arpraziquantel has achieved significant regulatory milestones. It received a positive scientific opinion from the European Medicines Agency, demonstrating its safety and efficacy for pediatric use.
The medication is currently included in the World Health Organization’s List of Prequalified Medicines, ensuring it meets international quality standards for global distribution.
Looking ahead, arpraziquantel is expected to be included in the WHO List of Essential Medicines in 2025, which will further facilitate its availability and use in endemic countries worldwide.
Arpraziquantel represents a game-changer for pediatric schistosomiasis treatment. It enables healthcare workers to treat preschool-aged children effectively, improves compliance through its child-friendly formulation, and remains stable in resource-limited settings where it’s needed most.
This pediatric formulation fills a critical gap in schistosomiasis treatment, ensuring that even the youngest patients can receive safe and effective therapy. It represents a significant step forward in the global effort to control and eliminate schistosomiasis.
Senegal has become a pioneering example in the fight against schistosomiasis, implementing one of the most comprehensive rollout plans for pediatric praziquantel treatment in Africa.
The rollout focuses on high-prevalence regions across Senegal, where schistosomiasis affects significant portions of the population, particularly preschool-aged children who were previously underserved by treatment programs.
The implementation plan includes four key components: community engagement to build trust and awareness, healthcare worker training on pediatric treatment protocols, robust supply chain management for medication distribution, and comprehensive data collection for monitoring progress.
Central to the Senegal rollout is an innovative implementation research study that examines integrated strategies for delivering pediatric praziquantel treatment effectively.
The research study compares four different delivery strategies: school-based programs, community outreach initiatives, integration with existing health facilities, and mobile clinic approaches. Each strategy is evaluated for effectiveness, cost, and community acceptance.
This comprehensive approach is generating valuable insights that will inform schistosomiasis control programs across sub-Saharan Africa and other high-prevalence regions worldwide.
The Senegal rollout is expected to provide crucial insights into optimal delivery strategies for different settings, cost-effectiveness of integrated approaches, and best practices for community engagement. These findings will create a scalable model for global implementation of pediatric schistosomiasis treatment programs.
Senegal’s pioneering approach demonstrates how systematic implementation research can transform global health interventions, providing evidence-based strategies that can be adapted and scaled to eliminate schistosomiasis in children worldwide.
Traditional schistosomiasis diagnosis relies on finding parasite eggs under a microscope. But this method has limitations – it can miss infections when egg counts are low, and requires skilled technicians.
Enter molecular diagnostics – PCR and LAMP. These advanced techniques don’t look for eggs. Instead, they detect the parasite’s DNA directly, making them much more sensitive and accurate.
PCR, or Polymerase Chain Reaction, amplifies tiny amounts of parasite DNA millions of times. This makes it possible to detect even very small numbers of parasites that traditional microscopy would miss completely.
LAMP, or Loop-mediated Isothermal Amplification, is even simpler. It works at a constant temperature and gives results faster than PCR. This makes it perfect for field testing in remote areas where schistosomiasis is common.
The key advantage of these molecular methods is their superior sensitivity and specificity. Sensitivity means they catch more true infections, while specificity means they avoid false positives. This leads to better patient care and more effective disease control.
These diagnostic advances are game-changers for schistosomiasis control. They enable earlier detection, more accurate monitoring of treatment programs, and better tracking of disease elimination efforts. This technology brings us closer to the goal of eliminating schistosomiasis as a public health problem.
Machine learning is revolutionizing how we diagnose schistosomiasis. These intelligent computer systems can analyze vast amounts of diagnostic data to find patterns that human eyes might miss.
Traditional schistosomiasis diagnosis relies on manual microscopic examination. Technicians visually inspect samples, manually count parasites, and interpret results based on their experience. This process is time-consuming and can vary between different observers.
Machine learning transforms this process by using computer algorithms that can recognize patterns in diagnostic images and data. These systems analyze thousands of samples to learn what schistosomiasis infections look like, becoming incredibly accurate at detection.
Machine learning works like a digital brain. It takes multiple types of diagnostic data as input – microscopic images, laboratory test results, and patient information. The algorithm processes this data through multiple layers, learning to recognize patterns that indicate schistosomiasis infection.
When new diagnostic data enters the system, it flows through the network. Each layer processes the information, identifying specific features like egg shapes, parasite characteristics, or blood markers that are associated with schistosomiasis.
The results are impressive. Traditional diagnostic methods typically achieve around seventy-five percent accuracy. Machine learning enhanced systems can reach ninety-five percent accuracy or higher, significantly reducing missed diagnoses and false positives.
Machine learning brings multiple benefits to schistosomiasis diagnosis. Results are available in minutes rather than hours, accuracy is significantly higher, results are more consistent between different facilities, and patients receive earlier treatment leading to better health outcomes.
This technology is already being implemented in research settings and clinical trials. As machine learning continues to advance, we can expect even more accurate and accessible diagnostic tools for schistosomiasis, bringing better healthcare to communities that need it most.
Urogenital schistosomiasis affects women differently than men, causing specific symptoms in the female reproductive and urinary systems. Understanding these symptoms is crucial for proper diagnosis and treatment.
The first major symptom is genital lesions. These are abnormal tissue changes or sores that can develop on the external genital area, including the vulva and surrounding tissues.
Women may experience abnormal vaginal bleeding that is not related to their menstrual cycle. This bleeding can be irregular and may occur between periods or after menopause.
Another significant symptom is dyspareunia, or pain during sexual intercourse. This can severely impact a woman’s quality of life and intimate relationships.
Women may also develop nodules in the vulva. These are small, firm lumps that can be felt under the skin and may cause discomfort or tenderness.
These symptoms are often overlooked or misdiagnosed because they can be confused with other gynecological conditions. This is why awareness among healthcare providers and women themselves is so important.
Early recognition of these symptoms can lead to timely diagnosis and treatment, preventing long-term complications and improving women’s reproductive health and overall quality of life.
Controlling schistosomiasis requires more than just treating infected people. We need integrated control measures that address multiple aspects of transmission simultaneously.
Single control strategies often fail because schistosomiasis transmission involves complex interactions between humans, parasites, snails, and the environment.
Integrated control combines four essential pillars that work together to break the transmission cycle at multiple points.
The first pillar is treatment with praziquantel to eliminate adult worms in infected individuals and reduce egg production.
The second pillar is snail control to eliminate the intermediate hosts that are essential for parasite development.
The third pillar is hygiene education to teach communities how to avoid contaminated water and practice safe behaviors.
The fourth pillar is providing access to safe water and sanitation to prevent contamination and reduce human contact with infected water.
These four pillars work synergistically. When combined, they create multiple barriers that interrupt transmission at different stages of the parasite life cycle.
This integrated approach is especially important for Schistosoma japonicum, which has unique transmission patterns involving multiple animal hosts and specific snail species.
The key takeaway is that no single intervention can eliminate schistosomiasis. Only through integrated control measures that address treatment, snail control, education, and sanitation can we achieve sustainable control and eventual elimination.
Vaccine development represents the most promising long-term solution for preventing schistosomiasis. Scientists around the world are working to create vaccines that could protect millions of people from this parasitic disease.
Currently, multiple schistosomiasis vaccine candidates are in various stages of development. Clinical trials are being conducted worldwide, and the World Health Organization has designated schistosomiasis vaccines as a high priority for global health.
Vaccines are considered high priority because they offer prevention rather than treatment. While current approaches require repeated medication for over 251 million people annually, a successful vaccine could provide long-term protection and create a clear path toward disease elimination.
Researchers are pursuing multiple vaccine approaches. Recombinant protein vaccines use specific parasite proteins to trigger immunity. Live attenuated vaccines use weakened parasites for safe immunization. DNA vaccines deliver genetic material to stimulate immune responses. However, challenges include the parasite’s complex life cycle, its ability to evade the immune system, and the need for long-lasting protection.
A successful schistosomiasis vaccine could dramatically transform global health. Instead of treating over 251 million people annually and facing nearly 12,000 deaths per year, vaccines could prevent new infections, reduce complications, and create a clear pathway to disease elimination worldwide.
The timeline for vaccine development spans many years. Current research includes preclinical studies and early phase trials. Within 5 to 10 years, we expect to see advanced clinical trials. A successful vaccine could be available in 10 or more years. Vaccines represent our best hope for long-term schistosomiasis prevention and eventual elimination of this devastating disease.
Climate change is creating new challenges in the fight against schistosomiasis. Rising temperatures and changing rainfall patterns are directly affecting how this parasitic disease spreads across the globe.
Warmer temperatures create ideal conditions for freshwater snails, the intermediate hosts of Schistosoma mansoni. As global temperatures rise, snail populations can survive and reproduce in areas that were previously too cold, expanding the geographic range of schistosomiasis.
Climate change also alters rainfall patterns, creating both droughts and floods. Increased rainfall expands freshwater habitats where snails thrive, while droughts can concentrate both snails and people around remaining water sources, increasing transmission risk.
As climate conditions change, Schistosoma mansoni is spreading into previously unaffected regions. Areas that were once too cold or dry are becoming suitable for snail populations and parasite transmission, creating new public health challenges.
Climate change complicates schistosomiasis control efforts significantly. Traditional control programs must adapt to unpredictable transmission patterns, monitor new endemic areas, and reallocate resources as the disease spreads to previously unaffected regions.
The relationship between climate change and schistosomiasis demonstrates how environmental factors directly impact disease transmission. Understanding these connections is crucial for developing effective, adaptive control strategies that can respond to our changing climate.
Hybrid schistosomes represent an emerging challenge in parasitology that’s making disease control more complicated than ever before.
But what exactly are hybrid schistosomes? Think of them as the offspring when two different species of schistosome parasites crossbreed, creating new parasites with mixed characteristics.
When these different species interbreed, they create hybrid offspring that combine genetic material from both parents, resulting in parasites with unpredictable traits.
These hybrids are particularly concerning because they can inherit unexpected combinations of traits that make them harder to detect, treat, and control.
First, hybrid schistosomes can have different transmission patterns. They might infect new types of snail hosts or survive in different water conditions, expanding where the disease can spread.
Second, they complicate diagnosis. Standard tests designed for known species might miss these hybrids or give confusing results, making it harder for doctors to identify infections.
Most importantly, hybrid schistosomes can undermine control programs. Treatments and prevention strategies designed for specific species might be less effective against these genetic mixtures.
The scientific community recognizes that much more research is urgently needed. We need to understand how common these hybrids are, where they occur, and how to adapt our control strategies.
Hybrid schistosomes represent a growing concern that could significantly impact global efforts to eliminate schistosomiasis. Understanding and addressing this challenge is crucial for protecting public health worldwide.
The World Health Organization recognizes that controlling schistosomiasis requires more than just treating humans. We need a One Health approach that considers the interconnected health of humans, animals, and the environment.
One Health is an integrated approach that recognizes the interconnection between human health, animal health, and environmental health. These three domains are deeply connected and influence each other.
In schistosomiasis control, the One Health approach means coordinating efforts across all three domains. For humans, we focus on treatment and education. For animals, we extend treatment to livestock and monitor wildlife reservoirs. For the environment, we control snail populations and manage water systems.
Animals play a crucial role in schistosomiasis transmission. Cattle and other livestock can serve as reservoir hosts, maintaining the parasite life cycle even when human infections are reduced. This is why WHO recognizes that treating only humans is not enough for effective control.
The One Health approach offers significant benefits for schistosomiasis control. It provides more effective and sustainable solutions by addressing the disease at its source. This integrated strategy is more cost-efficient and helps reduce reinfection rates by breaking transmission cycles across all domains.
The One Health approach represents the future of schistosomiasis control. By working across human, animal, and environmental health sectors, we can achieve more comprehensive and lasting results in the fight against this neglected tropical disease.
Expert opinions and comprehensive statistics reveal the true scope and impact of schistosomiasis as a global health challenge. The data tells a compelling story of both the burden and the economic opportunities in addressing this neglected tropical disease.
The schistosomiasis treatment market represents a significant economic opportunity. In 2024, the market reached a value of 53.5 million US dollars across the top seven markets, including the United States, European Union, United Kingdom, and Japan.
Market projections show continued growth, with the value expected to reach 74.1 million dollars by 2035. This represents a 38 percent increase over eleven years, reflecting growing investment in schistosomiasis research and treatment development.
The global burden statistics paint a sobering picture. In 2021, at least 251.4 million people required preventive treatment for schistosomiasis worldwide. However, only 75.3 million people were actually reported to have received treatment.
This reveals a significant treatment gap of 176.1 million people who needed but did not receive preventive treatment. This gap represents one of the major challenges in global schistosomiasis control efforts.
Africa bears the heaviest burden of schistosomiasis. An estimated 90 percent of all people requiring treatment for schistosomiasis live in African countries. This geographic concentration makes Africa the primary focus for elimination efforts.
The health impact is substantial. Schistosomiasis affects more than 270,000 people globally and causes an estimated 11,792 deaths per year worldwide. The disease burden amounts to approximately 3.31 million disability-adjusted life years.
Leading organizations are working toward ambitious elimination goals. The World Health Organization aims to eliminate the transmission and incidence of schistosomiasis in all endemic villages by 2025, representing a critical milestone in global health.
The Global Schistosomiasis Alliance is working to accelerate progress towards schistosomiasis control and elimination. This collaborative effort brings together researchers, policymakers, and health organizations to coordinate global response efforts.
These statistics and expert opinions highlight both the challenges and opportunities in schistosomiasis control. While the treatment gap remains significant, growing market investment and coordinated global efforts provide hope for achieving elimination goals.
As we conclude our exploration of schistosomiasis, let’s review the key takeaways and look toward the future of this important public health challenge.
Schistosomiasis remains a significant public health challenge, affecting over 250 million people worldwide, with 90 percent of cases occurring in Africa.
We’re making significant progress on multiple fronts. Advanced research is improving our diagnostic capabilities with PCR and LAMP technologies, while machine learning is enhancing accuracy. New treatments like arpraziquantel are making care accessible to children, and integrated control measures are taking a comprehensive approach to prevention.
Prevention remains crucial and rests on three fundamental pillars: access to clean water, proper sanitation systems, and comprehensive hygiene education. These elements work together to break the transmission cycle of schistosomiasis.
Looking ahead, the World Health Organization has set ambitious goals: elimination of schistosomiasis as a public health problem by 2025, and complete elimination by 2030. Achieving these goals requires continued global collaboration and sustained commitment.
Together, we can make a difference in the fight against schistosomiasis. Stay informed about neglected tropical diseases, support control efforts, advocate for clean water access, and promote hygiene education. Remember, every action counts in creating a world free from schistosomiasis.
Study Materials
Schistosomiasis - Life cycle, Symptoms, Treatment, Prevention
Helpful: 0%
Related Videos

- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.