AQA GCSE Biology 12 Views 1 Answers
Sourav PanLv 9November 12, 2024
Why do resistant strains, like MRSA, pose a significant challenge to treatment, and how do they spread?
Why do resistant strains, like MRSA, pose a significant challenge to treatment, and how do they spread?
Please login to save the post
Please login to submit an answer.
Sourav PanLv 9May 15, 2025
Methicillin-resistant Staphylococcus aureus (MRSA) poses a significant challenge to treatment due to its inherent resistance to multiple antibiotics and its ability to spread rapidly within communities and healthcare settings. Here’s an overview of the factors contributing to the challenges MRSA presents and the mechanisms of its spread.
Challenges Posed by MRSA
- Antibiotic Resistance:
- MRSA is resistant to methicillin and other beta-lactam antibiotics, which are commonly used to treat staphylococcal infections. This resistance arises from the acquisition of the mecA gene, which encodes a modified penicillin-binding protein that reduces the effectiveness of these antibiotics.
- In addition to methicillin, MRSA can exhibit resistance to multiple other antibiotic classes, complicating treatment options. The presence of strains with intermediate resistance to vancomycin (VISA) further exacerbates treatment difficulties, as these strains require prolonged therapy and are associated with more severe infections .
- Clinical Manifestations:
- MRSA infections can range from mild skin infections to severe conditions such as bloodstream infections, pneumonia, and surgical site infections. The variability in clinical presentation complicates diagnosis and treatment strategies .
- Limited Treatment Options:
- While newer antimicrobials are being developed, the options for effectively treating MRSA infections remain limited. The emergence of resistance to last-resort antibiotics like vancomycin raises concerns about future treatment failures.
Mechanisms of Spread
- Transmission Routes:
- Direct Contact: MRSA spreads through direct contact with infected individuals or carriers. This includes skin-to-skin contact during activities such as sports or healthcare interactions .
- Contaminated Surfaces: The bacteria can survive on surfaces (fomites) such as medical equipment, bedding, and doorknobs, facilitating transmission in healthcare settings and community environments .
- Respiratory Droplets: Although less common, MRSA can also spread through respiratory droplets when an infected person coughs or sneezes .
- Colonization:
- Many individuals can carry MRSA asymptomatically, particularly in the nasal passages or skin, serving as reservoirs for transmission without showing signs of infection . This colonization allows for the bacteria to spread silently within populations.
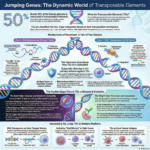
- Horizontal Gene Transfer:
- MRSA can acquire resistance genes through horizontal gene transfer mechanisms such as conjugation, transformation, or transduction. This capability enables the rapid spread of antibiotic resistance among different strains and species of bacteria . For example, methicillin-sensitive Staphylococcus aureus (MSSA) can acquire the mecA gene from resistant strains through mobile genetic elements.
- Environmental Factors:
- Poor hygiene practices, overcrowding in healthcare facilities or community settings, and inadequate infection control measures contribute significantly to the spread of MRSA . The global movement of people and animals also facilitates the dissemination of resistant strains across regions.
0
0 likes
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
0 found this helpful out of 0 votes
Helpful: 0%
Helpful: 0%
Was this page helpful?