What is Parathyroid Gland?
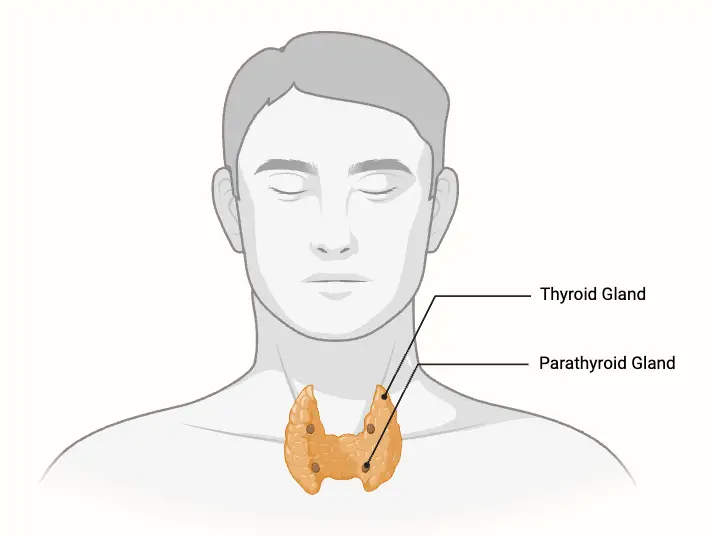
- The parathyroid glands are small, vital endocrine organs located in the neck, typically on the posterior surface of the thyroid gland. Most individuals have four parathyroid glands, although this number can vary, with some individuals having as many as eight. These glands are crucial for maintaining calcium homeostasis in the body, which is essential for numerous physiological processes such as muscle contraction, nerve transmission, and bone strength.
- The primary function of the parathyroid glands is to produce and secrete parathyroid hormone (PTH) in response to low blood calcium levels. PTH increases blood calcium by promoting calcium release from bones, enhancing calcium reabsorption in the kidneys, and increasing calcium absorption from the small intestine. This hormone ensures that the body’s calcium levels remain within a narrow range, which is critical for proper functioning.
- Embryologically, the parathyroid glands originate from the third and fourth pharyngeal pouches. The superior glands arise from the fourth pouch, while the inferior glands develop from the third pouch. These glands share their blood supply, venous drainage, and lymphatic systems with the thyroid gland, reflecting their close anatomical relationship.
- Dysfunction of the parathyroid glands can lead to significant health problems. Hyperparathyroidism, characterized by excessive PTH secretion, can result in elevated blood calcium levels, leading to weakened bones, kidney stones, and other complications. In contrast, hypoparathyroidism, which involves insufficient PTH production, can cause dangerously low calcium levels, affecting muscle and nerve function.
- The number and exact positioning of the parathyroid glands may vary, with some individuals having ectopic parathyroid glands located elsewhere in the neck or thorax. However, regardless of their number or location, their role in regulating calcium remains consistent and crucial for overall health.
Definition of Parathyroid Gland
The parathyroid glands are small endocrine glands located behind the thyroid gland that regulate calcium levels in the blood by secreting parathyroid hormone (PTH). This hormone helps maintain calcium balance by influencing the bones, kidneys, and intestines.
Anatomical Location of Parathyroid Gland
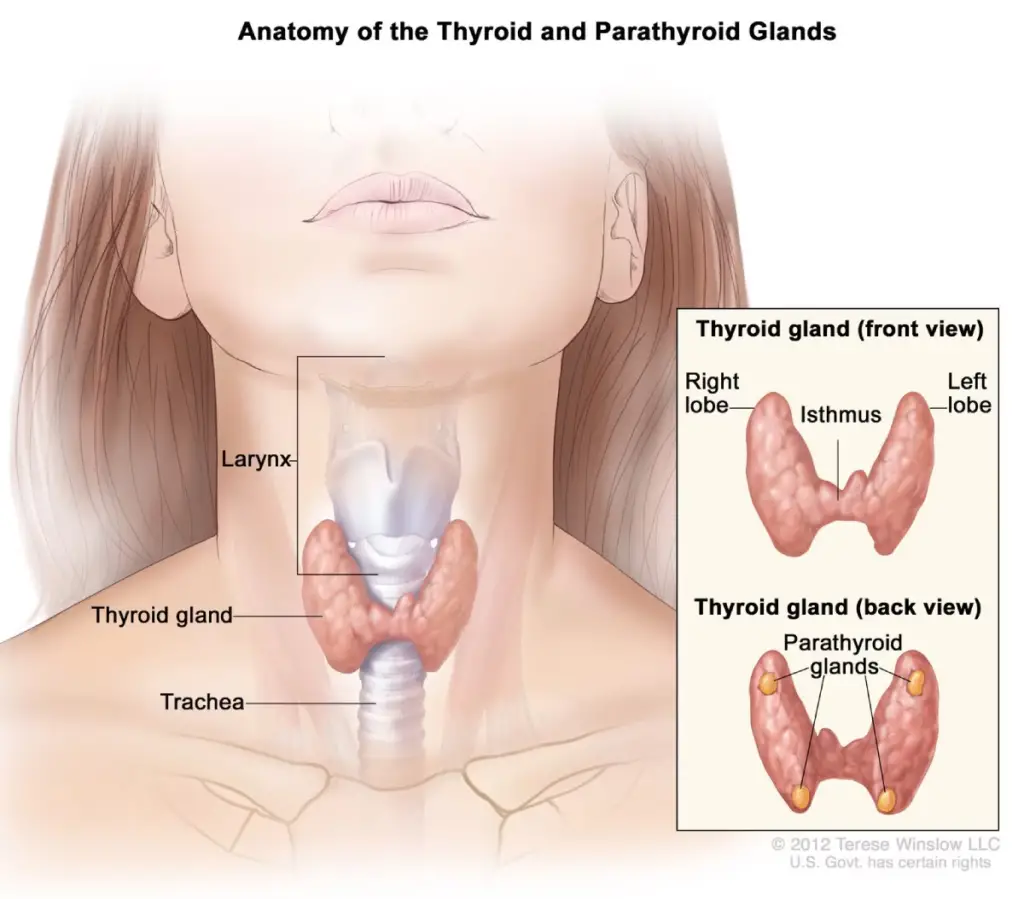
The parathyroid glands are small, flattened, oval-shaped endocrine structures typically located on the posterior side of the thyroid gland. Their primary role is to regulate calcium levels in the body. Below is a detailed explanation of the anatomical location of these glands:
- Location:
- The parathyroid glands are situated external to the thyroid gland but within the pretracheal fascia.
- Most people have four parathyroid glands, but variations in number (ranging from two to six) are common.
- Superior Parathyroid Glands (x2):
- Derived from the fourth pharyngeal pouch.
- Typically located on the middle part of the posterior border of each thyroid lobe.
- Positioned about 1 cm above the point where the inferior thyroid artery enters the thyroid gland.
- Inferior Parathyroid Glands (x2):
- Derived from the third pharyngeal pouch.
- Their location is more variable compared to the superior glands, but they are generally found near the inferior poles of the thyroid gland.
- In some cases, the inferior parathyroid glands may be located as far down as the superior mediastinum, an area in the chest cavity.
- Variation in Location and Number:
- The number and location of the parathyroid glands can differ among individuals. Ectopic parathyroid glands, which occur outside their typical location, may be present, particularly in the mediastinum or other areas of the neck.
Structure of Parathyroid Gland
The parathyroid glands are small nodular endocrine structures located on the posterior side of the thyroid gland. Typically, there are four parathyroid glands, although their number and location can vary. These glands play a crucial role in regulating calcium levels in the body. Below is a detailed description of the structure of the parathyroid glands:
- Origin: The parathyroid glands are derived from endodermal tissue and are located on the dorsal side of the thyroid gland.
- Number and Location: Generally, four glands are present, with two superior and two inferior glands positioned at the upper and lower poles of the thyroid. However, the number of glands can vary, with some individuals having more or fewer than four. These glands can also be located ectopically in areas like the mediastinum.
- Blood Supply: The primary blood supply comes from the inferior thyroid artery, although the superior thyroid artery may also contribute. The superior parathyroids are typically found near the cricothyroid junction, while the location of the inferior parathyroids is less consistent.
- Capsule: Each gland is surrounded by a fibrous capsule made of fine connective tissue. This capsule separates the glandular tissue of the parathyroid from the thyroid.
- Parenchyma: The functional tissue, or parenchyma, of the parathyroid glands is composed of two main types of cells:
- Chief Cells:
- These are the primary functional cells responsible for both the synthesis and secretion of parathyroid hormone (PTH).
- Chief cells contain calcium-sensing receptors (CaSR), which are G protein-coupled receptors that detect changes in blood calcium levels and regulate the release of PTH accordingly.
- Oxyphil Cells:
- These cells do not have a known endocrine function, and their number tends to increase with age.
- Although they are abundant in older individuals, their exact role in the parathyroid gland remains unclear.
- Chief Cells:
- Size and Weight: The size of the parathyroid glands can vary among individuals, but on average, each gland weighs about 50 milligrams.
- Histology: The parathyroid glands are arranged in columns of spherical cells surrounded by sinusoids, which are small blood vessels that supply the gland with blood.
Microanatomy of Parathyroid Gland
The microanatomy of the parathyroid gland is essential for understanding its functional role in calcium homeostasis. These small, pea-sized glands are typically located on the posterior aspect of the thyroid gland and are integral in regulating parathyroid hormone (PTH) secretion. Below is a detailed overview of the cellular composition and structural features of the parathyroid gland:
- Cell Types:
- Chief Cells:
- These are the predominant cells in the parathyroid gland, responsible for synthesizing and secreting parathyroid hormone.
- Chief cells are small and exhibit a dark staining pattern when filled with PTH, reflecting their active state. In contrast, when PTH is secreted, they appear clear or less dense.
- The primary function of chief cells is to monitor blood calcium levels and release PTH in response to hypocalcemia (low calcium levels), thus playing a crucial role in calcium regulation.
- Oxyphil Cells:
- Oxyphil cells are less abundant and larger than chief cells. They appear lighter in staining due to their lower content of secretory granules.
- The exact function of oxyphil cells remains uncertain; however, their numbers tend to increase with age, suggesting a potential role in the aging process or metabolic regulation.
- Some theories propose that oxyphil cells may have a supportive role in the parathyroid gland’s function or could be involved in producing certain proteins.
- Chief Cells:
- Glandular Architecture:
- The parathyroid glands are typically encapsulated by a thin connective tissue capsule, which helps maintain their structural integrity.
- The arrangement of chief and oxyphil cells creates a densely packed cellular environment, differentiating them from the follicular structure observed in the thyroid gland.
- Vascularization is significant, providing the necessary blood supply for hormone delivery and ensuring effective communication with other organs involved in calcium metabolism.
- Histological Characteristics:
- Microscopic examination of the parathyroid gland reveals clusters of chief cells interspersed with oxyphil cells, demonstrating a unique cellular architecture.
- The presence of adipose tissue may also be noted, particularly in older individuals, which can influence the function of the parathyroid glands over time.
- Functional Relevance:
- The primary function of the parathyroid glands is to maintain calcium homeostasis. The secretion of PTH by chief cells increases serum calcium levels by promoting:
- Bone resorption: PTH stimulates osteoclast activity, leading to the release of calcium from bones.
- Renal reabsorption: PTH promotes the reabsorption of calcium in the kidneys while encouraging phosphate excretion.
- Gastrointestinal absorption: While the parathyroid gland itself does not directly affect the gastrointestinal tract, PTH facilitates the synthesis of active vitamin D, enhancing intestinal absorption of calcium and phosphate.
- The primary function of the parathyroid glands is to maintain calcium homeostasis. The secretion of PTH by chief cells increases serum calcium levels by promoting:
Hormones of Parathyroid Gland
The parathyroid glands produce parathyroid hormone (PTH), also known as parathormone, which plays a crucial role in regulating calcium levels in the blood. Maintaining calcium homeostasis is vital for processes such as nerve impulse transmission, muscle contraction, and blood clotting. The following points outline the functions and mechanisms of the parathyroid hormone:
- Parathyroid Hormone (PTH):
- The primary hormone produced by the parathyroid glands is PTH, which regulates blood calcium levels.
- PTH is secreted when calcium levels in the blood drop, detected by receptors on the chief cells of the parathyroid gland.
- Action in the Bones:
- PTH stimulates osteoclasts, which are bone-resorbing cells, to break down bone tissue.
- This process, known as osteoporosis, releases stored calcium from the bones into the bloodstream to raise calcium levels.
- Action in the Kidneys:
- PTH reduces calcium excretion by increasing calcium reabsorption in the kidneys during filtration.
- It also activates Vitamin D in the kidneys, which is crucial for calcium absorption in the intestines.
- Role of Activated Vitamin D:
- Activated Vitamin D enhances calcium reabsorption in the distal tubules of the nephrons.
- This process is facilitated by a vitamin D-dependent calcium-binding protein, which increases the efficiency of calcium uptake.
- Overall Impact:
- PTH ensures that calcium is mobilized from bones, conserved in the kidneys, and absorbed in the intestines to maintain optimal blood calcium levels.
Diseases and Disorders of Parathyroid Gland
Diseases and disorders of the parathyroid gland can lead to significant disturbances in calcium and phosphate balance, affecting various systems of the body. Below is a detailed exploration of key parathyroid disorders:
- Primary Hyperparathyroidism:
- This disorder affects about 2% of the population over the age of 55, with women being more prone than men.
- It typically results from a parathyroid adenoma or hyperplasia and leads to excessive secretion of parathyroid hormone (PTH), causing hypercalcemia (elevated blood calcium levels).
- Patients may experience weakness, bone pain, mental fog, anxiety, or depression. Advanced cases can result in kidney stones, severe bone disease, and cardiovascular issues.
- Diagnosis is commonly made through routine blood tests showing elevated calcium levels and high or normal PTH without an appropriate stimulus.
- Secondary Hyperparathyroidism:
- In this condition, the parathyroid glands produce excessive PTH in response to chronically low calcium levels.
- It is often associated with vitamin D deficiency, renal insufficiency, or malabsorption of calcium in the gastrointestinal tract.
- Blood tests typically show elevated PTH with low or normal calcium levels.
- Symptoms include bone pain, kidney stones, and digestive problems, though the underlying cause often drives most symptoms.
- If left untreated, secondary hyperparathyroidism can progress to tertiary hyperparathyroidism, where the glands become autonomously hyperactive, leading to hypercalcemia.
- Hypoparathyroidism:
- Hypoparathyroidism results from insufficient PTH secretion, leading to low blood calcium (hypocalcemia) and high phosphate levels (hyperphosphatemia).
- Common causes include neck surgery, radiation, genetic mutations, or autoimmune disorders.
- Mild cases may cause tingling in the extremities, brittle nails, or dry skin. Severe cases can lead to muscle cramps (tetany), seizures, and cardiac issues.
- Untreated chronic hypoparathyroidism may result in skeletal deformities, cataracts, or long-term cardiovascular complications.
- Pseudohypoparathyroidism:
- Pseudohypoparathyroidism occurs due to resistance to PTH despite its normal or elevated production, often caused by genetic mutations affecting the PTH signaling pathway.
- This leads to low calcium and high phosphate levels similar to hypoparathyroidism, but PTH levels remain elevated.
- Associated symptoms include those of hypocalcemia, as well as features of Albright hereditary osteodystrophy, such as short stature, round face, and intellectual disabilities.
- Parathyroid Carcinoma:
- Parathyroid carcinoma is a rare malignancy that causes severe primary hyperparathyroidism.
- It often presents with very high PTH and calcium levels, leading to bone pain, fractures, kidney stones, and gastrointestinal issues such as pancreatitis or ulcers.
- Definitive diagnosis requires surgical resection followed by histological examination, as fine-needle aspiration is not recommended.
- Though rare, this form of cancer can be fatal, primarily due to complications related to hypercalcemia rather than the malignancy itself.
Functions of Parathyroid Gland
Below is a detailed explanation of the key functions of the parathyroid gland:
- Regulation of Calcium Homeostasis:
- The parathyroid glands synthesize and release parathyroid hormone (PTH), which is the primary regulator of calcium balance in the body.
- PTH helps maintain stable calcium levels by responding to changes in blood calcium concentrations.
- Action on Bones:
- PTH inhibits the activity of osteoblasts (cells responsible for bone formation) and stimulates osteoclasts (cells that break down bone tissue).
- This process releases stored calcium from the bones into the bloodstream, increasing blood calcium levels.
- Effect on Kidneys:
- PTH acts on the nephrons in the kidneys to enhance calcium reabsorption.
- It regulates calcium transporters, ensuring that calcium is retained during filtration and preventing excessive calcium loss through urine.
- Indirect Effect on the Gastrointestinal Tract:
- While the parathyroid glands do not directly act on the gastrointestinal tract, PTH stimulates the synthesis of active vitamin D in the kidneys.
- Activated vitamin D increases the absorption of calcium and phosphate from the gut, further contributing to maintaining calcium balance.
- Phosphate Regulation:
- In addition to regulating calcium, PTH also influences phosphate levels by reducing its reabsorption in the kidneys, leading to increased phosphate excretion through urine.
- Brown MB, Limaiem F. Histology, Parathyroid Gland. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK546596/
- Lofrese JJ, Basit H, Lappin SL. Physiology, Parathyroid. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482510/
- https://www.onlinebiologynotes.com/what-is-parathyroid-gland/
- https://teachmeanatomy.info/neck/viscera/parathyroid-glands/
- https://en.wikipedia.org/wiki/Parathyroid_gland