What is Pancreas?
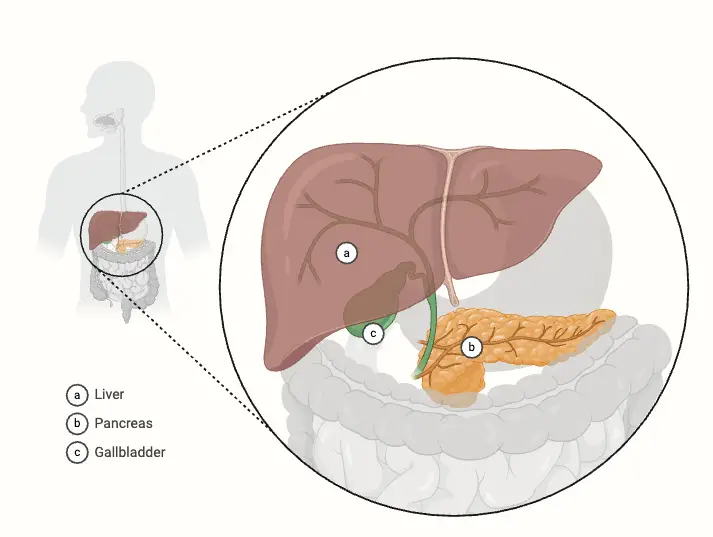
- The pancreas is a vital organ within the digestive and endocrine systems of vertebrates, particularly in humans. It is situated in the abdominal cavity, posterior to the stomach, and serves a dual function as a gland. The pancreas is categorized as a mixed gland, known as a heterocrine gland, due to its ability to perform both endocrine and exocrine functions. Approximately 99% of the pancreas is devoted to exocrine activities, while a mere 1% serves endocrine purposes.
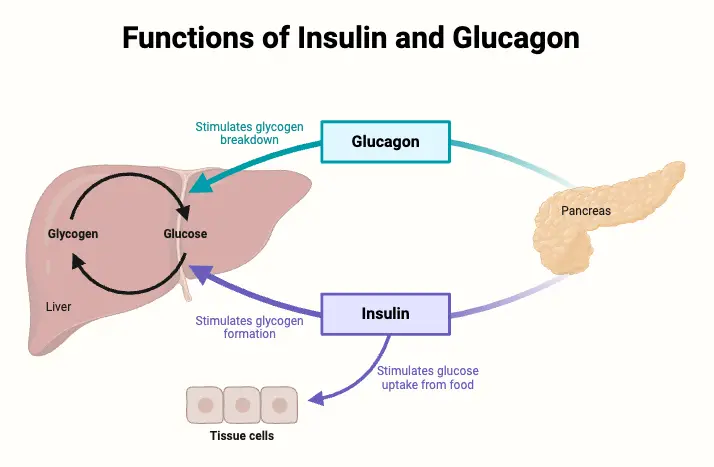
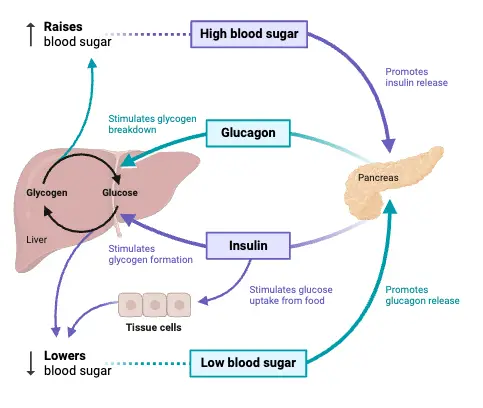
- As an endocrine gland, the pancreas plays a crucial role in regulating blood glucose levels through the secretion of various hormones. Key hormones produced include insulin, glucagon, somatostatin, and pancreatic polypeptide. Insulin and glucagon, secreted by specialized clusters of cells known as the Islets of Langerhans, work in concert to maintain glucose homeostasis. Insulin lowers blood sugar levels, while glucagon raises them, thereby ensuring the body has adequate energy to function.
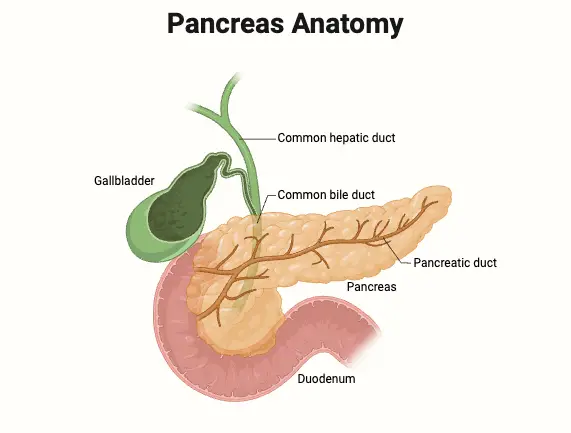
- In its capacity as an exocrine gland, the pancreas produces pancreatic juice, which is released into the duodenum via the pancreatic duct. This digestive fluid contains bicarbonate ions, which neutralize the acidic chyme arriving from the stomach, and various digestive enzymes that facilitate the breakdown of carbohydrates, proteins, and fats. These enzymes are essential for the proper digestion of nutrients, highlighting the pancreas’s role in the digestive process.
- Pancreatitis, the inflammation of the pancreas, is a significant health concern, often resulting from chronic alcohol consumption or gallstones. This condition can severely impact the pancreas’s ability to function effectively. Furthermore, the organ’s involvement in blood sugar regulation makes it a key player in diabetes mellitus, a metabolic disorder characterized by chronic high blood sugar levels. Pancreatic cancer, often emerging as a consequence of chronic pancreatitis or other risk factors, poses a grave prognosis, as it frequently remains undetected until it has metastasized to other organs.
- The term “pancreas” is derived from the Greek words πᾶν (pân, meaning “all”) and κρέας (kréas, meaning “flesh”). The significance of the pancreas in relation to diabetes was first recognized in 1889, with the discovery of its role in insulin production following in 1921.
- The pancreas’s endocrine component is primarily composed of the Islets of Langerhans, which consist of several thousand endocrine cells. This region accounts for roughly 2% of the total pancreatic mass but is critical in regulating metabolic processes through hormone secretion. The islets contain various cell types, each producing different hormones necessary for metabolic function. Notably, the formation of the endocrine region begins around ten weeks of gestation, stemming from the multiplication and differentiation of a single immature epithelial duct.
- The morphology and cellular characteristics of the Islets of Langerhans can vary significantly between species, influencing their size and cellular composition. This diversity reflects the adaptability of the pancreas across different vertebrate species, yet its fundamental functions in digestion and hormonal regulation remain consistent.
Definition of Pancreas
The pancreas is a vital organ in the human body that serves dual functions: it acts as an endocrine gland by producing hormones such as insulin and glucagon to regulate blood sugar levels, and as an exocrine gland by secreting digestive enzymes and bicarbonate into the small intestine to aid in the digestion of food.
Anatomical Position of Pancreas
The pancreas is an elongated organ situated within the upper abdomen, specifically at the level of the transpyloric plane (approximately the first lumbar vertebra, L1). Except for its tail, the pancreas is classified as a retroperitoneal organ, meaning it is located behind the peritoneum, the lining of the abdominal cavity. Its anatomical positioning allows it to have significant relations with various surrounding structures.
- General Positioning:
- The pancreas is located deep within the abdominal cavity, predominantly in the epigastric and left hypochondriac regions.
- Its head is nestled within the curve of the “C” shaped duodenum, while its tail extends toward the spleen.
- Relations with Other Organs:
- Stomach: The pancreas is positioned posterior to the stomach, with the lesser sac separating the two. The pylorus of the stomach lies anterior to the pancreas.
- Duodenum: The first part of the duodenum is situated anterior to the head of the pancreas, while the second part, including the ampulla of Vater, lies laterally to the right of the pancreatic head.
- Transverse Mesocolon: This structure attaches to the anterior surface of the pancreas, providing additional support.
- Common Bile Duct: The common bile duct descends posteriorly to the head of the pancreas before opening into the second part of the duodenum. It shares a conduit with the major pancreatic duct, converging at the major duodenal papilla.
- Spleen: The spleen is located posteriorly and laterally to the pancreas, with the lienorenal ligament—formed from peritoneum—connecting it to the tail of the pancreas.
- Vascular Relationships:
- Aorta and Inferior Vena Cava: These major blood vessels run posterior to the head of the pancreas, playing a crucial role in supplying blood to the region.
- Superior Mesenteric Artery: This artery passes behind the neck of the pancreas and anterior to the uncinate process, providing essential blood flow to the intestines.
- Hepatic Portal Vein: Formed by the union of the splenic and superior mesenteric veins, this vein is located posterior to the neck of the pancreas, highlighting its importance in venous drainage.
- Splenic Artery: This artery travels along the superior border of the pancreas, extending from its origin at the celiac plexus to the splenic hilum.
Structure of Pancreas
The pancreas is a complex organ characterized by distinct structural components that facilitate its dual functions in both endocrine and exocrine systems. It is typically divided into five main anatomical parts, each playing a specific role in the overall function of the organ.
- Head: The head of the pancreas is its widest portion, situated within the C-shaped curve of the duodenum. This part is connected to the duodenum by connective tissue, allowing for the direct release of pancreatic juices into the digestive tract.
- Uncinate Process: This projection arises from the lower part of the head and extends medially, lying beneath the body of the pancreas. The uncinate process is located posterior to the superior mesenteric vessels, which are critical for the vascular supply of the pancreas and surrounding structures.
- Neck: Positioned between the head and body, the neck of the pancreas overlies the superior mesenteric vessels, forming a groove in its posterior aspect. This anatomical feature is essential for understanding the vascular relationships within the abdominal cavity.
- Body: The body of the pancreas is centrally located, traversing the midline of the body. It is situated behind the stomach and to the left of the superior mesenteric vessels, further emphasizing the organ’s anatomical complexity and integration with neighboring structures.
- Tail: The tail represents the leftmost portion of the pancreas and lies in close proximity to the hilum of the spleen. This section is contained within the splenorenal ligament along with the splenic vessels. Notably, the tail is the only intraperitoneal portion of the pancreas, distinguishing it from the other parts.
In addition to these structural components, the pancreas contains the Islets of Langerhans, which constitute about 2% of the total pancreatic mass. The total number of islets in humans ranges from approximately 3.2 to 14.8 million. The islets are composed of four distinct cell types:
- α cells: These cells are responsible for producing glucagon, a hormone that raises blood glucose levels.
- β cells: Account for about 60% of the total islet mass, these cells produce insulin, which lowers blood glucose levels.
- δ cells: Comprising approximately 10% of the islet mass, δ cells secrete somatostatin, which regulates the endocrine system and inhibits the secretion of other hormones.
- γ or PP cells: These pancreatic polypeptide-producing cells also make up about 10% of the mass and are involved in regulating pancreatic secretions and appetite.
The cellular arrangement of the islets is generally random, with most following a mantle-core pattern, indicating a complex architecture that allows for effective hormone secretion. The blood and nerve supply to the pancreas is facilitated by a neuromuscular bundle that penetrates the central core of the β cells, ensuring the organ is well vascularized and innervated.
Duct System of Pancreas
The duct system of the pancreas plays a crucial role in the exocrine functions of the organ, facilitating the transport of digestive enzymes and bicarbonate to the small intestine. This system is meticulously organized, allowing for efficient secretion and regulation of pancreatic juices essential for digestion.
- Exocrine Structure: The exocrine pancreas is a lobulated, serous gland composed of approximately one million acini, which are clusters of specialized cells that produce digestive enzyme precursors. These acini are structurally analogous to small berries, emphasizing their clustered arrangement.
- Intercalated Ducts: Each acinus is connected to short intercalated ducts. These ducts serve as conduits for the digestive enzyme precursors produced by the acinar cells.
- Intralobular Collecting Ducts: The intercalated ducts merge with those from adjacent lobules, forming a network of intralobular collecting ducts. This network is integral for channeling secretions toward the main pancreatic duct.
- Main Pancreatic Duct: The main pancreatic duct runs the entire length of the pancreas. It serves as the principal duct through which pancreatic juices flow. At its distal end, the main pancreatic duct unites with the common bile duct, a significant structure that collects bile from the liver and gallbladder.
- Hepatopancreatic Ampulla of Vater: The junction of the main pancreatic duct and the common bile duct forms the hepatopancreatic ampulla of Vater. This ampulla is a critical anatomical feature that allows for the convergence of bile and pancreatic juices before entering the duodenum.
- Major Duodenal Papilla: The ampulla of Vater opens into the duodenum through the major duodenal papilla. This opening is essential for the release of digestive enzymes and bicarbonate into the intestinal lumen, aiding in the neutralization of gastric acid and the digestion of nutrients.
- Sphincter of Oddi: The release of secretions from the pancreas into the duodenum is regulated by the sphincter of Oddi. This muscular valve encircles the ampulla of Vater, functioning as a control mechanism that ensures the coordinated release of pancreatic juice and bile, thereby optimizing digestive processes.
Vasculature of Pancreas
The vasculature of the pancreas is vital for its function, ensuring adequate blood supply for both its exocrine and endocrine activities. The intricate network of arteries and veins facilitates the delivery of oxygen, nutrients, and hormones while allowing for efficient drainage of metabolic waste products.
- Arterial Supply: The pancreas receives its arterial blood supply predominantly from the pancreatic branches of the splenic artery. This artery is responsible for nourishing the majority of the gland.
- Additional Arterial Contributions: The head of the pancreas has supplementary blood supply from two critical arteries:
- The superior pancreaticoduodenal artery, which branches from the gastroduodenal artery (originating from the celiac trunk).
- The inferior pancreaticoduodenal artery, arising from the superior mesenteric artery. This dual supply is essential for maintaining blood flow to the head region, particularly during periods of high metabolic demand.
- Venous Drainage: The venous drainage system is equally important in maintaining pancreatic health. The head of the pancreas drains into the superior mesenteric branches of the hepatic portal vein. This connection is significant as it directs blood towards the liver for further processing.
- Drainage of the Rest of the Pancreas: The remaining portions of the pancreas are drained by pancreatic veins that lead to the splenic vein. This venous return is crucial for ensuring that the metabolic byproducts are efficiently removed from the pancreas.
- Portal Circulation: The pancreas is intricately linked to the portal circulation, which is vital for regulating nutrient absorption and metabolism. By draining into the hepatic portal vein, the pancreas ensures that its secretions, including hormones like insulin and glucagon, are effectively transported to the liver for regulation of blood glucose levels.
- Vascular Relationships: The proximity of major vascular structures, such as the splenic artery and vein, to the pancreas plays a critical role in surgical considerations and the management of pancreatic diseases. Understanding these relationships is essential for healthcare professionals when addressing conditions such as pancreatitis or pancreatic cancer.
Hormones of Pancreas
The pancreas plays a crucial role in regulating metabolic processes through the secretion of hormones from its specialized cell clusters known as the Islets of Langerhans. These hormones—insulin, glucagon, somatostatin, and pancreatic polypeptide—work together to maintain homeostasis within the body.
- Insulin
- Secreted by the β cells of the Islets of Langerhans, insulin is a polypeptide hormone composed of approximately 50 amino acids.
- Its primary function is to lower blood nutrient levels, particularly glucose, and to a lesser extent, amino acids and fatty acids.
- Insulin is categorized as an anabolic hormone, promoting the storage of nutrients in various tissues.
- It is synthesized as part of a larger precursor molecule known as proinsulin, which undergoes enzymatic cleavage to produce active insulin.
- Insulin operates through several mechanisms:
- It enhances the transport of glucose into cells, thereby lowering blood glucose levels.
- It inhibits the breakdown of glycogen into glucose, reducing the availability of glucose in the bloodstream.
- Additionally, insulin prevents the conversion of amino acids and fats into glucose, further contributing to the regulation of blood sugar levels.
- Glucagon
- Produced by the α cells of the pancreas, glucagon is a polypeptide hormone consisting of 29 amino acids.
- In contrast to insulin, glucagon serves as a hyperglycemic agent, primarily responsible for raising blood glucose levels.
- The primary target organ for glucagon is the liver, where it stimulates the breakdown of glycogen into glucose through a process called glycogenolysis.
- It also promotes gluconeogenesis, the synthesis of glucose from non-carbohydrate precursors such as lactic acid and certain amino acids.
- The secretion of glucagon is triggered by decreased blood glucose levels, which is often mediated by the sympathetic nervous system. Conversely, elevated amino acid levels also stimulate glucagon release, demonstrating its role in metabolic regulation.
- Somatostatin
- Somatostatin is secreted by the δ cells of the Islets of Langerhans.
- This hormone acts primarily as an inhibitory regulator of endocrine and exocrine functions.
- It reduces the secretion of both insulin and glucagon, contributing to the regulation of glucose metabolism and maintaining balanced nutrient levels.
- Furthermore, somatostatin plays a role in inhibiting gastrointestinal motility and the release of various digestive enzymes.
- Pancreatic Polypeptide
- Produced by the PP cells (or γ cells), pancreatic polypeptide plays a role in regulating pancreatic secretions and gastrointestinal motility.
- Its release is influenced by meals and is involved in the feedback mechanism that balances digestive enzyme secretion.
Disorders of Pancreas
Disorders of the pancreas encompass a range of conditions that can significantly impact metabolic processes and overall health. Understanding these disorders is essential for effective diagnosis and treatment.
- Diabetes Mellitus
- Diabetes mellitus is primarily characterized by either insufficient insulin secretion or ineffective insulin action.
- It is classified into two main types:
- Type 1 Diabetes Mellitus:
- This autoimmune disorder occurs when the immune system mistakenly attacks and destroys the insulin-secreting β cells in the pancreas, leading to an absolute deficiency of insulin.
- It typically develops during childhood or adolescence and is marked by an immediate onset of symptoms.
- Patients with Type 1 diabetes require lifelong insulin injections to regulate blood glucose levels.
- Type 2 Diabetes Mellitus:
- This form is more prevalent, particularly among adults, and arises from a combination of insulin resistance and inadequate insulin secretion.
- Symptoms often develop gradually and may go unnoticed for years.
- Management usually involves lifestyle modifications, such as diet and exercise, alongside pharmacological interventions like metformin or other antidiabetic medications.
- Type 1 Diabetes Mellitus:
- Both types of diabetes can lead to chronic complications, including kidney failure, cardiovascular diseases, and neuropathy if not adequately managed.
- Pancreatic Perforation
- This serious condition occurs when the pancreatic tissue is damaged, allowing digestive enzymes such as amylase and lipase to leak into the abdominal cavity, leading to a process called self-digestion.
- Surgical removal of the pancreas may be necessary; however, individuals will require lifelong management, including insulin therapy and pancreatic enzyme replacements to aid digestion.
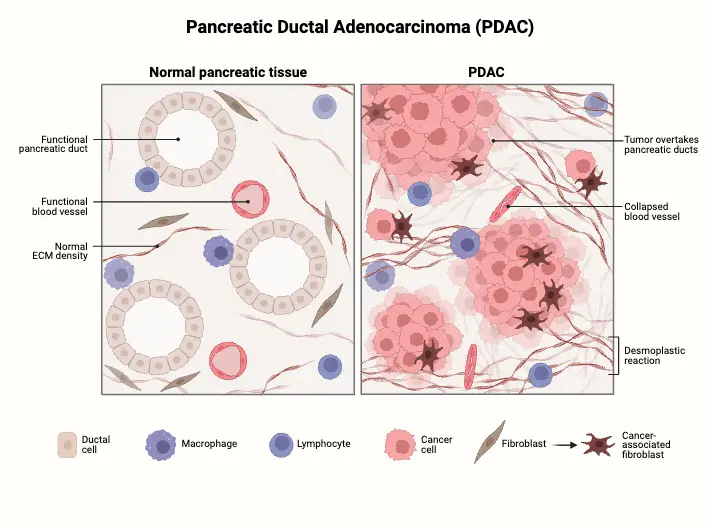
- Pancreatic Cancer
- Among the various types of cancer, pancreatic adenocarcinoma is particularly notorious for its poor prognosis and difficulty in treatment.
- Typically diagnosed at an advanced stage due to a lack of early symptoms, it has a median age of diagnosis of 71 years.
- Risk factors for developing pancreatic cancer include smoking, obesity, diabetes, and genetic predispositions such as multiple endocrine neoplasia type 1 and hereditary nonpolyposis colon cancer.
- Pancreatitis
- Inflammation of the pancreas is referred to as pancreatitis, which can be acute or chronic.
- Causes of pancreatitis include:
- Recurrent gallstones
- Alcohol abuse
- Viral infections, such as measles and mumps
- Certain medications and genetic conditions like alpha-1 antitrypsin deficiency
- Rarely, exposure to scorpion stings.
- Symptoms often include severe abdominal pain that can radiate to the back, jaundice, pale stools, and dark urine.
- Management typically involves hospitalization, supportive care, and addressing the underlying cause, whether it be dietary changes or treatment for gallstones.
Functions of Pancreas
The pancreas plays a crucial role in regulating various physiological processes in the body, primarily through its dual functions: endocrine and exocrine. These functions are vital for maintaining metabolic homeostasis and digestive processes.
- Endocrine Functions
- The pancreas houses clusters of cells known as the Islets of Langerhans, which are responsible for the endocrine functions of the organ. This component of the pancreas is critical for regulating blood nutrient levels through hormone secretion.
- Insulin:
- Produced by the β cells within the Islets of Langerhans, insulin is a polypeptide hormone composed of approximately 50 amino acids.
- Its primary function is to lower blood glucose levels. It achieves this by facilitating the uptake of glucose into various tissues, particularly muscle and adipose tissue, while inhibiting hepatic gluconeogenesis and glycogenolysis.
- Insulin also promotes the storage of nutrients, thus exhibiting anabolic effects on metabolism.
- Glucagon:
- Secreted by the α cells of the pancreas, glucagon functions antagonistically to insulin.
- This hormone increases blood glucose levels, particularly during fasting or low-carbohydrate intake. It stimulates the liver to convert stored glycogen back into glucose (glycogenolysis) and promotes gluconeogenesis from non-carbohydrate sources, such as amino acids and glycerol.
- The secretion of glucagon is typically triggered by declining blood glucose levels and rising levels of certain amino acids.
- Somatostatin:
- Released by the δ cells of the Islets of Langerhans, somatostatin functions to inhibit the secretion of both insulin and glucagon.
- It also plays a regulatory role by inhibiting growth hormone release from the pituitary gland. This multifaceted regulation ensures that hormone levels are kept in balance according to the body’s metabolic needs.
- Exocrine Functions
- The pancreas also possesses an exocrine component responsible for producing digestive enzymes, though this aspect is not highlighted in the provided content.
- These enzymes include amylase, lipase, and proteases, which are essential for the digestion of carbohydrates, fats, and proteins, respectively. They are secreted into the small intestine to facilitate nutrient absorption.
- Talathi SS, Zimmerman R, Young M. Anatomy, Abdomen and Pelvis, Pancreas. [Updated 2023 Apr 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532912/
- Karpińska M, Czauderna M. Pancreas-Its Functions, Disorders, and Physiological Impact on the Mammals’ Organism. Front Physiol. 2022 Mar 30;13:807632. doi: 10.3389/fphys.2022.807632. PMID: 35431983; PMCID: PMC9005876.
- https://en.wikipedia.org/wiki/Pancreas
- https://columbiasurgery.org/pancreas/pancreas-and-its-functions
- https://www.kenhub.com/en/library/anatomy/the-pancreas
- https://pancreapedia.org/reviews/anatomy-and-histology-of-pancreas
- https://www.brainkart.com/article/The-Pancreas—Structure-and-Function-of-Digestive-System_21145/
- https://teachmeanatomy.info/abdomen/viscera/pancreas/
- https://www.geeksforgeeks.org/pancreas-diagram-structure/
- https://www.onlinebiologynotes.com/pancreas-mixed-gland/