What is Ovary?
- The ovary is a critical component of the female reproductive system, serving both reproductive and endocrine functions. Structurally, each ovary is made up of two main regions: the outer cortex and the inner medulla. The cortex contains numerous ovarian follicles, each of which houses an immature egg, or oocyte. These follicles undergo a maturation process called folliculogenesis, which leads to the release of an egg during ovulation.
- The ovary plays a central role in hormone production, functioning as an endocrine gland. It produces essential hormones such as estrogen, progesterone, and androgens. Estrogen, synthesized primarily in the ovarian follicles, is essential for the development of female secondary sexual characteristics and prepares the uterus for pregnancy. Progesterone, mainly produced by the corpus luteum after ovulation, helps maintain the uterine lining, supporting potential implantation and pregnancy. Androgens, including testosterone, although present in smaller quantities in females, also contribute to reproductive processes.
- In terms of reproductive function, when an ovum is released during ovulation, it travels through the fallopian tube toward the uterus, where it may be fertilized. Each female has two ovaries, located on either side of the uterus, and they operate in a cycle from puberty until menopause, continuously maturing and releasing eggs.
- The ovary’s function evolves through different life stages, starting from the prenatal period and continuing until menopause, when the ovary ceases to release eggs and hormone production declines. Through its roles in ovulation and hormone regulation, the ovary is fundamental to both the menstrual cycle and overall fertility.
Definition of Ovary
The ovary is a reproductive organ in females that produces eggs and secretes hormones like estrogen and progesterone, essential for regulating the menstrual cycle and fertility.
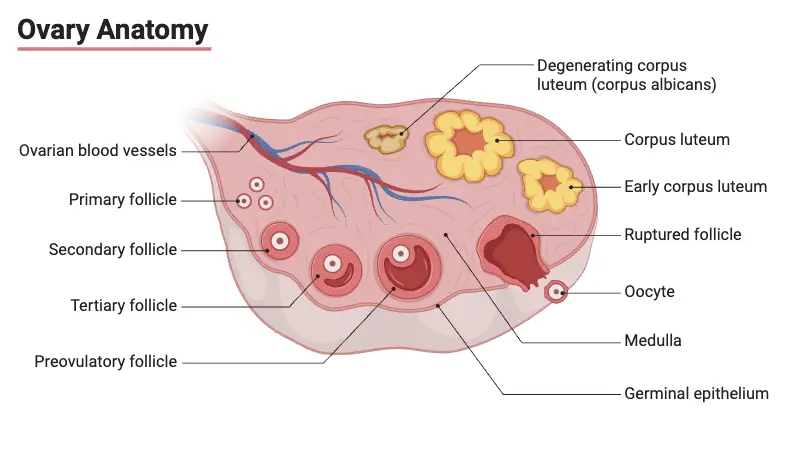
Anatomy of the Ovary
The ovary is a crucial organ in the female reproductive system, responsible for producing eggs and secreting hormones essential for fertility and reproductive health. It is located in the pelvic region near the uterus, with a complex internal and external structure. The anatomy of the ovary is detailed as follows:
- Location and Size:
The ovaries are paired, with one on each side of the uterus. They are small, ovoid-shaped glands, typically measuring 3 to 5 cm in length and weighing 10–20 grams during reproductive years. As a woman ages, their size and weight decrease. Each ovary is connected to the uterus by the ovarian ligament and supported by the broad ligament via the mesovarium. - Germinal Epithelium:
The outermost layer of the ovary is lined with germinal epithelium, which consists of a single layer of cuboidal cells. This layer is continuous with the peritoneal lining. Despite its name, the germinal epithelium does not produce germ cells but plays a role in protecting the ovary. The cells in this layer contain microvilli and mitochondria, which increase in size during pregnancy. - Cortex:
The cortex is the thick outer part of the ovary, composed of various tissues:- Tunica Albuginea: This is a thin, fibrous layer beneath the germinal epithelium. It is much less dense than the tunica albuginea found in the testes.
- Stroma: Below the tunica albuginea, the stroma is a connective tissue matrix made of reticular fibers and fusiform cells that resemble mesenchymal cells. These cells provide structural support and contain developing ovarian follicles.
- Ovarian Follicles: Scattered throughout the stroma, these follicles are in different stages of development, each containing an immature egg or oocyte. The maturation of these follicles leads to the release of eggs during ovulation.
- Medulla:
The medulla forms the inner part of the ovary and contains connective tissue rich in blood vessels, especially veins. Smooth muscle fibers and elastic fibers are also found in this region, playing a role in the vascular supply and the overall function of the ovary. - Hilum:
The hilum is the point where the ovary attaches to the mesentery, allowing for the entry and exit of blood vessels and lymphatic vessels. It serves as a critical passage for the vascular and nervous supply to the ovary. The hilum also contains remnants of mesonephric ducts and hilus cells, which are similar to interstitial cells found in the testes.
Hormones of Ovary
The ovaries produce several key hormones that play crucial roles in regulating female reproductive health and secondary sexual characteristics. These hormones are vital for processes such as menstruation, pregnancy, and lactation. The primary hormones secreted by the ovaries are outlined below:
- Estrogen:
Estrogen is a primary female sex hormone responsible for various reproductive functions and the development of secondary sexual characteristics. The ovaries produce large quantities of estrogen, though some amount is also produced by the adrenal glands. Estrogen facilitates the proliferation and growth of cells in the reproductive system, regulating the menstrual cycle and preparing the body for pregnancy. The three main types of estrogen secreted by the ovaries are:- β-Estradiol: The most potent and abundant form of estrogen produced by the ovaries, β-estradiol plays a central role in reproductive health, influencing the menstrual cycle, ovulation, and the development of the uterine lining.
- Estrone: This weaker form of estrogen is also secreted by the ovaries, contributing to the regulation of reproductive functions, though its levels are lower compared to β-estradiol.
- Estriol: Primarily produced during pregnancy, estriol is the least potent of the three estrogens and plays a supportive role in maintaining pregnancy.
- Progesterone:
Progesterone is the dominant hormone in the second half of the menstrual cycle and is critical for preparing the uterus for pregnancy. Its primary function is to support the thickening of the uterine lining (endometrium), making it suitable for embryo implantation. Progesterone also prepares the mammary glands for lactation. Key details about progesterone include:- In non-pregnant women, progesterone is mainly secreted during the luteal phase of the ovarian cycle by the corpus luteum, which forms after ovulation from the remnants of the ovarian follicle.
- During pregnancy, especially after the fourth month, progesterone production increases significantly, with the placenta contributing to its secretion, helping maintain the pregnancy and prevent uterine contractions.
Regulation of Ovarian Function
The ovaries are essential for female fertility, and their function is regulated by a network of hormonal signals. This regulation is controlled by the hypothalamic-pituitary-gonadal (HPG) axis and is influenced by various factors such as age, lifestyle, and environmental conditions. The process of ovarian regulation is detailed below:
- Hormonal Regulation and Control:
Ovarian function is controlled by a series of hormonal interactions initiated by the HPG axis, ensuring proper follicular development, ovulation, and hormone production.- Hypothalamic-Pituitary-Gonadal Axis:
The HPG axis begins with the hypothalamus, which secretes gonadotropin-releasing hormone (GnRH). This hormone stimulates the anterior pituitary gland to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH promotes the growth and development of ovarian follicles, while LH triggers ovulation and the formation of the corpus luteum, which produces progesterone. - FSH and Follicular Development:
FSH is critical for the early stages of follicle development. It stimulates the growth of multiple ovarian follicles, but typically, only one will reach full maturity and be released during ovulation. FSH also promotes the production of estrogen by the follicles. - LH and Ovulation:
Midway through the menstrual cycle, a surge in LH leads to ovulation, where the mature egg is released from the ovary. After ovulation, LH supports the development of the corpus luteum, which is responsible for secreting progesterone to maintain the uterine lining in preparation for a potential pregnancy.
- Hypothalamic-Pituitary-Gonadal Axis:
- Feedback Mechanisms:
Hormonal regulation in the ovaries is tightly controlled by feedback loops to maintain balance and proper function.- Negative Feedback:
As estrogen levels rise during follicular development, they inhibit the release of FSH from the pituitary, preventing overstimulation of the ovaries. Similarly, after ovulation, elevated levels of progesterone suppress LH production. These feedback mechanisms ensure that hormone levels remain within optimal ranges to support the menstrual cycle. - Positive Feedback (LH Surge):
Toward the middle of the menstrual cycle, high levels of estrogen from the mature follicle create a positive feedback loop, causing a surge in LH. This LH surge is the key event that triggers ovulation.
- Negative Feedback:
Factors Influencing Ovarian Function
Ovarian function is influenced by various internal and external factors that impact fertility and hormonal balance. These factors include age, environmental conditions, and lifestyle habits. A detailed breakdown of these influences is provided below:
- Age:
Ovarian function is highly dependent on age. As women age, the ovarian reserve—the number of viable eggs—gradually declines. This decrease in follicle quantity and quality reduces the ovaries’ ability to produce hormones like estrogen and progesterone. As a result, fertility diminishes, and menopause typically occurs when ovarian function ceases entirely. - Environmental Factors:
The environment plays a significant role in ovarian health. Exposure to pollutants, toxins, and chemicals, such as endocrine-disrupting chemicals (EDCs), can adversely affect ovarian function. EDCs interfere with the body’s hormone production and signaling, leading to disruptions in the menstrual cycle and potential fertility issues. Long-term exposure to harmful environmental agents can reduce ovarian efficiency and overall reproductive health. - Lifestyle Factors:
Lifestyle choices, including diet, physical activity, and stress management, significantly influence ovarian function. Poor dietary habits, such as consuming processed foods and lacking essential nutrients, can negatively affect hormone regulation. Similarly, a sedentary lifestyle can disrupt normal hormonal cycles. Chronic stress increases cortisol levels, which can suppress the hypothalamic-pituitary-gonadal axis, leading to irregular menstruation and decreased ovarian performance. On the other hand, a balanced diet, regular physical exercise, and effective stress management promote healthy ovarian function and reproductive well-being.
Ovarian Disorders
Ovarian disorders refer to various medical conditions that affect the ovaries and can disrupt normal reproductive function. These disorders often lead to hormonal imbalances, fertility issues, and other health complications. A detailed overview of common ovarian disorders is provided below:
- Polycystic Ovary Syndrome (PCOS):
PCOS is a prevalent hormonal disorder characterized by irregular menstrual cycles, elevated androgen (male hormone) levels, and the presence of multiple small cysts on the ovaries. Women with PCOS often experience symptoms such as irregular periods, acne, excessive hair growth (hirsutism), weight gain, and difficulty in conceiving. PCOS can also increase the risk of long-term complications such as type 2 diabetes and cardiovascular disease. - Ovarian Cysts:
Ovarian cysts are fluid-filled sacs that develop on or within the ovary. Most ovarian cysts are benign and asymptomatic, often resolving without medical intervention. However, some cysts can cause discomfort, pain, or bloating, and in rare cases, they may rupture or twist (ovarian torsion), leading to more severe symptoms that require medical attention. Types of ovarian cysts include functional cysts, dermoid cysts, and endometriomas. - Ovarian Cancer:
Ovarian cancer is a malignant condition that originates in the cells of the ovaries. It is often referred to as a “silent killer” because it is usually asymptomatic in the early stages, making it difficult to detect until it has advanced. Symptoms may include abdominal bloating, pelvic pain, and unexplained weight loss. Early diagnosis and treatment improve survival rates, but ovarian cancer remains one of the most challenging cancers to treat effectively. - Premature Ovarian Failure (POF):
Premature ovarian failure, also called primary ovarian insufficiency, occurs when the ovaries stop functioning before the age of 40. This condition results in reduced or absent estrogen production, leading to infertility and symptoms commonly associated with menopause, such as hot flashes, night sweats, and vaginal dryness. POF can be caused by genetic factors, autoimmune diseases, or medical treatments such as chemotherapy.
Functions of Ovary
The ovary is essential for female reproduction, functioning in both egg production and hormone regulation. Understanding the specific functions of the ovary highlights its critical role in reproductive health. The key functions of the ovary are as follows:
- Production of Oocytes (Eggs):
The ovary is responsible for producing oocytes, or eggs, through two primary processes:- Oogenesis: This process involves the development of eggs from precursor cells called oogonia. Oogenesis begins before birth and continues throughout a woman’s reproductive years. The oogonia undergo multiple stages of transformation, eventually maturing into eggs ready for ovulation.
- Folliculogenesis: This is the development and maturation of ovarian follicles, the structures that house immature eggs. Each month, several follicles grow, but typically only one fully matures and releases an egg during ovulation.
- Hormone Production:
The ovary also functions as an endocrine gland, producing hormones critical for reproductive and overall health:- Estrogen: Primarily produced by ovarian follicles, estrogen is essential for developing secondary sexual characteristics and regulating the menstrual cycle. It promotes the growth of the uterine lining, preparing it for potential pregnancy.
- Progesterone: Produced by the corpus luteum after ovulation, progesterone supports the thickened uterine lining during the luteal phase of the menstrual cycle. This hormone is crucial for preparing the uterus for embryo implantation.
- Androgens: The ovary produces small amounts of androgens, including testosterone. These hormones contribute to libido and play a regulatory role in ovarian function.
- Role in the Menstrual Cycle:
The ovary regulates key phases of the menstrual cycle, which is vital for reproductive health and fertility:- Follicular Phase: The cycle begins with the follicular phase, where ovarian follicles develop under the influence of follicle-stimulating hormone (FSH). Estrogen produced by the developing follicles stimulates the thickening of the uterine lining.
- Ovulation: Mid-cycle, a surge in luteinizing hormone (LH) triggers ovulation, releasing a mature egg from the ovary into the fallopian tube. This is the window during which fertilization can occur.
- Luteal Phase: After ovulation, the follicle transforms into the corpus luteum, which secretes progesterone. This hormone maintains the uterine lining, ensuring it remains thick for possible implantation. If fertilization does not occur, the corpus luteum degenerates, hormone levels drop, and menstruation begins, marking the start of a new cycle.
- Gibson E, Mahdy H. Anatomy, Abdomen and Pelvis, Ovary. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545187/
- https://www.pw.live/exams/neet/ovary/
- https://www.brainkart.com/article/Ovaries—Female-Reproductive-System_21990/
- https://www.aakash.ac.in/important-concepts/biology/ovary-structure
- https://www.geeksforgeeks.org/diagram-of-ovary/
- https://www.livescience.com/58862-ovary-facts.html
- https://my.clevelandclinic.org/health/body/22999-ovaries