What is Neuromuscular junction?
- A neuromuscular junction, also known as a myoneural junction, serves as a vital connection between motor neurons and muscle fibers. It facilitates the transmission of signals from the nervous system to the muscle, ultimately leading to muscle contraction.
- The neuromuscular junction plays a crucial role in enabling the nervous system to regulate muscle contraction and control various biological functions. Without this junction, muscles would not receive the necessary innervation to function or maintain muscle tone, which would result in muscle atrophy.
- In the neuromuscular system, nerves from both the central and peripheral nervous systems are interconnected and collaborate with muscles. The process of synaptic transmission at the neuromuscular junction begins when an action potential reaches the presynaptic terminal of a motor neuron. This triggers the activation of voltage-gated calcium channels, allowing calcium ions to enter the neuron. The calcium ions then bind to sensor proteins called synaptotagmins on synaptic vesicles, leading to the fusion of vesicles with the cell membrane and the subsequent release of neurotransmitters, such as acetylcholine (ACh), into the synaptic cleft.
- In vertebrates, motor neurons release ACh, which diffuses across the synaptic cleft and binds to nicotinic acetylcholine receptors (nAChRs) on the muscle fiber’s cell membrane, known as the sarcolemma. These nAChRs function as ionotropic receptors, acting as ligand-gated ion channels. When ACh binds to the receptors, it depolarizes the muscle fiber, triggering a cascade of events that eventually results in muscle contraction.
- Neuromuscular junction diseases can arise from genetic or autoimmune factors. Genetic disorders, like Congenital myasthenic syndrome, can result from mutations in the structural proteins that make up the neuromuscular junction. On the other hand, autoimmune diseases, such as myasthenia gravis, occur when antibodies are produced against nicotinic acetylcholine receptors on the sarcolemma.
- At its core, the neuromuscular junction represents a specific type of synapse where neuronal signals from the brain or spinal cord interact with skeletal muscle fibers, initiating their contraction. The coordinated activation of multiple muscle fibers leads to muscle contraction, enabling movement. Remarkably, the processes occurring at the neuromuscular junction happen at such rapid speeds that movements occur without any noticeable delay. The neuromuscular junction acts as a crucial component in the body’s ability to generate and control movement, bridging the gap between nerve signals and muscle action.
Definition of Neuromuscular junction
A neuromuscular junction is a specialized connection between a motor neuron and a muscle fiber, where signals from the nervous system are transmitted to the muscle, resulting in muscle contraction.
Structure of a Neuromuscular Junction
The structure of Neuromuscular junction can be broadly divided into three parts:
- Presynaptic
- Synaptic cleft
- Postsynaptic portions.
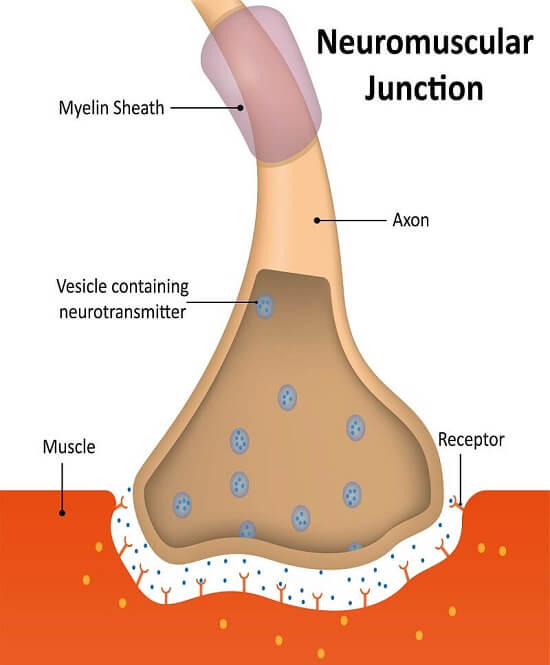
1. Presynaptic Terminal
- The presynaptic terminal, also known as the axonal terminal, is the end of a motor neuron’s axon in a neuromuscular junction. It is responsible for transmitting signals to the muscle fiber.
- Within the presynaptic terminal, there are specialized structures called synaptic vesicles. These vesicles are small compartments separate from the rest of the cell and contain neurotransmitters. In the case of the neuromuscular junction, the neurotransmitter present is acetylcholine (ACh).
- Motor neurons, originating from the anterior horn of the spinal cord or brainstem, innervate skeletal muscles. Their axons, which are the largest diameter axons in the body, lose their myelin sheath as they approach the skeletal muscle fiber. They then divide into fine branches known as terminal axons, which end in small swellings called terminal buttons. These terminal buttons are located at the center of the muscle fiber within the synaptic trough but outside the muscle fiber membrane.
- Each muscle fiber is supplied by a single motor neuron terminal, forming a motor unit. The terminal buttons in the presynaptic terminal contain numerous mitochondria and neurotransmitter vesicles. Acetylcholine (ACh) is synthesized in the mitochondria and stored within these vesicles.
- The synaptic vesicles are clustered around a specific area called the active zone, where voltage-gated calcium (Ca++) channels are present. These channels play a crucial role in facilitating the release of acetylcholine (ACh) during neurotransmission.
2. Synaptic Cleft
- The synaptic cleft, also known as the synaptic gap, plays a crucial role in the transmission of signals between neurons and muscle cells. Situated approximately 20 nanometers wide, it serves as a vital junction between the presynaptic terminal, also known as the axonal terminal, and the postsynaptic membrane, which is the muscle cell that receives the signal.
- The synaptic cleft serves as a crucial checkpoint in the signaling process. It ensures that the concentration of neurotransmitters responsible for transmitting the signal to the muscle cell is tightly regulated. Neurotransmitters are chemical messengers that carry signals across the synapse, the junction between neurons or a neuron and a muscle cell. In this case, the synaptic cleft facilitates the transfer of neurotransmitters from the presynaptic terminal to the postsynaptic membrane.
- The precise structure of the synaptic cleft is important for its function. It is a narrow gap, typically ranging from 50 to 100 nanometers in width. Within this gap, the basement membrane of the muscle fiber contains an enzyme called acetylcholinesterase. This enzyme plays a significant role in the termination of the signal transmission process by breaking down the neurotransmitter acetylcholine (ACh) into acetate and choline.
- Acetylcholine is a neurotransmitter that is essential for transmitting signals from neurons to muscle cells. However, once it has served its purpose, it needs to be rapidly cleared from the synaptic cleft to prevent continuous stimulation of the postsynaptic membrane. Acetylcholinesterase acts as a key player in this process by hydrolyzing acetylcholine into its constituent parts, acetate and choline. This breakdown effectively terminates the signal transmission and allows for the precise control of muscle contractions.
- Overall, the synaptic cleft serves as a crucial interface where the transfer of signals between neurons and muscle cells occurs. Its narrow width and the presence of acetylcholinesterase in the basement membrane of the muscle fiber ensure the precise regulation and termination of signal transmission. Through these mechanisms, the synaptic cleft plays a pivotal role in facilitating efficient communication and coordination within the nervous system.
3. Postsynaptic Membrane
- The postsynaptic membrane is a critical component of the muscle fiber cells that receive signals from motor neurons. This specialized membrane plays a crucial role in the transmission of signals and coordination of muscle contractions. It is characterized by numerous indents and folds that greatly increase its surface area, facilitating efficient signal transmission from the motor neuron.
- One important feature of the postsynaptic membrane is the presence of a specific region known as the end plate membrane or motor end plate. This region of the muscle fiber plasma membrane lies directly beneath the terminal axon portion of the motor neuron. It is at this precise location that the synaptic cleft, the narrow gap between the presynaptic terminal and the postsynaptic membrane, interacts with the muscle fiber.
- To further enhance its surface area, the end plate membrane is thrown into several folds, referred to as junctional folds. These folds are characterized by crests that contain nicotinic acetylcholine (ACh) receptors. Nicotinic ACh receptors are specialized receptors that bind to acetylcholine, a neurotransmitter released by the motor neuron. When acetylcholine binds to these receptors on the crests of the junctional folds, it initiates a series of events that lead to the generation of an electrical signal within the muscle fiber.
- The increased surface area of the postsynaptic membrane, facilitated by the indents and junctional folds, allows for a larger number of nicotinic ACh receptors to be present. This abundance of receptors enables efficient and rapid signal transmission between the motor neuron and the muscle fiber. The binding of acetylcholine to the nicotinic receptors triggers an influx of ions, particularly sodium, into the muscle fiber, leading to the initiation of a muscle contraction.
- In addition to the specialized postsynaptic membrane, muscle cells also possess a unique cell membrane called the sarcolemma. The sarcolemma surrounds the entire muscle fiber and aids in the transmission of signals throughout the fiber. It provides structural support and is responsible for maintaining the electrical potential required for muscle contractions.
Steps of Signalling at Neuromuscular Junctions
Signaling at neuromuscular junctions involves a series of coordinated steps that allow the transmission of signals from the motor neuron to the muscle cell, ultimately leading to muscle contraction. Let’s explore the steps in more detail:
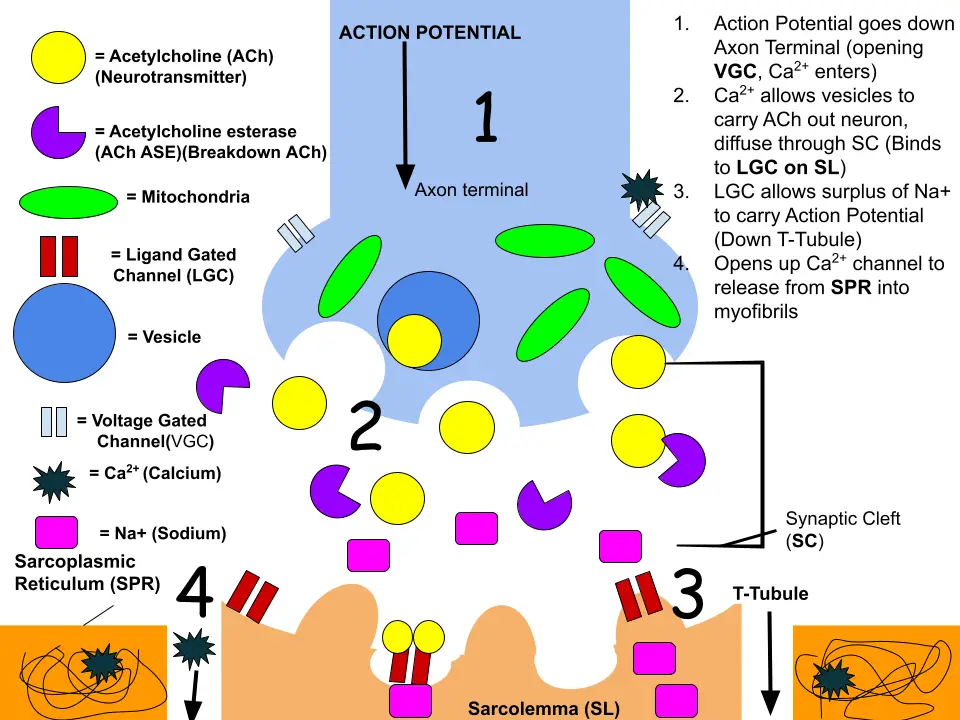
- Motor Neuron Activation: The signal originates from the axon terminal of the previous neuron and travels down the motor neuron to reach the presynaptic axon terminal. This triggers the activation and opening of calcium channels present in the membrane of the axon terminal.
- Vesicle Fusion: Within the axon terminal, neurotransmitters, specifically acetylcholine, are stored in vesicles. When the calcium ions enter the neuron through the opened calcium channels, they bind to SNARE proteins on the surface of the vesicles. This binding triggers vesicle fusion with the cell membrane, allowing the vesicles to release their contents.
- Exocytosis: The fused vesicles release acetylcholine outside the cell through the process of exocytosis. Acetylcholine is then released into the synaptic cleft, the small gap between the presynaptic axon terminal and the postsynaptic membrane.
- Diffusion of Acetylcholine: Acetylcholine diffuses across the synaptic cleft and reaches the postsynaptic membrane, which is located on the muscle cell. The postsynaptic membrane is rich in folds called the sarcolemma, which provide an increased surface area to maximize the number of acetylcholine receptors available for binding.
- Acetylcholine Receptor Binding: Acetylcholine binds to specific receptors on the sarcolemma known as nicotinic acetylcholine receptors. Binding of acetylcholine to these receptors causes ion channels to open, allowing the influx of sodium and potassium ions into the muscle cell.
- Depolarization and Calcium Ion Entry: The influx of sodium ions depolarizes the muscle cell, which facilitates the entry of calcium ions into the cell. The calcium ions play a crucial role in muscle contraction. They interact with the contractile proteins within the muscle cell, leading to the generation of force and contraction.
Additionally, calcium ions present in the sarcoplasmic reticulum, a specialized organelle within the muscle cell, are also released in response to the signaling at the neuromuscular junction. The release of calcium ions from the sarcoplasmic reticulum further contributes to muscle cell contraction.
Furthermore, calcium ions can propagate the signal to contract to other muscle cells by moving between cells through structures called gap junctions. These gap junctions link adjacent muscle cells, allowing them to behave synchronously and coordinate their contractions.
In summary, the steps involved in signaling at neuromuscular junctions include motor neuron activation, vesicle fusion and exocytosis, diffusion of acetylcholine, acetylcholine receptor binding, depolarization and calcium ion entry, release of calcium ions from the sarcoplasmic reticulum, and the potential spread of the signal through gap junctions. These steps ensure the effective transmission of signals from the nervous system to the muscle cells, leading to muscle contraction and coordinated movement.
Disorders of Neuromuscular Junctions
Disorders of neuromuscular junctions encompass a range of conditions that affect the transmission of signals between motor neurons and muscle cells. These disorders can be classified into autoimmune and genetic categories, each with its own unique characteristics and treatment approaches.
- One of the autoimmune disorders that affect the neuromuscular junction is myasthenia gravis (MG). In MG, the body produces antibodies that target either the acetylcholine receptor (AChR) or muscle-specific kinase (MuSK). These antibodies interfere with the binding of acetylcholine to the receptor, leading to muscle weakness and fatigue. Neonatal MG, a transient form of the disease, can occur when maternal AChR antibodies pass through the placenta to the fetus, causing weakness and fetal akinesia.
- Lambert-Eaton myasthenic syndrome (LEMS) is another autoimmune disorder affecting the presynaptic portion of the neuromuscular junction. It is characterized by muscle weakness, autonomic dysfunction, and areflexia. LEMS is caused by autoantibodies that target P/Q-type voltage-gated calcium channels, leading to reduced acetylcholine release from motor nerve terminals. A significant number of LEMS patients also have an associated tumor, typically small-cell lung carcinoma.
- Neuromyotonia, also known as Isaac’s syndrome, is a disorder characterized by hyperexcitation of motor nerves. Unlike other neuromuscular junction diseases, it does not cause muscle weakness. Neuromyotonia is believed to have an autoimmune origin and is associated with down-regulation of voltage-gated potassium channels, leading to increased neurotransmitter release and repetitive firing of motor nerves.
- On the genetic side, congenital myasthenic syndromes (CMS) are inherited disorders caused by mutations in genes that affect various proteins in the neuromuscular junction. These mutations can impact the function and expression of the acetylcholine receptor and other proteins involved in synaptic transmission. CMS can manifest during different stages of life and present with symptoms such as muscle weakness, ptosis, ophthalmoplegia, and breathing difficulties.
- Treatment approaches for disorders of the neuromuscular junction depend on the specific condition and its underlying cause. In the case of autoimmune disorders like MG and LEMS, immunosuppressive therapies may be employed to reduce the autoimmune response and improve muscle function. Medications like 3,4-diaminopyridine can be used to enhance muscle strength by prolonging the opening of voltage-gated calcium channels. For certain subtypes of CMS, 3,4-diaminopyridine is also being investigated as a potential treatment option.
Overall, disorders of neuromuscular junctions pose significant challenges to patients due to their impact on muscle function and quality of life. Ongoing research and advancements in treatment strategies aim to improve the management and outcomes for individuals affected by these conditions.
Toxins and Drugs Acting at Neuromuscular Junction
Toxins and drugs can have significant effects on the neuromuscular junction, either by blocking or stimulating its function. Here are some examples:
- Neuromuscular Blockers: a. Botulinum Toxin: Derived from Clostridium botulinum bacteria, this toxin blocks neuromuscular transmission by preventing the release of acetylcholine (ACh) from the nerve endings. It interferes with SNARE proteins, inhibiting vesicle fusion and ACh release. b. Curare: This competitive inhibitor binds to ACh receptors on the postsynaptic membrane, preventing ACh from binding and generating endplate potentials. c. Bungarotoxin: Found in snake venom, bungarotoxin binds to ACh receptors, blocking neuromuscular transmission. d. Succinylcholine and Carbamylcholine: These drugs keep the muscle depolarized, mimicking the action of ACh. They are not broken down by acetylcholinesterase, leading to prolonged depolarization.
- Neuromuscular Stimulators: a. Drugs with ACh-like Action: Carbachol and nicotine are not efficiently broken down by acetylcholinesterase, leading to repeated stimulation of the neuromuscular junction and continuous muscle activity. b. Drugs that Inactivate AChE: Neostigmine and physostigmine inhibit acetylcholinesterase, leading to increased ACh levels at the neuromuscular junction and stimulation of muscle activity.
Nerve gases, such as sarin, bind to and phosphorylate acetylcholinesterase, rendering it inactive. This results in the accumulation of ACh in the synaptic cleft, causing continuous muscle contraction and potentially leading to paralysis and death.
Botulinum toxin, commercially known as Botox, is used in medical and cosmetic procedures. It inhibits ACh release by cleaving SNARE proteins, causing temporary flaccid paralysis and chemical denervation of the affected muscles. The effects of botulinum toxin begin approximately two weeks after injection and gradually wear off over several months.
Tetanus toxin, produced by Clostridium tetani, functions similarly to botulinum toxin by interfering with SNARE proteins. However, tetanus toxin causes spastic paralysis, characterized by sustained muscle contractions.
Latrotoxin found in widow spider venom stimulates the release of ACh from the presynaptic cell, leading to pain, muscle contraction, and potential paralysis.
Snake venom can act as both presynaptic and postsynaptic neurotoxins. Presynaptic neurotoxins inhibit the release of neurotransmitters like ACh, while postsynaptic neurotoxins bind to postsynaptic ACh receptors, preventing their activation. These toxins can cause weakness and paralysis.
Understanding how toxins and drugs interact with the neuromuscular junction provides valuable insights into its normal function and helps develop treatments for related conditions, such as muscle disorders and myasthenia gravis.
Singnificance of Neuromuscular junction
The neuromuscular junction (NMJ) is a crucial connection between motor neurons and skeletal muscle fibers. It plays a significant role in transmitting signals from the nervous system to the muscles, allowing voluntary movement and control over muscle contractions. The significance of the neuromuscular junction can be understood from the following perspectives:
- Muscle Contraction: The NMJ is responsible for initiating muscle contraction. When an action potential reaches the presynaptic terminal of the motor neuron, it triggers the release of the neurotransmitter acetylcholine (ACh) into the synaptic cleft. ACh binds to receptors on the postsynaptic membrane of the muscle fiber, leading to depolarization and the generation of an action potential in the muscle. This process enables muscle fibers to contract and generate force, allowing movement and physical activities.
- Precision and Control: The NMJ allows precise control over muscle contractions. Each motor neuron typically innervates multiple muscle fibers, forming a motor unit. The size and composition of motor units can vary depending on the specific muscle and its function. Fine motor control requires smaller motor units with fewer muscle fibers, while larger motor units are responsible for generating more forceful contractions. By selectively activating motor units, the nervous system can control muscle movement with remarkable precision.
- Neurotransmitter Regulation: The NMJ plays a critical role in regulating the levels and actions of neurotransmitters. After ACh binds to the postsynaptic receptors, it is rapidly broken down by the enzyme acetylcholinesterase (AChE). This ensures that the muscle fibers are not continuously stimulated and allows for precise control over muscle contraction duration. Dysfunctions in the regulation of neurotransmitters at the NMJ can lead to various neuromuscular disorders, such as myasthenia gravis.
- Target for Therapeutics: The neuromuscular junction is a target for several therapeutic interventions. Drugs that affect the function of the NMJ, such as neuromuscular blockers, can be used during surgeries to induce muscle relaxation. Conversely, drugs that enhance neurotransmission, such as acetylcholinesterase inhibitors, are used in conditions like myasthenia gravis to improve muscle strength and function.
- Research and Disease Studies: The NMJ serves as a valuable model system for studying synaptic function and understanding various neuromuscular disorders. Researchers investigate the mechanisms of neurotransmitter release, receptor interactions, and signaling pathways at the NMJ. Diseases affecting the neuromuscular junction, including myasthenia gravis, Lambert-Eaton syndrome, and congenital myasthenic syndromes, provide insights into the molecular and cellular mechanisms underlying synaptic dysfunction and muscle weakness.
FAQ
What is the neuromuscular junction?
The neuromuscular junction is a specialized synapse where a motor neuron communicates with a muscle fiber. It is responsible for transmitting signals from the nervous system to the muscle, initiating muscle contractions.
How does the neuromuscular junction work?
When an action potential reaches the presynaptic terminal of a motor neuron, it triggers the release of the neurotransmitter acetylcholine (ACh). ACh binds to receptors on the postsynaptic membrane of the muscle fiber, leading to depolarization and the generation of an action potential in the muscle, resulting in muscle contraction.
What happens if there is a dysfunction at the neuromuscular junction?
Dysfunctions at the neuromuscular junction can lead to various disorders, such as myasthenia gravis, Lambert-Eaton syndrome, and congenital myasthenic syndromes. These conditions can cause muscle weakness, fatigue, and impaired muscle control.
How is neurotransmission terminated at the neuromuscular junction?
The neurotransmitter acetylcholine (ACh) is rapidly broken down by the enzyme acetylcholinesterase (AChE) present in the synaptic cleft. This enzymatic breakdown ensures that the muscle is not continuously stimulated and allows for precise control over muscle contraction duration.
What are neuromuscular blockers?
Neuromuscular blockers are drugs that interfere with the neuromuscular transmission at the neuromuscular junction. They can induce muscle relaxation and are commonly used during surgeries to facilitate intubation and improve surgical conditions.
What is the role of the neuromuscular junction in muscle diseases?
The neuromuscular junction is often affected in various muscle diseases, such as muscular dystrophy and myasthenia gravis. Understanding the molecular and cellular mechanisms at the neuromuscular junction is crucial for studying and developing treatments for these conditions.
Can the neuromuscular junction regenerate after injury?
Yes, the neuromuscular junction has the ability to regenerate after injury. In cases of nerve damage or trauma, the nerve fibers can regrow and reestablish connections with muscle fibers, restoring neuromuscular function.
How is the neuromuscular junction studied in research?
Researchers use various techniques to study the neuromuscular junction, including electrophysiological recordings, imaging methods, and genetic manipulation of model organisms. These approaches help in understanding synaptic transmission, synaptic plasticity, and the underlying molecular processes.
Are there any diseases caused by toxins targeting the neuromuscular junction?
Yes, certain toxins can target the neuromuscular junction and interfere with its function. For example, botulinum toxin (Botox) blocks the release of acetylcholine, leading to temporary muscle paralysis.
Can drugs affect the neuromuscular junction?
Yes, there are drugs that can affect neuromuscular transmission. For instance, acetylcholinesterase inhibitors, such as neostigmine, are used to increase acetylcholine levels and enhance neuromuscular function in conditions like myasthenia gravis.