What is Myeloperoxidase staining (MPO Staining)?
Myeloperoxidase (MPO) staining is a vital technique in medical diagnostics, particularly in the field of hematology. MPO is an enzyme predominantly found in certain white blood cells, namely neutrophils, eosinophils, and to a lesser extent, monocytes. Notably absent in lymphocytes, the presence and activity of myeloperoxidase play a crucial role in differentiating between types of leukemia.
Primarily stored in azurophilic granules within neutrophils, myeloperoxidase is a lysosomal enzyme. Its primary function is to produce hypohalous acids, which are essential for the antimicrobial activities of these white blood cells. Among these acids, hypochlorous acid is particularly significant, as it is a powerful antimicrobial agent, similar in composition to household bleach. This antimicrobial function is vital for the body’s defense mechanism against pathogens.
The myeloperoxidase gene is located on chromosome 17 in humans. The enzyme’s presence is most pronounced in neutrophils, a type of white blood cell playing a key role in the immune response. During certain immune reactions, such as inflammation, neutrophils release MPO into the extracellular space, a process known as degranulation.
A unique characteristic of myeloperoxidase is its green coloration, which is due to the heme pigment in its structure. This green hue is often observable in secretions rich in neutrophils, like mucus and sputum, and was historically the reason behind its former name, verdoperoxidase.
In medical diagnostics, MPO staining is a crucial tool. It is particularly used to distinguish between acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL). The presence of MPO in cells is indicative of AML, as these cells are derived from myeloid lineage, where MPO is typically found. In contrast, its absence suggests ALL, where lymphoid cells (lacking MPO) are involved. This differentiation is critical for accurate diagnosis and appropriate treatment planning for leukemia patients.
In summary, myeloperoxidase staining is an essential diagnostic tool in hematology. It leverages the unique properties of the MPO enzyme, predominantly its presence in specific white blood cells and its antimicrobial function, to provide critical insights into various blood disorders, most notably in differentiating types of leukemia.
Purpose of Myeloperoxidase stain
- To differentiate the blasts of acute myeloid leukemia (AML) from those of acute lymphoblastic leukemia (ALL).
- To diagnose congenital deficiency of neutrophil myeloperoxidase.
Principle of MPO stain (Myeloperoxidase stain)
The principle underlying the Myeloperoxidase (MPO) stain in pathology hinges on the specific biochemical properties of the myeloperoxidase enzyme found in certain leukocyte granules. This technique is employed to visualize and identify the presence of MPO in leukocytes, particularly useful in differentiating types of leukemia cells and understanding immune cell functions.
At its core, the MPO staining process involves a reaction where the myeloperoxidase enzyme, in the presence of hydrogen peroxide (H2O2), oxidizes certain substrates. These substrates, which are typically colorless in their original form, are transformed into insoluble blue or brown derivatives. This reaction occurs specifically at the site of MPO activity within the leukocyte granules, thereby marking the presence and location of the enzyme.
Commonly used substrates for this reaction include Benzidine, 3,3′-Diaminobenzidine (DAB), or p-phenylenediamine dihydrochloride. When these substrates encounter the MPO-H2O2 complex, they undergo oxidation and precipitate at the site, forming stable, non-diffusible products. This localized precipitation ensures that the staining accurately reflects the presence and distribution of MPO within the cells.
Additionally, the staining intensity and clarity can be enhanced by the addition of agents such as copper sulfate or nitrate. These compounds facilitate the oxidation process, leading to a more pronounced and discernible color change, which is crucial for accurate visualization under a microscope.
Requirements for Myeloperoxidase staining (MPO Stain)
For conducting Myeloperoxidase (MPO) staining, a specific set of requirements must be met to ensure accurate and reliable results. This staining procedure is an essential tool in histopathology for identifying myeloperoxidase enzyme presence in leukocytes. The following are the key components required for MPO staining:
- Fixative: An appropriate fixative is crucial for preserving the tissue sample’s structure and enzymes. Commonly used fixatives for MPO staining include 10% formalin in ethanol or buffered formal acetone. These fixatives help to maintain the integrity of the leukocyte granules and ensure that the myeloperoxidase enzyme is retained in its active form.
- Substrate: The substrate is a vital component of the staining process, reacting with myeloperoxidase in the presence of hydrogen peroxide. Options for substrates include Benzidine, 3,3′-diaminobenzidine (DAB), or p-phenylenediamine dihydrochloride. The choice of substrate determines the color and intensity of the stain, with each substrate offering specific properties that can be beneficial for different applications.
- Buffer: Sorensen’s phosphate buffer at pH 7.3 is used to maintain an optimal pH environment for the enzymatic reaction. The buffer helps in stabilizing the reaction conditions, ensuring that the MPO enzyme functions effectively during the staining process.
- Hydrogen Peroxide: A 3% solution of hydrogen peroxide is used as a reactant in the staining process. It works in conjunction with the substrate to facilitate the oxidation reaction, which leads to the formation of the colored stain.
- Working Substrate Solution: To prepare the working substrate solution, 30 mg of DAB is dissolved in 60 ml of the Sorensen’s phosphate buffer. Then, 120 µl of hydrogen peroxide is added and mixed thoroughly. This solution is used for the actual staining process, where it reacts with the MPO enzyme in the tissue sample.
- Counterstain: Hematoxylin is commonly used as a counterstain in MPO staining. It provides a contrasting color, typically staining nuclei blue. This contrast enhances the visibility of the MPO stain and allows for better differentiation of cellular structures within the tissue sample.
| Requirement | Description |
|---|---|
| Fixative | 10% formalin in ethanol or buffered formal acetone. Used for preserving tissue structure and enzyme integrity. |
| Substrate | Options include Benzidine, 3,3′-diaminobenzidine (DAB), or p-phenylenediamine dihydrochloride. Key for the color development in the staining process. |
| Buffer | Sorensen’s phosphate buffer, pH 7.3. Maintains the optimal pH for the enzymatic reaction. |
| Hydrogen Peroxide | 3% solution. Reacts with the substrate to facilitate the oxidation reaction for stain development. |
| Working Substrate Solution | Prepared by dissolving 30 mg of DAB in 60 ml of buffer, then adding 120 µl of hydrogen peroxide. Used for the staining process. |
| Counterstain | Hematoxylin. Provides contrasting color to enhance the visibility of the MPO stain and differentiate cellular structures. |
Procedure of Myeloperoxidase staining (MPO Stain)
- Fixation of Smears: Begin by fixing air-dried smears in formalin ethanol or buffered formal acetone. This step should last for about 60 seconds. The fixation process is crucial as it preserves the cellular structure and enzymes within the smear.
- Rinsing: After fixation, the smears should be thoroughly rinsed in running tap water. A duration of 30 seconds is typically sufficient. This step helps to remove any residual fixative that might interfere with the staining process.
- Application of Working Substrate: Next, cover the smear with the working substrate solution and incubate it for 10 minutes. The working substrate contains the components necessary for the MPO enzyme to react and produce a visible color change in the smear.
- Washing: Following incubation, gently wash the smear with running tap water for another 30 seconds. This step removes excess substrate and prepares the smear for counterstaining.
- Counterstaining: Counterstain the smear with hematoxylin for 3-5 minutes. Hematoxylin will stain the nuclei within the cells, providing a contrast that enhances the visibility of the MPO stain.
- Final Rinse and Drying: After counterstaining, rinse the smear again in running tap water and then allow it to air dry. This step ensures that any excess counterstain is removed and that the smear is ready for microscopic examination.
- Microscopic Examination: Finally, examine the smear under a microscope. The MPO stain will highlight the presence of myeloperoxidase enzyme in the cells, aiding in the diagnosis and analysis of hematological conditions.
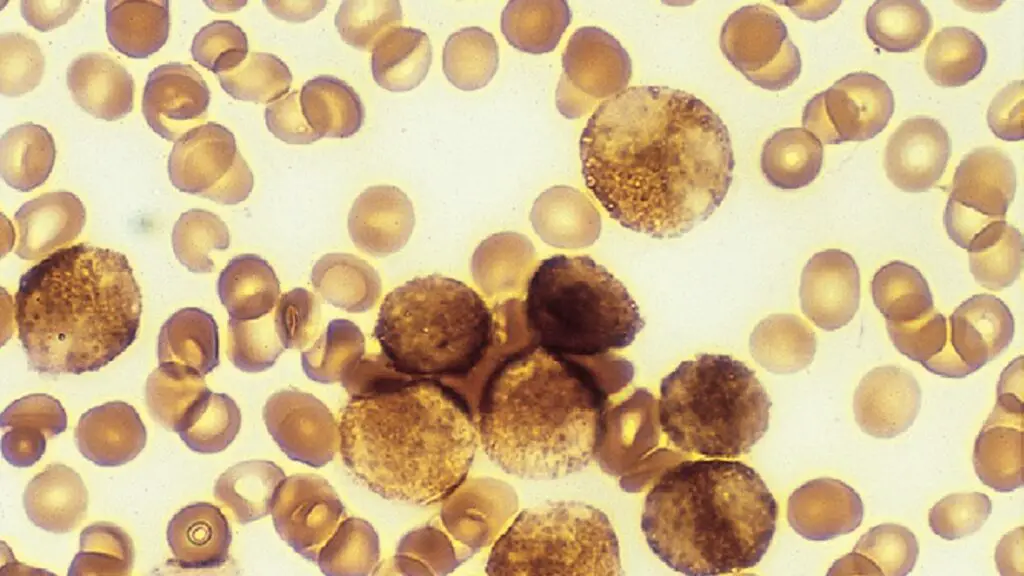
Myeloperoxidase staining Result and Interpretation
MPO Staining Results:
- Presence in Myeloid Cells: MPO is typically found in the primary granules of myeloid cells. However, early myeloblasts, which are immature myeloid cells, generally do not show MPO positivity. As these cells mature, granular positivity for MPO becomes more apparent.
- Acute Myeloid Leukemia (AML): In many cases of AML, including types M1 (without maturation), M2 (with maturation), and M3 (promyelocytic leukemia), over 80% of blasts exhibit MPO activity. Auer rods, which are needle-like inclusions found in some leukemia cells, are strongly positive for MPO.
- Monocytic Series: Cells of the monocytic lineage tend to show a less intense positive reaction for MPO. This reaction is characterized by fine granular deposits scattered throughout the cell.
- Lymphoblasts and Lymphoid Cells: These cells are typically negative for MPO, providing a clear differential marker from myeloid cells.
| Cell Type | MPO Staining Result | Notes |
|---|---|---|
| Myeloblasts (Early) | Negative | Lack of MPO in early stages, with positivity in maturation. |
| Mature Myeloid Cells | Positive | Granular positivity increases with maturation. |
| Acute Myeloid Leukemia (AML) | Positive in >80% of blasts | Includes AML types M1, M2, M3. Auer rods are strongly positive. |
| Monocytic Series | Less Intense Positive | Characterized by fine granular deposits. |
| Neutrophilic Granulocytes | Positive (except in blast forms) | Mature forms show positivity. |
| Eosinophils | Positive | Consistently show MPO positivity. |
| Monocytes (Mature) | Positive (except in blast forms) | Generally positive for MPO. |
| Basophils | Weakly Positive or Negative | Typically show weak or no MPO activity. |
| Lymphoblasts and Lymphoid Cells | Negative | Important for differentiation from myeloid leukemias. |
| Erythrocyte Cell Series | Negative | Red blood cells and precursors do not show MPO activity. |
Interpretation of MPO Staining:
- Positive MPO Reaction:
- Neutrophilic Granulocytes: Mature neutrophilic granulocytes display a positive MPO reaction, except in their blast forms.
- Eosinophils: These cells also show positive MPO staining.
- Monocytes: Mature monocytes, excluding their blast forms, are generally positive for MPO.
- Negative MPO Reaction:
- Basophils: These cells are weakly positive or negative for MPO.
- Lymphocytic Cell Series: Lymphoblasts and other lymphoid cells do not exhibit MPO activity, which is a critical diagnostic feature in distinguishing lymphocytic from myeloid leukemias.
- Erythrocyte Cell Series: Red blood cells and their precursors do not show MPO activity.
In summary, the results and interpretation of MPO staining are essential in the identification and classification of blood cells, particularly in the diagnosis of various forms of leukemia. The presence or absence of MPO in cells provides valuable information about their lineage and stage of maturation, which is crucial for accurate diagnosis and treatment planning in hematological disorders.
Uses of Myeloperoxidase Staining
- Diagnosis of Leukemia Types: MPO staining is crucial in differentiating between acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL). In AML, cells typically show positive MPO staining due to their myeloid origin, whereas ALL cells, being of lymphoid origin, do not.
- Determining Cell Lineage: MPO staining helps in identifying the lineage of immature white blood cells (blasts) in bone marrow or peripheral blood. This is important in diagnosing various forms of blood cancers and other hematological disorders.
- Identifying Myeloid Dysplasia: In conditions like myelodysplastic syndromes, MPO staining can help in assessing the maturation and differentiation patterns of myeloid cells.
- Assessment of Infectious Diseases: Since neutrophils are a primary defense against bacterial infections, MPO staining can be used to assess neutrophil activity and response in infectious diseases.
- Research in Immunology: In research settings, MPO staining is used to study neutrophil function and the role of myeloperoxidase in various immune responses and inflammatory processes.
- Detection of Auer Rods in Leukemia: Auer rods, which are indicative of certain types of leukemia, are strongly MPO positive. Their detection through MPO staining is significant for diagnostic purposes.
- Evaluation of Congenital Neutrophil Deficiencies: MPO staining is useful in diagnosing congenital deficiencies of neutrophil myeloperoxidase, which can be linked to increased susceptibility to infections.
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.