- The heart possesses a remarkable ability known as autorhythmicity, which enables it to generate its own electrical impulses and rhythm independent of external nervous or hormonal controls. This inherent capacity ensures that the heart beats continuously, sustaining life. However, it is important to note that the heart is also influenced by both sympathetic and parasympathetic fibers from the autonomic nervous system, which can modulate the heart rate according to the body’s needs. Additionally, circulating hormones, such as adrenaline and thyroxine, play a significant role in regulating the heart rate.
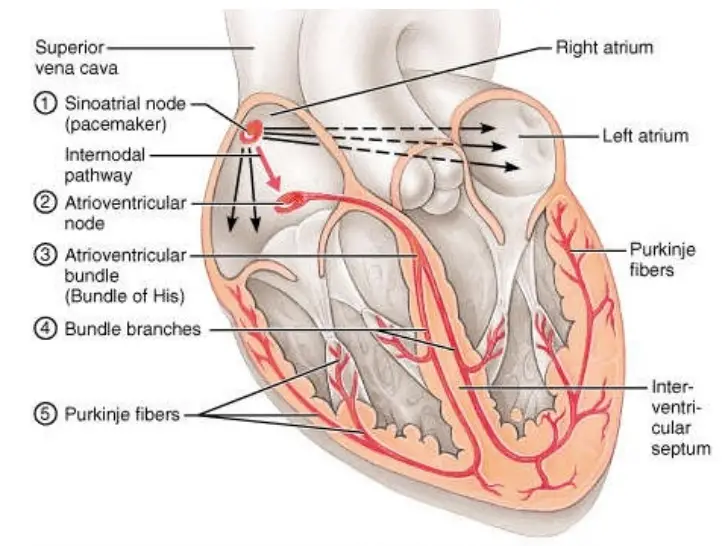
- The central nervous system (CNS) exerts some control over the heart; nevertheless, the cardiac muscle cells of the sinoatrial (SA) node primarily initiate the electrical impulses that drive heartbeats, functioning independently of the CNS. The SA node is a small cluster of specialized cells located in the wall of the right atrium, near the opening of the superior vena cava. These cells exhibit electrical instability, which is crucial for their ability to generate impulses and regulate the heart’s rhythm.
- Due to their electrically unstable nature, the cells of the SA node depolarize at a regular rate of 60 to 80 times per minute under normal physiological conditions. This depolarization creates an electrical impulse that propagates to adjacent muscle cells of the right atrium through gap junctions found in intercalated discs. Consequently, the wave of depolarization spreads throughout the right and left atria, leading to atrial contraction, which facilitates the flow of blood into the ventricles.
- Once the electrical impulse leaves the SA node, it travels to the atrioventricular (AV) node, a small mass of neuromuscular tissue situated in the atrial septum near the tricuspid valve. The AV node serves primarily as a conduit for transmitting electrical signals from the atria to the ventricles. A crucial aspect of the AV node’s function is the built-in delay of approximately 0.1 seconds that occurs during this transmission. This brief pause allows the atria to complete their contraction before the ventricles are stimulated to contract.
- In addition to its role in impulse transmission, the AV node possesses a secondary pacemaker function. In situations where the SA node fails to generate impulses or transmit them effectively, the AV node can take over this responsibility, ensuring the continuation of the heartbeat.
- Following the AV node, the electrical impulse is relayed to a specialized group of conducting fibers known as the Bundle of His (or AV bundle). This bundle originates from the AV node and descends toward the ventricles. Upon reaching the interventricular septum, the Bundle of His bifurcates into right and left bundle branches, which extend into each ventricle. Within the ventricular myocardium, these branches further divide into fine fibers known as Purkinje fibers.
- The coordinated action of the AV node, Bundle of His, and Purkinje fibers ensures that the electrical impulse rapidly propagates throughout the ventricles. This efficient transmission results in synchronized ventricular contraction, which is essential for effective blood ejection into the pulmonary artery and aorta.
- In summary, the conducting system of the heart is an intricate network of specialized cells and fibers that work together to initiate and propagate electrical impulses. This system not only ensures the heart’s rhythmic contractions but also allows for precise coordination between atrial and ventricular activities, ultimately sustaining the vital functions of the cardiovascular system.
Overview of Heart Conduction
The conduction system of the heart is a complex network that orchestrates the electrical signals required for heart muscle contraction. This system ensures that the heart beats in a coordinated manner, facilitating efficient blood circulation throughout the body. The process begins with the generation of an electrical signal, which propagates through various components of the conduction system.
- An excitation signal, known as an action potential, is generated by the sinoatrial (SA) node. This node serves as the primary pacemaker of the heart, initiating the heartbeat.
- Once generated, the wave of excitation spreads across the atria, leading to their contraction. This contraction pushes blood into the ventricles, preparing the heart for the subsequent phase of the cardiac cycle.
- As the wave of excitation reaches the atrioventricular (AV) node, there is a crucial delay in signal transmission. This delay allows the atria to complete their contraction before the ventricles begin to contract, ensuring optimal filling of the ventricles with blood.
- Following this delay, the electrical signal is conducted into the bundle of His. This bundle, also known as the atrioventricular bundle, carries the signal down the interventricular septum, which separates the left and right ventricles.
- The bundle of His subsequently branches into the Purkinje fibers, which spread the wave of impulses throughout the ventricles. This rapid transmission of electrical signals triggers ventricular contraction, allowing blood to be pumped out of the heart and into the pulmonary artery and aorta.
This organized sequence of electrical events is critical for maintaining a rhythmic and effective heartbeat. The heart’s conduction system ensures that each contraction is synchronized, thus optimizing cardiac output and overall physiological function.
Components of the Cardiac Conduction System
The cardiac conduction system is a specialized network responsible for initiating and propagating electrical impulses throughout the heart. This system consists of several key components, each with distinct functions that contribute to the heart’s rhythmic contraction and effective blood circulation.
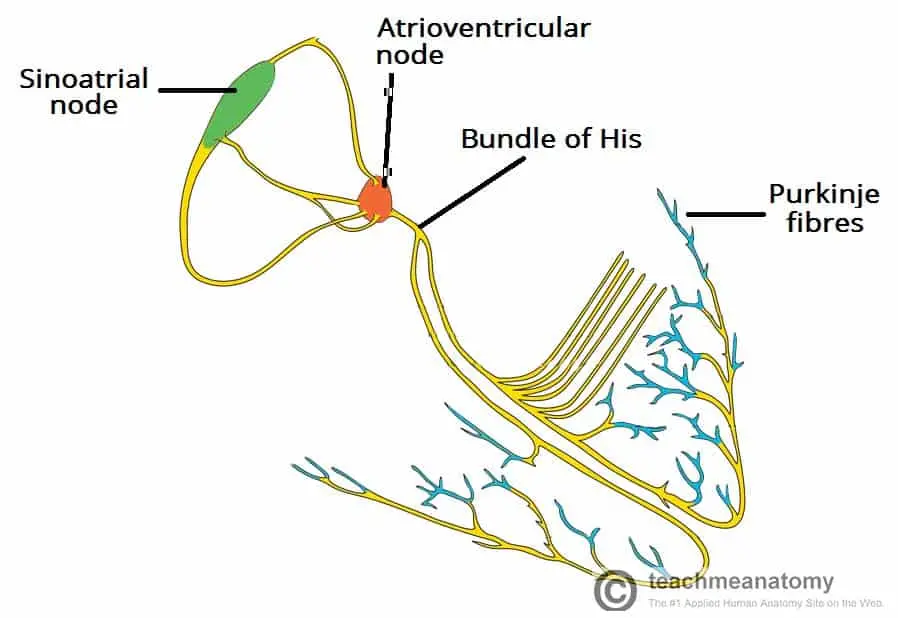
- Sinoatrial (SA) Node
The SA node is a cluster of specialized pacemaker cells located in the upper wall of the right atrium, specifically at the junction where the superior vena cava enters. These pacemaker cells possess the unique ability to spontaneously generate electrical impulses. When activated, the wave of excitation spreads through gap junctions across both atria, leading to atrial contraction, or atrial systole. This contraction facilitates the movement of blood from the atria into the ventricles. The firing rate of the SA node is modulated by the autonomic nervous system:- The sympathetic nervous system enhances the firing rate of the SA node, thereby increasing the heart rate.
- The parasympathetic nervous system reduces the firing rate of the SA node, resulting in a decreased heart rate.
- Atrioventricular (AV) Node
Following the propagation of electrical impulses across the atria, these impulses converge at the AV node, situated within the atrioventricular septum near the opening of the coronary sinus. The primary function of the AV node is to delay the electrical impulses by approximately 120 ms. This delay ensures that the atria have sufficient time to completely eject blood into the ventricles prior to the onset of ventricular contraction, or ventricular systole. Once the delay has occurred, the wave of excitation is transmitted from the AV node into the atrioventricular bundle. - Atrioventricular Bundle (Bundle of His)
The atrioventricular bundle, also known as the bundle of His, serves as a continuation of the specialized tissue from the AV node. Its primary role is to conduct the electrical impulse from the AV node to the Purkinje fibers within the ventricles. The bundle of His descends through the membranous portion of the interventricular septum and subsequently divides into two main branches:- The right bundle branch conducts the impulse to the Purkinje fibers of the right ventricle.
- The left bundle branch transmits the impulse to the Purkinje fibers of the left ventricle.
- Purkinje Fibers
The Purkinje fibers, also known as the sub-endocardial plexus of conduction cells, comprise a network of specialized cells rich in glycogen and characterized by extensive gap junctions. Located in the subendocardial surface of the ventricular walls, these fibers rapidly transmit cardiac action potentials from the atrioventricular bundle to the myocardium of the ventricles. The speed of conduction through the Purkinje fibers allows for coordinated ventricular contraction, or ventricular systole, which propels blood from the right and left ventricles into the pulmonary artery and aorta, respectively.
Mechanism of Impulse Conduction in the Heart
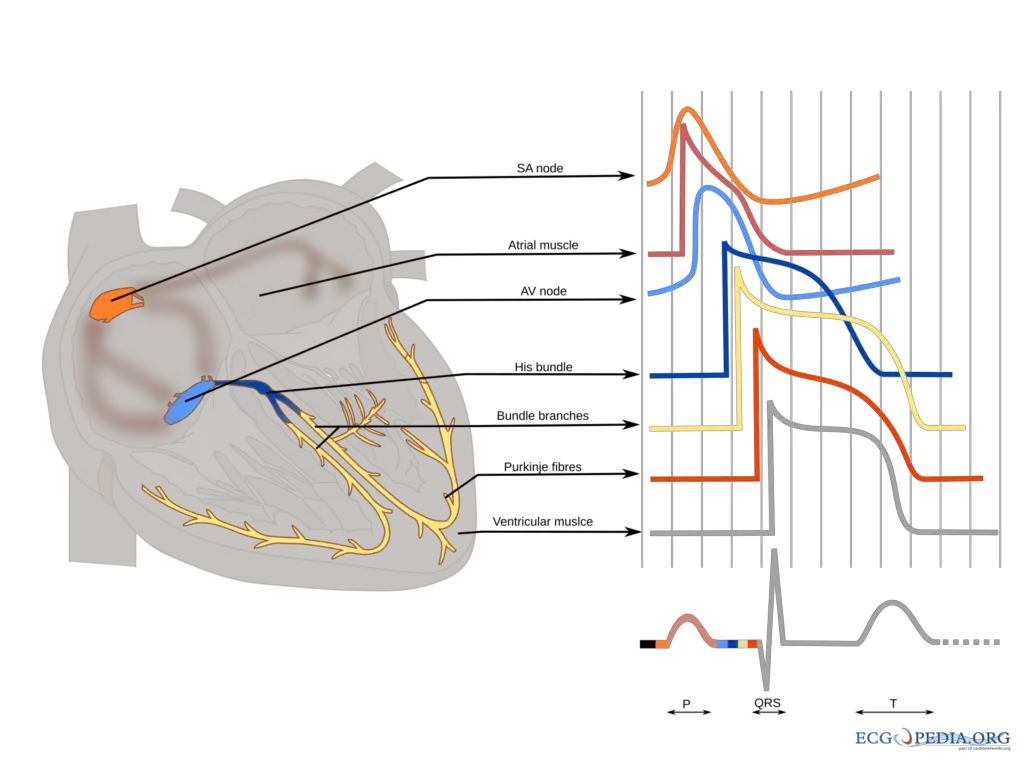
The conduction of electrical impulses in the heart is a highly coordinated process that enables the rhythmic contraction of cardiac muscle. This mechanism is primarily facilitated by specialized action potentials known as cardiac action potentials, which occur in distinct phases. Understanding these phases is crucial for comprehending how the heart maintains its function effectively.
- Resting Potential
At rest, the membrane potential of cardiac muscle fibers, also known as cardiac myocytes, is approximately -90 mV, indicating a stable state under normal conditions. During this phase, the cardiac myocytes are polarized and not actively transmitting impulses. The sinoatrial (SA) node, which serves as the primary pacemaker of the heart, generates electrical impulses that initiate depolarization. The SA node has the unique capability to depolarize regularly without external influences, sending depolarization waves to adjacent atrial cells. - Depolarization
During this phase, there is a substantial influx of sodium ions (Na⁺) through fast voltage-gated sodium channels. This influx rapidly reverses the membrane potential from -90 mV to approximately +30 mV. Concurrently, the permeability of the membrane to potassium ions (K⁺) decreases as potassium channels close, preventing K⁺ from exiting the cell. The combined effect of increased Na⁺ concentration within the cell and decreased K⁺ concentration outside the cell results in depolarization. - Early Repolarization
This phase is characterized by the inactivation of sodium channels, which occurs due to the simultaneous influx of calcium ions (Ca²⁺) through slow voltage-gated calcium channels. The increased Ca²⁺ concentration initiates the release of more calcium ions from the sarcoplasmic reticulum, which further stimulates muscle contraction. Additionally, the opening of potassium channels allows K⁺ to exit the cell, contributing to the early stages of repolarization. - Plateau
During the plateau phase, the action potential remains stable at approximately +30 mV due to a delicate balance between the inward movement of Ca²⁺ and the outward movement of K⁺. Minor contributions to this phase come from the Na-Ca exchanger and Na⁺/K⁺ pumps. This prolonged action potential prevents immediate repolarization, creating a refractory period of 0.25 seconds, which is significantly longer—about nine times—than that of skeletal muscle. This extended refractory period allows the heart to refill with blood and prevents the occurrence of extra beats. - Repolarization
In the final phase, potassium channels reopen while calcium channels gradually close, resulting in the outward movement of K⁺ and blocking the inward flow of Ca²⁺. This efflux of K⁺ ions leads to an increase in the negative charge inside the cell, thus restoring the membrane potential back to -90 mV. However, the distribution of ions is altered, with an elevated concentration of K⁺ outside the cell and Na⁺ inside. Consequently, sodium ions are actively pumped out of the cell while potassium ions are pumped back in via the Na⁺/K⁺ pump, re-establishing the resting membrane potential.
- https://www.onlinebiologynotes.com/conducting-system-of-heart-beat/
- https://ecgwaves.com/topic/structure-and-function-of-myocardial-fibers-myocardium/
- https://courses.lumenlearning.com/suny-ap2/chapter/cardiac-muscle-and-electrical-activity/
- https://teachmeanatomy.info/thorax/organs/heart/conducting-system/
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.