- Coccidioidomycosis, also known as cocci, Valley fever, California fever, arid rheumatism, and San Joaquin Valley fever, is a fungal disease of mammals caused by Coccidioides immitis or Coccidioides posadasii. Coccidioidomycosis is endemic in sections of Arizona, California, Nevada, New Mexico, Texas, Utah, and northern Mexico, among other states.
- C. immitis is a dimorphic saprophytic fungus that produces a spherule form in the host organism and grows as mycelium in the soil. It inhabits the soil in sections of the southwestern United States, including California and Arizona.
- It is also common in regions of Central and South America and northern Mexico. C. immitis is dormant during extended periods of drought, and when it rains, it transforms into a mold with long filaments that break off into airborne spores.
- The spores, also known as arthroconidia, are dispersed into the air when the soil is disturbed, such as during construction, cultivation, low-wind or dust events, or an earthquake.
- Additionally, windstorms may cause epidemics outside of endemic regions. In December 1977, a windstorm in an endemic region near Arvin, California caused hundreds of cases and deaths in nonendemic regions hundreds of miles distant.
- In endemic regions of the United States, coccidioidomycosis is a prevalent cause of community-acquired pneumonia.Infections are typically caused by inhaling arthroconidial particles after soil disruption.The disease is not transmissible.In certain instances, an infection may recur or become chronic.
Coccidioides is a genus of dimorphic fungi that exist as both mycelia and spherules. Mycelia and spherules are both asexual structures. Sexual coccidiosis has not been identified. The results of a molecular analysis indicate that Coccidioides is related to ascomycetes such as Histoplasma capsulatum and Blastomyces dermatitidis. There are two recognized taxa within the genus Coccidioides: C. immitis and Coccidioides posadasii. C. immitis is found in California, whereas C. posadasii is found in other U.S. states and internationally. Clinical manifestation and in vitro susceptibility are identical between these two species. The two Coccidioides species are phenotypically identical and can only be distinguished using molecular techniques. Consequently, clinical microbiology laboratories do not routinely identify Coccidioides species to the species level. This fungus thrives in arid, salt-rich environments. Coccidioides grow in mycelia or filamentous form in soil and agar.
When inhaled, the infectious particles of Coccidiosis species, arthroconidia, are deposited in the lungs. In the lung and tissues, arthroconidia morph into spherules. Endospores are contained within spherules (2 to 5 micrometers in diameter). This spherule can rupture within tissues, releasing endospores that can amplify an infection.
After five or seven days of incubation, Coccidioides species thrive on the majority of mycological and bacterial media. Typically, colonies are white in color. Despite this, appearance is not diagnostic. The yeast is extremely contagious at this stage. There have been outbreaks among laboratory personnel; therefore, the laboratory must be notified when Coccidiosis species are suspected.
Causative agents of coccidioidomycosis
- Coccidioidomycosis, also known as Valley Fever, is a fungal infection caused by the soil-dwelling fungi of the genus Coccidioides. There are two species of Coccidioides that can cause coccidioidomycosis: Coccidioides immitis and Coccidioides posadasii.
- These fungi are found in the soil of arid and semi-arid regions of the southwestern United States, Mexico, and parts of Central and South America. When the soil is disturbed, such as during construction or farming activities, the fungi can become airborne in the form of spores. People can then inhale the spores, which can lead to infection.
- Coccidioidomycosis is not contagious and cannot be transmitted from person to person. The risk of infection is highest for people who live in or travel to endemic areas, particularly those who work outdoors, such as construction workers, farmers, and military personnel. People with weakened immune systems are also at higher risk of developing severe or disseminated coccidioidomycosis.
Risk factors of Coccidioidomycosis infection
- Geographic Location: Coccidioidomycosis is most commonly found in the southwestern United States, particularly in California, Arizona, New Mexico, and Texas. The risk of infection is higher in these regions due to the prevalence of the fungus in the soil.
- Season: The risk of infection is higher during the dry season, when the fungus is more likely to be airborne and easily inhaled.
- Occupation: People who work in agriculture, construction, or any other profession that involves disturbing the soil are at increased risk of inhaling the fungus.
- Age: Elderly individuals and young children are more vulnerable to Coccidioidomycosis, as their immune systems may not be as strong as those of healthy adults.
- Immunodeficiency: People with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy, are at higher risk of developing severe forms of Coccidioidomycosis.
- Pregnancy: Pregnant women are more susceptible to Coccidioidomycosis, and the infection can be severe for both the mother and fetus.
- Genetic factors: Certain genetic factors may increase the risk of developing severe forms of Coccidioidomycosis.
Virulence factors of the Coccidioidomycosis causative agents
- In addition to adherence, specialization, and antigenic variation, infectious disease agents like Coccidioidomycosis may possess additional virulence factors that contribute to their ability to cause disease and elude the host immune system.
- Coccidioides, for instance, may produce enzymes such as lipases, proteases, and ureases that degrade host tissues and nutrients in order to aid the fungus in surviving and spreading within the host. The fungus may also produce melanin, a pigment that can shield it from the immune defenses of the host and antifungal drugs.
- Coccidioides may also be capable of forming biofilms, which are communities of microorganisms that adhere to surfaces and protect themselves from host immune defenses and antimicrobial agents. The biofilm matrix creates a physical barrier that prevents immune cells and medications from penetrating the microorganisms and killing them.
- Coccidioides’ ability to form spores and remain latent in the environment for extended periods contributes to its virulence. The spores can endure severe environmental conditions for months to years and remain infectious during that time. When favorable conditions exist, the particles can become airborne and infect susceptible hosts.
- Understanding the complex interactions between the virulence factors of Coccidioides and the host immune system is essential for the development of effective Coccidioidomycosis treatments and vaccines. It may be necessary to target multiple virulence factors to effectively control and prevent this potentially fatal fungal infection.
Clinical features of coccidioidomycosis
Coccidioidomycosis, also known as Valley fever, is a fungal infection caused by the fungus Coccidioides immitis or Coccidioides posadasii. The clinical features of coccidioidomycosis can vary widely depending on the severity and location of the infection.
The most common symptoms of coccidioidomycosis include:
- Flu-like symptoms: Fever, chills, headache, muscle aches, and fatigue.
- Respiratory symptoms: Cough, chest pain, shortness of breath, and difficulty breathing.
- Skin symptoms: A red rash that is painful and can blister.
In some cases, coccidioidomycosis can cause severe disease, such as meningitis, and can lead to death. Other less common symptoms of coccidioidomycosis include joint pain, swollen lymph nodes, weight loss, and night sweats.
The severity of coccidioidomycosis can vary depending on the individual’s overall health, the amount of fungus that enters the body, and the immune system’s ability to fight off the infection. In general, people with weakened immune systems are more likely to develop severe coccidioidomycosis.
Serious Complications
- Patients with compromised immune systems may develop severe complications, such as severe pneumonia with respiratory failure and bronchopleural fistulas necessitating resection, lung nodules, and a potential disseminated form, in which the infection spreads throughout the body.
- The disseminated form of coccidioidomycosis can wreak havoc on the body, resulting in skin ulcers, abscesses, bone lesions, swollen joints with severe pain, inflammation of the heart, urinary tract issues, and inflammation of the brain’s membrane, which can be fatal.
- In 2012, a particularly severe case of meningitis caused by valley fever was initially misdiagnosed as sinus infections and cluster migraines, among others. The patient was unable to work during the diagnosis and initial treatment investigation. Eventually, the proper treatment was identified, albeit with severe adverse effects, requiring four pills per day and medication injected directly into the brain every 16 weeks.
Life cycle of Coccidioides
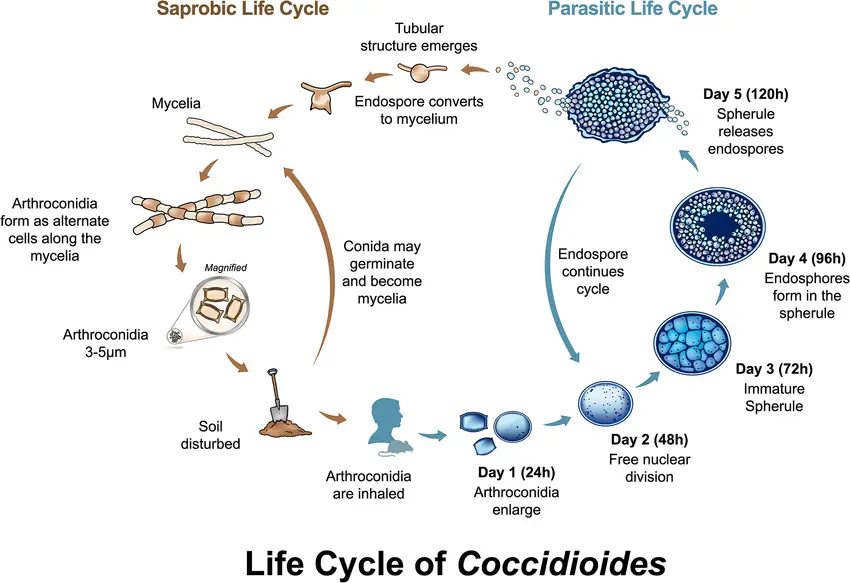
- Both species of Coccidioides have the same asexual life cycle, which alternates between saprobic (on the left) and parasitic (on the right) life stages.
- The environment contains the saprobic cycle, which produces the infectious arthroconidia. The conidia can either be inhaled by a susceptible host or returned to the environment to continue the saprobic life cycle.
- When arthroconidia enlarge and transform into embryonic spherules, either in vivo or under specific in vitro conditions, the parasitic life cycle is initiated.
- Spherules undergo free nuclear division and commence endospore development between 24 and 72 hours.
- The mature spherules rupture between 72 and 120 hours to discharge endospores. Each endospore is capable of initiating a new spherule or, under specific atmospheric conditions, nutrient changes, and/or a lower temperature, transforming into mycelium and initiating the saprobic phase.
- This occurs infrequently in living hosts, whereas it is prevalent in the environment.
Diagnosis of Coccidioidomycosis
Diagnosing Coccidioidomycosis is essential for the proper treatment and administration of the disease. There are a variety of diagnostic techniques available for identifying the infection.
- In order to diagnose Coccidioidomycosis, physical examination and patient history are utilized. X-rays of the chest are taken to detect any unilateral infiltration, lobar consolidation, nodular infiltrate, cavitation, and hilar and peritracheal adenopathy or mediastinal lymphadenopathy for extrathoracic involvement. These X-rays can assist in identifying the disease in its earliest stages.
- Laboratory diagnosis is another method of diagnosis. For diagnosis, specimens such as sputum, pleural fluid, cerebrospinal fluid, lesion exudates, and biopsy are collected. Using KOH Wet mount and calcofluor stains, the spherules of the fungi, which are typically 20 to 80 microns in diameter and have dense walls, can be observed under the microscope.
- The microscopic endospores of C. immitis, measuring between 2 and 4 um, can also be observed. Fungi are also cultured in mycological and/or bacterial media to generate colonies with hyphae containing chains of arthroconidia that form independently from hyphal cells. It is also possible to cultivate and produce spherules of these fungi using a complex medium.
- Coccidioidomycosis, also known as Valley fever, is caused by inhaling spores from the soil-dwelling fungi Coccidioides immitis and Coccidioides posasii. The disease is native to the southwestern United States, specifically Arizona and California, as well as portions of Central and South America.
- Coccidioidomycosis is frequently difficult to diagnose due to its nonspecific symptoms that mimic other respiratory infections. Using sputum or tissue samples, a histological diagnosis can be made to determine the presence of spherules, which are characteristic of the disease. These spherules are double refractile structures with dense walls and a diameter of approximately 80 m.
- The diagnosis of coccidioidomycosis can also be aided by serologic testing. Eosinophilia or elevated levels of inflammatory markers, such as ESR or CRP, may be detected by a complete blood count and differentiation. Anti-coccidioidal antibody testing, which includes IgG and IgM, can corroborate the presence of the disease. Enzyme immunoassays can also detect the presence of disease-specific antibodies and coccidioidal antigens. Immunodiffusion can be used to detect anti-coccidioidomycosis IgM and IgG antibodies.
- Another helpful diagnostic instrument for coccidioidomycosis is the complement fixation test. It assesses the severity of the disease by measuring the complement-fixing antibody concentrations in the blood. Low titers indicate a decline in disease severity or a less severe disease. Important for the diagnosis of coccidioidal meningitis, complement fixation testing can detect the presence of complement-fixing antibodies in cerebrospinal fluid.
- A urine antigen test can be used to detect the presence of the disease in immunocompromised patients with severe manifestations of the disease, such as pneumonia and disseminated disease.
- In endemic regions, delayed cutaneous hypersensitivity is a diagnostic test used in epidemiological investigations. This test is used to detect hypersensitivity to coccidioidin or spherulin, which typically develops in immunocompetent patients within 10 to 21 days after acute infections. However, spherulin is absent in diseases that progress.
- Also used to aid in the diagnosis of coccidioidomycosis is the skin test. In order to administer the coccidioidin skin test, a standardized dilution of coccidioidin is injected into the epidermis. Within 24 to 48 hours, the test is considered positive if there is induration with a diameter of 5 mm or greater.
- Finally, molecular diagnosis using cDNA probing or polymerase chain reaction (PCR) can rapidly identify fungal growth and detect fungal DNA from samples from the lower respiratory tract. These tests are particularly useful in patients with negative serological or histological results but with suspected coccidioidomycosis.
Treatment of Coccidioidomycosis
- Coccidioidomycosis, also known as Valley Fever, is a fungal infection caused by the inhalation of spores of the fungus Coccidioides. Treatment of coccidioidomycosis depends on the severity of the infection and the patient’s overall health.
- Mild cases of coccidioidomycosis may not require treatment and will resolve on their own within a few weeks to months. However, if symptoms are severe, or if the infection has spread to other parts of the body, treatment is necessary.
- The most commonly used medications to treat coccidioidomycosis are antifungal drugs such as fluconazole, itraconazole, and voriconazole. In severe cases, amphotericin B may be used. The duration of treatment depends on the severity of the infection and can range from a few weeks to several months or longer.
- In addition to medication, supportive care can help manage symptoms of coccidioidomycosis. This may include rest, hydration, and pain relief.
- It’s important to note that coccidioidomycosis can be a serious and sometimes life-threatening infection, particularly in people with weakened immune systems. If you suspect you have coccidioidomycosis, you should seek medical attention as soon as possible.
Prevention and Control of Coccidioidomycosis
- Avoiding exposure to dust: The best way to prevent Valley Fever is to avoid exposure to dust in areas where the fungus is known to be present. This includes staying indoors during dust storms, wearing a mask when outside, and using air conditioning to filter the air.
- Covering the skin: Wear long-sleeved shirts and pants to avoid skin contact with soil that may contain the fungus.
- Watering the soil: Keeping the soil moist can help prevent the fungus from becoming airborne. Watering the soil around your home and workplace can be a helpful preventive measure.
- Vaccination: Although there is currently no vaccine available for Valley Fever, research is ongoing to develop one.
- Hospitalization: In severe cases, hospitalization may be necessary for supportive care, such as oxygen therapy and intravenous fluids.
- Reporting: Healthcare professionals are required to report cases of Valley Fever to their local health department. This helps public health officials monitor the spread of the disease and develop strategies to prevent further transmission.
- Education: Public health education campaigns can help raise awareness about the risk of Valley Fever and the measures that individuals can take to prevent infection. This can include information about dust control, wearing protective
- Wear a mask: When working in dusty environments or during dusty conditions, wearing an N95 respirator mask can help reduce your risk of inhaling fungal spores.
- Stay indoors during dust storms: If you live in an area prone to dust storms, try to stay indoors during these events, or wear a mask if you have to go outside.
- Practice good hygiene: Wash your hands regularly with soap and water, and avoid touching your face, especially your nose and mouth.
- Consult a doctor: If you live in an area where coccidioidomycosis is prevalent and you experience flu-like symptoms such as fever, cough, and fatigue, see a doctor promptly.
- Antifungal medication: Antifungal medications such as fluconazole, itraconazole, and amphotericin B may be prescribed to treat severe cases of coccidioidomycosis.
- Prevention in high-risk individuals: People with weakened immune systems, such as those with HIV or undergoing chemotherapy, should take extra precautions to avoid exposure to the fungus.
FAQ
What is coccidioidomycosis?
Coccidioidomycosis, also known as Valley fever, is a fungal infection caused by inhaling spores of the fungus Coccidioides immitis or Coccidioides posadasii. The fungus is found in the soil of arid regions, particularly in the southwestern United States, Central America, and South America.
What are the symptoms of coccidioidomycosis?
The symptoms of coccidioidomycosis can range from mild to severe and can include fever, cough, chest pain, fatigue, headache, joint pain, and rash. In some cases, the infection can spread to other parts of the body and cause more serious complications.
How is coccidioidomycosis diagnosed?
Coccidioidomycosis can be diagnosed by a blood test that detects antibodies to the Coccidioides fungus. In some cases, a culture or biopsy of infected tissue may also be necessary to confirm the diagnosis.
How do people get coccidioidomycosis?
People get coccidioidomycosis by breathing in the spores of the Coccidioides fungus. The fungus is found in the soil, and the spores can become airborne when the soil is disturbed, such as during construction or agricultural activities. People who live or work in areas where the fungus is common are at higher risk of getting the infection.
Is coccidioidomycosis contagious?
No, coccidioidomycosis is not contagious. It cannot be spread from person to person.
References
- Akram SM, Koirala J. Coccidioidomycosis. [Updated 2023 Feb 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448161/
- Lewis, Eric & Bowers, Jolene & Barker, Bridget. (2015). Dust Devil: The Life and Times of the Fungus That Causes Valley Fever. PLoS pathogens. 11. e1004762. 10.1371/journal.ppat.1004762.
- https://www.cdc.gov/fungal/diseases/coccidioidomycosis/index.html#:~:text=Valley%20fever%2C%20also%20called%20coccidioidomycosis,found%20in%20south%2Dcentral%20Washington.
- https://www.cdc.gov/fungal/diseases/coccidioidomycosis/symptoms.html
- https://en.wikipedia.org/wiki/Coccidioidomycosis
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.