| Kingdom: | Fungi |
| Division: | Ascomycota |
| Class: | Saccharomycetes |
| Order: | Saccharomycetales |
| Family: | Saccharomycetaceae |
| Genus: | Candida |
| Species: | C. parapsilosis |
What is Candida parapsilosis?
- Candida parapsilosis is a yeast species that has emerged as a major cause of sepsis and wound and tissue infections in immunocompromised individuals.
- C. parapsilosis, unlike C. albicans and C. tropicalis, is not an obligatory human pathogen, having been isolated from nonhuman sources including domestic animals, invertebrates, and soil.
- C. parapsilosis is a normal human commensal and one of the most frequently isolated fungi from human palms.
- Several risk factors can contribute to the colonization of C. parapsilosis. C. parapsilosis infection is prevalent among immunocompromised individuals and surgical patients, particularly those undergoing surgery of the gastrointestinal tract.
- Currently, there is no consensus regarding the treatment of invasive candidiasis caused by C. parapsilosis; however, the therapeutic approach typically involves the removal of foreign bodies such as implanted prostheses and the administration of systemic antifungal therapy.
- Amphotericin B and Fluconazole are frequently used to treat infections caused by C. parapsilosis. Ashford discovered Candida parapsilosis in Puerto Rico in 1928 from diarrheal feces. It was initially referred to as Monilia parapilosis and deemed nonpathogenic.
- In 1940, it was identified as the causative agent of sepsis in an intravenous drug user.It is currently regarded as a significant, emergent nosocomial pathogen. C. parapsilosis is the most prevalent non-C. albicans Candida species. and the second most prevalent pathogen in superficial candidiasis, after Candida albicans.
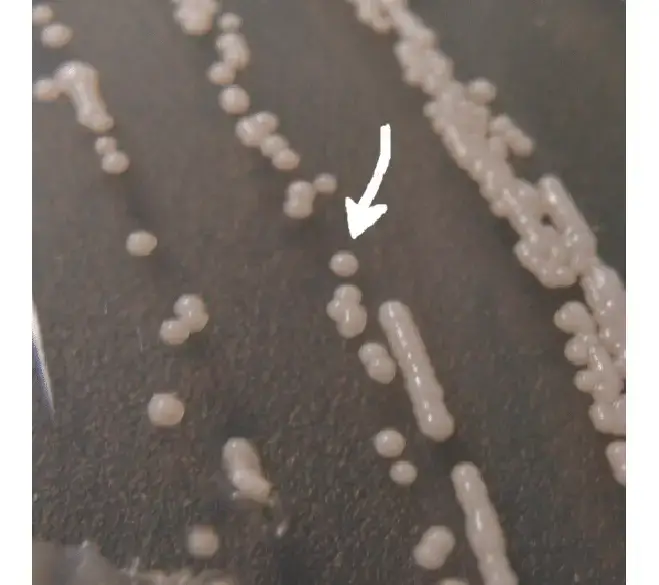
- Candida parapsilosis does not produce genuine hyphae; it only exists in yeast or pseudohyphal phases.In dextrose agar, it is white, creamy, and shiny, and its cell morphology is oval, round, or cylindrical.
- The phenotype of C. parapsilosis in yeast form is either smooth or pitted. In contrast, the pseudohyphae form has a furrowed or concentric phenotype.Citrulline is related to the formation of pseudohyphae, which is a recently discovered factor that alters the morphology and phenotype of colonies.
- C. parapsilosis is encountered more frequently in nature than other Candida species, presumably because it is one of the few non-human-exclusive species of the genus.C. parapsilosis does not require antecedent colonization and is typically transmitted externally.
- In the United States, infants with a low birth weight are prone to invasive infections, and bloodstream infections are common in North America.
- It is most frequently isolated from human skin and is encountered most frequently in Asia and Latin America.Based on its capacity to produce chemicals with cytotoxic effects on the cells of other organisms, C. parapsilosis is considered a killer yeast and fungal antagonist.
Taxonomy of Candida parapsilosis
The taxonomy of Candida parapsilosis is as follows:
- Domain: Eukaryota
- Kingdom: Fungi
- Phylum: Ascomycota
- Subphylum: Saccharomycotina
- Class: Saccharomycetes
- Order: Saccharomycetales
- Family: Saccharomycetaceae
- Genus: Candida
- Species: Candida parapsilosis
Candida parapsilosis belongs to the kingdom Fungi and the phylum Ascomycota, which includes a diverse group of fungi. It falls under the class Saccharomycetes, which is a class of yeast-like fungi. The order is Saccharomycetales, and the family is Saccharomycetaceae. The genus is Candida, which is a large and medically important genus of yeasts. Lastly, the specific epithet is parapsilosis, which distinguishes it as a particular species within the Candida genus.
This taxonomy provides a systematic categorization of Candida parapsilosis within the fungal kingdom, allowing for proper identification and classification of the organism in scientific and medical contexts.
Habitat of Candida parapsilosis
- Human body: Candida parapsilosis is considered to be part of the normal microbial flora on human epidermis and mucous membranes. It is present on the epidermis, in the mouth, and in the digestive and urinary tracts of healthy people.
- The skin: C. parapsilosis is a common skin commensal, which means it lives harmlessly on the epidermis. It occurs most frequently on the hands, feet, and groin.
- The mouth: C. parapsilosis is also a prevalent oral commensal. It occurs most frequently on the tongue and pharynx.
- The gut: C. parapsilosis is a prevalent commensal of the gut. It is typically located in the small intestine.
- Soil: C. parapsilosis is found in soil, where it can persist for extended durations.
- Water: C. parapsilosis is present in water, where it can persist for brief durations.
- Plants: C. parapsilosis is found on plants, where it can persist for extended periods.
- Hospital environments: In hospital settings, Candida parapsilosis is known as an opportunistic pathogen, which means it can cause infections, especially in those with compromised immune systems or who have undertaken invasive medical procedures. It has been linked to healthcare-associated infections and has been detected in hospitals, particularly on catheters, medical devices, and hospital apparatus.
- Community settings: In addition to hospital environments, Candida parapsilosis can also be found in community contexts. It is present on various surfaces and in the environment, such as water, soil, vegetation, and food.
- Animals: Candida parapsilosis has been isolated from animals, including domesticated animals such as canines and cats. Similar to its presence in humans, it can colonize the epidermis, mucous membranes, and gastrointestinal tracts of animals.
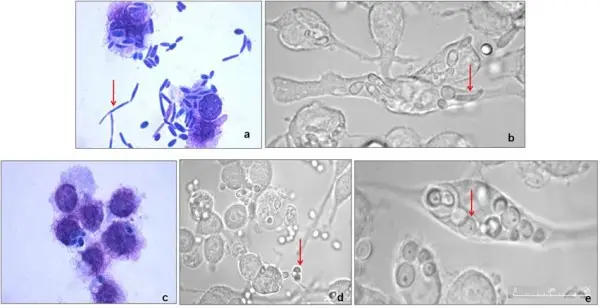
Morphology of Candida parapsilosis
- Cellular Shape: The yeast cells of Candida parapsilosis are typically oval-shaped and single-celled. In general, the diameter of these cells ranges between 2 and 4 micrometers.
- Budding: Candida parapsilosis, like other yeasts, reproduces through a process known as budding. During the process of budding, a small daughter cell develops from the mother cell and ultimately separates to become an independent cell. This process provides yeast cells their distinctive appearance, with a prominent bud or daughter cell attached to the mother cell.
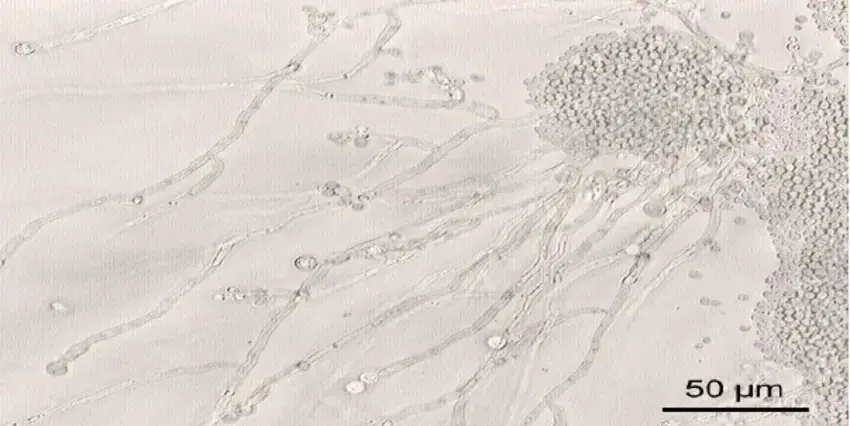
- Pseudohyphae: Under certain conditions, Candida parapsilosis can form pseudohyphae, which are chains of elongated cells. When yeast cells fail to separate completely after budding, a chain-like structure is produced. However, Candida parapsilosis is less likely than other Candida species to produce pseudohyphae.
- Gram Staining: When exposed to a Gram stain, Candida parapsilosis cells appear Gram-positive because they retain the crystal violet stain used in the Gram staining process. This indicates that Candida parapsilosis has a dense layer of peptidoglycan, a characteristic of Gram-positive organisms, in its cell wall.
Cultural characteristics of Candida parapsilosis
- Morphology: Under a microscope, Candida parapsilosis typically appears as ovoid or elongated yeast cells. It reproduces by budding, producing daughter cells that are attached to the mother cell prior to separating.
- Growth on agar media: Candida parapsilosis can thrive on a variety of agar-based laboratory culture media, including Sabouraud dextrose agar and chromogenic media. It typically creates white to cream-colored colonies that are smooth, creamy, or glossy. It is essential to observe, however, that the appearance of a colony alone is insufficient for accurate identification.
- Biochemical tests: To differentiate Candida parapsilosis from other Candida species, biochemical assays can be conducted. These studies involve carbohydrate assimilation (e.g., glucose, lactose, maltose, etc.) and enzymatic reactions (e.g., urease production).
- Molecular techniques: With the development of molecular techniques, DNA-based methodologies such as polymerase chain reaction (PCR) and DNA sequencing can be used to identify Candida parapsilosis with pinpoint accuracy.
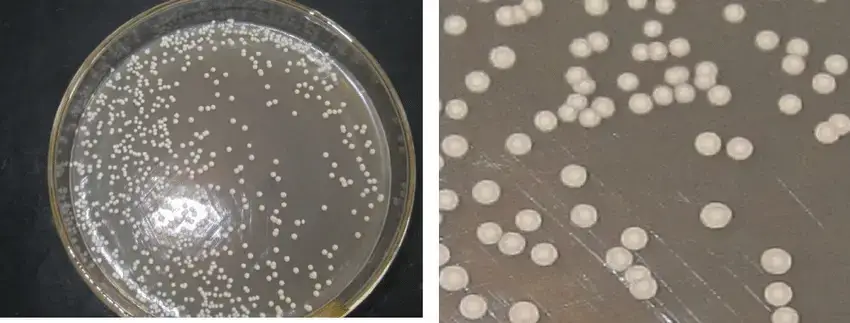
Culture Media used for the growth of Candida parapsilosis
- Sabouraud Dextrose Agar (SDA): This is a commonly used medium for the cultivation of yeasts and fungi. It contains dextrose (glucose) as a source of carbon, peptone or tryptone as a source of nitrogen, and agar as a thickener. SDA’s low pH (approximately 5.6) promotes the proliferation of Candida species.
- Chromogenic Agar: Agar containing chromogenic substrates that change color when metabolized by particular microorganisms. Some commercially available chromogenic media, including CHROMagar Candida, can be used to identify and differentiate Candida species, including Candida parapsilosis.
- Cornmeal Agar: Cornmeal Agar is a specialized medium used to characterize the morphology of Candida species. It contains cornmeal as a nutrient source, which encourages Candida parapsilosis to produce chlamydospores. Candida parapsilosis is distinguished by the presence of chlamydospores, which can aid in its identification.
- Yeast Extract-Peptone-Dextrose (YPD) Agar: (YPD) is Yeast Extract-Peptone-Dextrose. YPD Agar is a versatile medium used to cultivate yeasts, including Candida species. Yeast extract, peptone, dextrose, and agar are present. The nutrient-rich environment provided by YPD agar promotes the growth of Candida parapsilosis.
Pathogenesis of Candida parapsilosis
- Adherence and Biofilm Formation: Candida parapsilosis is capable of adhering to host tissues and medical devices including catheters, prosthetic joints, and intravenous lines. It has adhesins, which consist of proteins and polysaccharides, on its cell surface, allowing it to bind to host cells and form biofilms. Biofilms are microorganism communities encased in a protective matrix that provide increased resistance to host defenses and antifungal agents.
- Secreted Hydrolytic Enzymes: Hydrolytic Enzymes Secreted Candida parapsilosis secretes a variety of hydrolytic enzymes, including proteinases and phospholipases. By degrading host proteins and compromising the integrity of host cell membranes, these enzymes promote tissue invasion and injury.
- Evasion of Host Immune Response: Evasion of the Host Immune Response Candida parapsilosis possesses a number of mechanisms to evade or modulate the host immune response. It can alter the surface protein expression in order to avoid immune recognition. It can also produce molecules that interfere with host immune cell functions, such as inhibiting neutrophil phagocytosis or reducing immune cell activity.
- Production of Virulence Factors: The virulence factors produced by Candida parapsilosis contribute to its pathogenesis. Extracellular proteases, phospholipases, lipases, and hemolysins are involved in tissue invasion, nutrient acquisition, and host-defense evasion.
- Host-Pathogen Interaction: Candida parapsilosis is capable of inducing an inflammatory response in the host, resulting in the recruitment and activation of immune cells. However, immune responses that are excessive or dysregulated can also contribute to tissue injury and inflammation. The interaction between Candida parapsilosis and the host immune system is complex and variable based on the immune status and genetic factors of the host.
Risk factors of Candida parapsilosis infections
- Immunosuppression: Those with weakened immune systems are more susceptible to Candida parapsilosis infections. This includes individuals with HIV/AIDS, those undergoing chemotherapy or radiation therapy, recipients of organ transplants, and those with autoimmune diseases.
- Hospitalization: Candida parapsilosis infections are frequently associated with healthcare contexts, especially in patients who have been hospitalized or who have received medical care in intensive care units (ICUs), surgical wards, or long-term care facilities. Extended hospital stays and frequent use of invasive medical devices, including urinary catheters, central venous catheters, and ventilators, increase the risk of infection.
- Premature Infants: Infections with Candida parapsilosis are more prevalent in premature neonates, especially those admitted to neonatal intensive care units (NICUs). Premature infants are susceptible to Candida infections as a result of their immature immune systems, protracted hospitalization, and frequent exposure to invasive procedures and antibiotics.
- Prior Antifungal Therapy: Prior Antifungal Therapy: Prolonged or inappropriate use of broad-spectrum antibiotics or antifungal agents can disrupt the body’s normal microbial balance, allowing Candida parapsilosis to overgrow and cause an infection. Additionally, Candida parapsilosis can develop resistance to particular antifungal medications, making treatment more difficult.
- Parenteral Nutrition: Long-term parenteral nutrition (intravenous nourishment) increases the risk of Candida parapsilosis bloodstream infections in patients. The use of intravenous catheters for the delivery of nutrition presents a potential entry point for Candida into the circulation.
- Diabetes: Uncontrolled diabetes, particularly when blood sugar levels are inadequately managed, weakens the immune system and increases the risk of fungal infections, such as Candida parapsilosis.
- Invasive Procedures: Invasive procedures, such as surgery, the placement of an indwelling catheter, and invasive diagnostic tests, can introduce Candida parapsilosis into the body and create infection risk.
- Skin Barrier Disruption: Skin conditions, such as burns, surgical wounds, or dermatitis, that compromise the integrity of the skin can provide an entry site for Candida parapsilosis and increase the risk of infection.
Transmission of Candida parapsilosis
Candida parapsilosis is transmissible via a variety of routes, but it is predominantly regarded as an endogenous organism, which is part of the normal flora on the skin and mucous membranes of healthy people. However, Candida parapsilosis can be transmitted from person to person or indirectly through environmental sources under certain conditions. Uncertainty surrounds the precise modes of transmission for Candida parapsilosis, which may include the following:
- Person-to-Person Transmission: Candida parapsilosis can potentially be transmitted through direct contact between individuals. This can occur via intimate physical contact or contact with contaminated surfaces or hands. There may be an increased risk of person-to-person transmission among healthcare personnel, patients, and individuals residing in close quarters, such as in nursing homes or hospitals.
- Healthcare-Associated Transmission: Infections caused by Candida parapsilosis can proliferate in healthcare settings, especially intensive care units (ICUs), surgical wards, and neonatal intensive care units (NICUs). The transmission of Candida parapsilosis between patients may be facilitated by the use of contaminated medical devices, such as central venous catheters, urinary catheters, or endotracheal tubing. These devices can contribute to the spread of the fungus if they are improperly handled or inadequately disinfected.
- Environmental Contamination: Candida parapsilosis is capable of surviving in the environment, including on surfaces and medical equipment. Bed linens, apparel, furniture, and medical devices can serve as potential sources of transmission when contaminated. Fomites, such as contaminated mitts or clothing worn by healthcare workers, may also contribute to the propagation of the fungus.
- Vertical Transmission: There have been reports of Candida parapsilosis being transmitted vertically from mother to neonate during childbirth. The fungus is capable of colonizing the birth canal and transmitting itself to the neonate during delivery. This transmission mode is more prevalent in neonatal intensive care units.
It is essential to observe that while transmission of Candida parapsilosis is possible, it does not always result in infection. Frequently, the presence of risk factors, such as weakened immune systems or invasive medical procedures, is required for the emergence of an infection.
Implementing appropriate infection control measures, including proper hand hygiene, cleansing and disinfection of environmental surfaces, adherence to aseptic techniques during invasive procedures, and careful handling of medical devices, is necessary to prevent the transmission of Candida parapsilosis. In many healthcare facilities, protocols are in place to prevent the spread of infections, including Candida parapsilosis.
Virulence factors of Candida parapsilosis
Several virulence factors in Candida parapsilosis contribute to its ability to induce infections. These virulence factors allow the fungus to elude immune responses from the host, adhere to host tissues, and cause tissue damage. Among the most important virulence factors associated with Candida parapsilosis are the following:
- Adhesion Proteins: Candida parapsilosis produces adhesion proteins that facilitate its attachment to host cells and surfaces. These proteins allow the fungus to adhere to diverse tissues, such as epithelial cells, endothelial cells, and medical devices such as catheters. Adhesion is a crucial first stage in the establishment of an infection. C. parapsilosis produces numerous adhesins that enable it to adhere to host cells. These adhesins consist of:
- Galactose-specific lectins: Galactose-specific lectins bind to galactose residues on the surface of host cells.
- Fibronectin-binding proteins: These proteins bind to the extracellular matrix protein fibronectin.
- Laminin-binding proteins: These proteins bind to the extracellular matrix protein laminin.
- Biofilm Formation: Candida parapsilosis is capable of forming biofilms, which are structured communities of fungal cells surrounded by a protective matrix. Biofilms contribute significantly to the pathogenesis of Candida infections by increasing the fungus’ resistance to host immune defenses and antifungal medications. Biofilms can form on medical devices, such as catheters, resulting in difficult-to-eradicate infections.
- Secreted Enzymes: Candida parapsilosis secretes a variety of enzymes that contribute to its pathogenesis. Included in this category are phospholipases, proteases, and hemolysins. Phospholipases degrade the membranes of host cells, thereby facilitating the invasion of host tissues. Proteases can degrade host proteins, thereby interfering with the host’s defense mechanisms. Hemolysins can harm red blood cells as well as other host cells.
- Proteases: C. parapsilosis generates a variety of proteases capable of degrading host cell proteins. These proteases can aid the pathogen in invading host tissues and evading the immune system of the host.
- Phospholipases: C. parapsilosis produces a variety of phospholipases that can degrade the membranes of host cells. These phospholipases can aid the pathogen in invading host tissues and evading the immune system of the host.
- Morphological Switching: Candida parapsilosis is capable of undergoing morphological switching between various cellular forms, including yeast, pseudohyphae, and true hyphae. This morphological flexibility permits the fungus to adapt to various host environments and facilitates tissue invasion. Specifically, hyaline strains of Candida parapsilosis are associated with increased pathogenicity.
- Antifungal Resistance: Candida parapsilosis has demonstrated a propensity to develop resistance to antifungal medications. This resistance may be innate or acquired via genetic mutations. Candida parapsilosis infections are difficult to treat due to the fact that antifungal resistance reduces the efficacy of commonly used antifungal agents.
- Toxins: C. parapsilosis produces a variety of cytotoxic substances that can harm host cells. These toxins consist of:
- Candidalysin: Candidalysin is a pore-forming toxin that can disrupt the membranes of host cells.
- Enolase: Enolase is an enzyme that can cause DNA damage to host cells.
- Mannan-binding lectin (MBL): MBL is a protein capable of binding to mannan, a sugar found on the surface of C. parapsilosis cells. MBL is capable of activating the complement system, resulting in the lysis of C. parapsilosis cells.
Clinical Features of Candida parapsilosis
- Candidemia: Candidemia refers to the presence of Candida species in the circulatory system. It is among the most notable clinical manifestations of Candida parapsilosis infections. Candidaemia can manifest with fever, chills, hypotension, and other symptoms of a systemic infection. Endocarditis, septicemia, and disseminated infections affecting multiple organs can result from candidemia.
- Catheter-Related Infections: Candida parapsilosis preferentially colonises intravascular catheters, urinary catheters, and intravenous lines. Infections associated with these devices may manifest as localised inflammation at the insertion site, catheter-related systemic infections, or biofilm formation on the catheter surface.
- Surgical Site Infections: Candida parapsilosis can cause surgical site infections, especially in patients who have undergone invasive surgical procedures or have in-dwelling surgical devices. In the case of gastrointestinal surgeries, these infections can manifest as wound infections, abscesses, or anastomotic leakage.
- Skin and Soft Tissue Infections: Infections of the Skin and Soft Tissues Candida parapsilosis is capable of causing localised infections of the skin and soft tissues. These infections frequently occur in damp and moist-prone areas, such as the groyne, axilla, and spaces between the fingers. Symptoms include erythema, pruritus, papules, pustules, and satellite lesion formation.
- Mucosal Infections: Candida parapsilosis is capable of causing mucosal infections, most commonly effecting the oral cavity (also known as oral thrush) and the genital area. Oral thrush manifests as painful, creamy white patches on the tongue, palate, and inner cheekbones, which can impede feeding and swallowing. Infections of the genital area can cause vulvovaginitis in women, which is characterised by irritation, burning, and abnormal vaginal discharge.
- Gut infections: C. parapsilosis can induce a gastrointestinal infection known as diarrhoea. Diarrhoea is characterised by faeces that are loose and watery.
- Infections of the bloodstream: C. parapsilosis can induce a bloodstream infection known as fungemia. Fungemia is marked by fever, shivers, and exhaustion.
Lab Diagnosis of Candida parapsilosis
- Microscopic Examination: Clinical specimens, such as blood, tissue, or body fluid samples, can be subjected to microscopic examination using techniques such as Gramme staining or potassium hydroxide (KOH) moist mount preparation. Under a microscope, Candida parapsilosis appears as sprouting yeast cells or pseudohyphae.
- Culture: The primary technique for isolating and identifying Candida species, including Candida parapsilosis, is through culture. Blood, urine, wound samples, and respiratory secretions can be inoculated onto culture media such as Sabouraud dextrose agar (SDA) or chromogenic agar. On these media, Candida parapsilosis typically grows as pearly white colonies.
- Blood cultures: Blood cultures are the most prevalent method for diagnosing C. parapsilosis bloodstream infections. By inserting a needle into a vein and withdrawing a small quantity of blood, blood cultures are obtained. The blood is then added to a culture medium that encourages the growth of fungi. C. parapsilosis will proliferate in the culture medium if it is present in the blood.
- Swab cultures: Swab cultures can be used to diagnose infections of the epidermis, mouth, and mucous membranes caused by C. parapsilosis. To acquire swab cultures, a sterile swab is rubbed over the affected area. The swab is then deposited in a culture medium designed to promote the growth of fungi. C. parapsilosis will proliferate in the culture medium if it is present on the swab.
- Urine cultures: Urine cultures can be used to diagnose urinary tract infections caused by C. parapsilosis. Urine cultures are obtained by obtaining a sample of midstream urine. The urine sample is then deposited in a culture medium that promotes fungal growth. C. parapsilosis will proliferate in the culture medium if it is present in the urine.
- Biochemical assays: Candida parapsilosis can be distinguished from other Candida species using a variety of biochemical assays. These assays evaluate the enzymatic or metabolic properties of the fungus. For instance, assimilation assays utilising sugar or carbon sources, such as the API 20C AUX system, can provide species-specific profiles for the identification of Candida parapsilosis.
- Molecular Methods: For the swift and specific detection of Candida parapsilosis, molecular techniques such as polymerase chain reaction (PCR) can be utilised. In clinical samples, Candida parapsilosis DNA can be amplified and identified by PCR assays targeting specific gene sequences, such as the internal transcribed spacer (ITS) region.
- Antifungal Susceptibility Testing: Antifungal susceptibility testing is necessary to determine Candida parapsilosis’s susceptibility to various antifungal agents. It facilitates appropriate antifungal treatment. The most prevalent method for determining antifungal susceptibility is broth microdilution, which assesses the minimum inhibitory concentration (MIC) of antifungal drugs against the fungus.
Treatment of Candida parapsilosis infections
- Antifungal Medications: Azole antifungals, such as fluconazole, voriconazole, and itraconazole, are the most frequently prescribed antifungals for Candida parapsilosis infections. By targeting the synthesis of fungal cell membranes, these medications inhibit the growth of fungi. Due to its efficacy and safety profile, fluconazole is frequently the drug of choice for treating Candida parapsilosis infections. However, azole antifungal resistance is possible, and susceptibility testing should be conducted to determine the most appropriate treatment.
- Echinocandins: Echinocandins, which include caspofungin, micafungin, and anidulafungin, are an additional class of antifungal agents used to treat Candida parapsilosis infections. They prevent the formation of fungal cell walls, resulting in cell demise. Echinocandins are typically reserved for the treatment of severe or resistant infections or when azole resistance is suspected. They are especially effective against biofilms of Candida parapsilosis.
- Amphotericin B: Amphotericin B, a polyene antifungal agent, may be considered for the treatment of severe Candida parapsilosis infections or when other antifungals have failed. To reduce toxicity, it can be administered as a lipid formulation, such as liposomal amphotericin B. Amphotericin B binds to the membranes of fungal cells, causing cell permeability and mortality.
- Combination Therapy: Combination antifungal therapy may be considered in certain instances, particularly for critically ill patients or those with complicated infections. Combining antifungal agents from distinct classes, such as an azole with an echinocandin or amphotericin B, can improve efficacy and reduce the risk of antifungal resistance.
- Removal of Infected Devices: In cases of catheter-associated Candida parapsilosis infections or infections associated with other indwelling medical devices, the removal or replacement of the infected device may be required for effective treatment. This is especially crucial when the infection persists despite antifungal treatment.
Prevention and control of Candida parapsilosis
- Hand Hygiene: Proper hand sanitation is essential for preventing the spread of Candida parapsilosis. Before and after patient contact, healthcare professionals should wash their hands with soap and water or use alcohol-based hand sanitizers, as well as adhere to strict hand sanitation protocols.
- Infection Control Practises: It is essential for healthcare facilities to implement standard infection control practises. This includes the use of personal protective equipment (such as gloves, gowns, and hoods) and adherence to infection control guidelines for invasive procedures, wound care, and catheter insertion and maintenance.
- Environmental Cleaning: In order to reduce the environmental reservoir of Candida parapsilosis, it is essential that patient care areas, medical equipment, and surfaces in healthcare settings are regularly and thoroughly cleaned and disinfected. The use of appropriate disinfectants with antifungal activity is advised.
- Catheter Care: Proper care and maintenance of indwelling medical devices, such as central venous catheters and urinary catheters, can aid in the prevention of Candida parapsilosis infections. Catheters should be inserted and maintained using strict aseptic techniques, and they should be removed as soon as they are no longer required.
- Antifungal Stewardship: Rational use of antifungal agents is essential for preventing the emergence of drug resistance and decreasing the risk of Candida parapsilosis infections associated with healthcare settings. Antifungal stewardship programmes encourage the proper use of antifungals, including the selection of the most effective agent, the optimisation of dosage, and the monitoring of adverse effects.
- Education of Patients and Carers: Educating patients and their carers about the risk factors for Candida parapsilosis infections and the significance of preventive measures can aid in reducing the incidence of infections. This includes practising proper hygiene, adhering to prescribed medications, and recognising signs of infection in order to receive prompt medical care.
- Surveillance and Outbreak Investigation: Active surveillance for Candida parapsilosis infections in healthcare settings can aid in the identification of trends, clusters, and outbreaks. Identifying and investigating cases in a timely manner can facilitate prompt intervention and the implementation of control measures to prevent further spread.
FAQ
What is Candida parapsilosis?
Candida parapsilosis is a species of yeast that can cause infections in humans, particularly in healthcare settings. It is considered an emerging fungal pathogen.
What are the risk factors for Candida parapsilosis infections?
Risk factors for Candida parapsilosis infections include prolonged hospitalization, use of broad-spectrum antibiotics, indwelling medical devices (e.g., central venous catheters), immunosuppression, invasive procedures, and prolonged stay in the intensive care unit.
How is Candida parapsilosis diagnosed?
Diagnosis of Candida parapsilosis infections involves laboratory tests such as microscopic examination, culture of clinical specimens, biochemical tests, and molecular methods. Antifungal susceptibility testing may also be performed to guide appropriate treatment.
What are the common infections caused by Candida parapsilosis?
Candida parapsilosis can cause various infections, including bloodstream infections (candidemia), catheter-related infections, surgical site infections, urinary tract infections, and infections in neonates and premature infants.
What is the treatment for Candida parapsilosis infections?
Treatment of Candida parapsilosis infections typically involves antifungal therapy with agents such as fluconazole, echinocandins (e.g., caspofungin), or amphotericin B. The choice of antifungal and duration of treatment depend on the site and severity of infection.
Can Candida parapsilosis infections be prevented?
Yes, Candida parapsilosis infections can be prevented through measures such as proper hand hygiene, adherence to infection control practices, environmental cleaning, appropriate catheter care, antifungal stewardship, patient education, and surveillance for early detection.
Is Candida parapsilosis resistant to antifungal drugs?
Candida parapsilosis is generally susceptible to commonly used antifungal drugs such as fluconazole and echinocandins. However, resistance to azole antifungals can occur, and susceptibility testing is recommended to guide appropriate therapy.
Can Candida parapsilosis infections recur?
Yes, Candida parapsilosis infections can recur, especially in individuals with underlying conditions or compromised immune systems. Proper management, including identification and addressing of risk factors, is important to prevent recurrent infections.
Are Candida parapsilosis infections contagious?
Candida parapsilosis infections are typically not contagious from person to person. However, in healthcare settings, the fungus can spread through contaminated hands, medical equipment, or environmental surfaces.
Are there any emerging trends or research on Candida parapsilosis?
Ongoing research focuses on understanding the genetic diversity, virulence factors, antifungal resistance mechanisms, and epidemiology of Candida parapsilosis. Additionally, studies on the development of new diagnostic methods and therapeutic strategies are also being conducted.
References
- Trofa D, Gácser A, Nosanchuk JD. Candida parapsilosis, an emerging fungal pathogen. Clin Microbiol Rev. 2008;21(4):606-625. doi:10.1128/CMR.00013-08
- Tavanti A, Davidson AD, Fordyce MJ, et al. Population structure and properties of Candida parapsilosis, as revealed by multilocus sequence typing. J Clin Microbiol. 2005;43(2):559-568. doi:10.1128/JCM.43.2.559-568.2005
- Arendrup MC, Boekhout T, Akova M, et al. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of rare invasive yeast infections. Clin Microbiol Infect. 2014;20 Suppl 3:76-98. doi:10.1111/1469-0691.12539
- Chow JK, Golan Y, Ruthazer R, et al. Factors associated with candidemia caused by non-albicans Candida species versus Candida albicans in the intensive care unit. Clin Infect Dis. 2008;46(8):1206-1213. doi:10.1086/529435
- Pfaller MA, Diekema DJ, Gibbs DL, et al. Results from the ARTEMIS DISK Global Antifungal Surveillance Study, 1997 to 2007: a 10.5-year analysis of susceptibilities of Candida species to fluconazole and voriconazole as determined by CLSI standardized disk diffusion. J Clin Microbiol. 2010;48(4):1366-1377. doi:10.1128/JCM.02464-09
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.