What is Candida albicans?
| Kingdom: | Fungi |
| Division: | Ascomycota |
| Class: | Saccharomycetes |
| Order: | Saccharomycetales |
| Family: | Saccharomycetaceae |
| Genus: | Candida |
| Species: | C. albicans |
- Candida albicans, an opportunistic pathogenic yeast, is a prevalent component of the human gut flora. Besides being present within the human body, it can also thrive externally.
- Studies have shown that 40-60% of healthy adults have Candida albicans present in their gastrointestinal tract and mouth. Typically, it exists as a harmless commensal organism. However, under certain conditions, especially in individuals with compromised immune systems, it can become pathogenic.
- Therefore, it is one of the few species within the Candida genus known to cause candidiasis, a condition arising from an overgrowth of the fungus. This infection is frequently observed in patients with HIV.
- Furthermore, C. albicans is the predominant fungal species found in biofilms, which can form on implanted medical devices or human tissue.
- Along with C. tropicalis, C. parapsilosis, and C. glabrata, C. albicans accounts for 50-90% of all human candidiasis cases. Alarmingly, a 40% mortality rate has been associated with systemic candidiasis caused by C. albicans.
- In the US alone, invasive candidiasis acquired in hospitals results in an estimated 2,800 to 11,200 deaths annually. Then, recent studies have brought to light that C. albicans might be able to cross the blood-brain barrier in mice, suggesting that the actual impact of this organism might be even more significant.
- In the realm of scientific research, C. albicans serves as a model organism for studying fungal pathogens. It exhibits dimorphism, meaning it can grow as both yeast and filamentous cells. Besides these forms, it also presents various other morphological phenotypes.
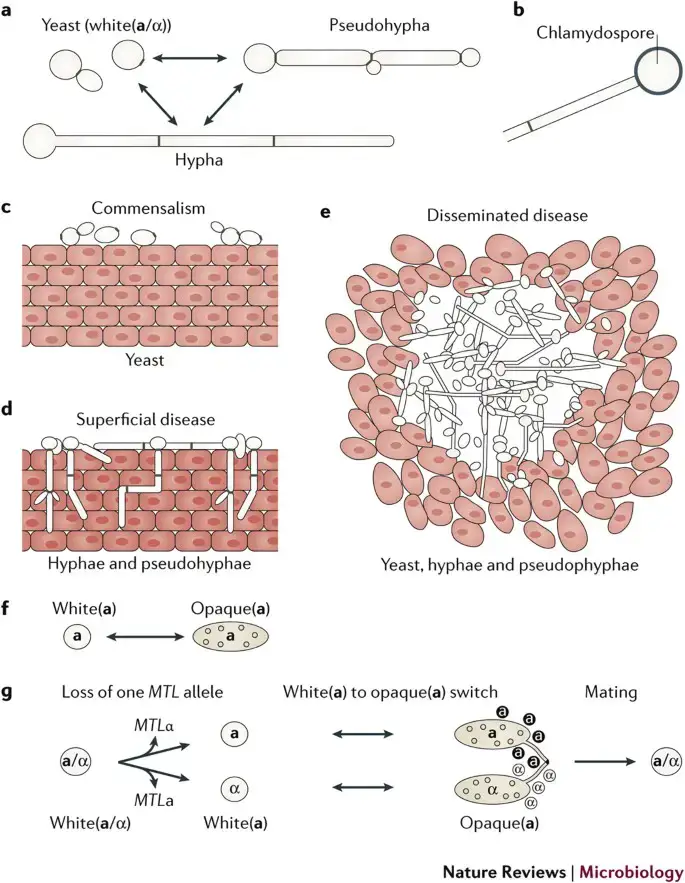
- For many years, it was believed that C. albicans was strictly diploid. However, it has been discovered that it can exist in both haploid and tetraploid stages. The diploid genome of this organism is roughly 29 Mb in size, with a significant portion of its protein-coding genes yet to be characterized.
- For research purposes, C. albicans can be easily cultured in laboratories and studied both in vivo and in vitro. The choice of media can influence its morphological state, with CHROMagar Candida being a specialized medium used to identify different Candida species.
- The name “Candida albicans” is derived from Latin, with “Candida” meaning white and “albicans” translating to becoming white, making the name somewhat redundant. Commonly, it is referred to as thrush, candidiasis, or simply candida.
- The Candida genus encompasses over 200 species, with C. albicans being one of the most studied. Historical references to thrush, likely caused by C. albicans, can be traced back to 400 BCE in the writings of Hippocrates.
Habitat of Candida albicans
Candida albicans is a form of yeast commonly found as part of the human body’s normal microbial flora. It is known to inhabit various body segments, particularly mucous membranes and moist regions. Here are some of Candida albicans’ common habitats:
- Mouth and throat: Candida albicans can be found in the oral cavity, which includes the tongue, gums, and back of the pharynx. It is a common cause of oral thrush, particularly in infants, people with weakened immune systems, and those taking antibiotics or corticosteroids.
- Genital area: Both males and females can be colonized by Candida albicans in the genital area. It can cause vaginal yeast infections in women, manifested by symptoms including itching, burning, and aberrant discharge. It can cause balanitis, an inflammation of the penis’s head, in males.
- Gastrointestinal tract: Candida albicans can be found in the digestive tract, particularly in the small intestine and rectum. Generally, the immune system and the presence of beneficial bacteria keep it in control. Certain factors, such as a weakened immune system or protracted use of antibiotics, can however disrupt this equilibrium, leading to an overgrowth of Candida and conditions such as candidiasis or candida overgrowth syndrome.
- Skin and nails: Candida albicans is also able to colonize the epidermis and nails. It can cause infections such as cutaneous candidiasis, which typically manifest in warm, moist areas of the body such as armpits, groin, and skin fissures. Infections of the nails (onychomycosis) can also result in thickened, discolored, and fragile nails.
Morphology of Candida albicans
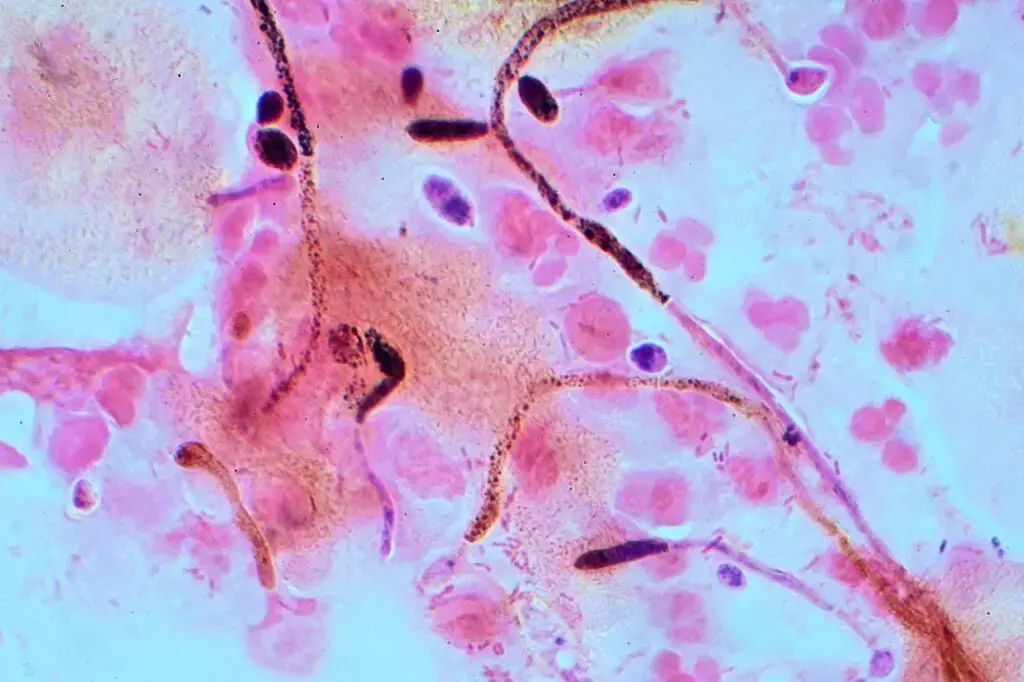
Candida albicans is a dimorphic fungus capable of growing in both yeast and hyphae forms. Yeast cells are round or oval in shape and range in diameter from 5 to 10 micrometers. Hyphae are long, thread-like structures with a maximum length of several centimeters.
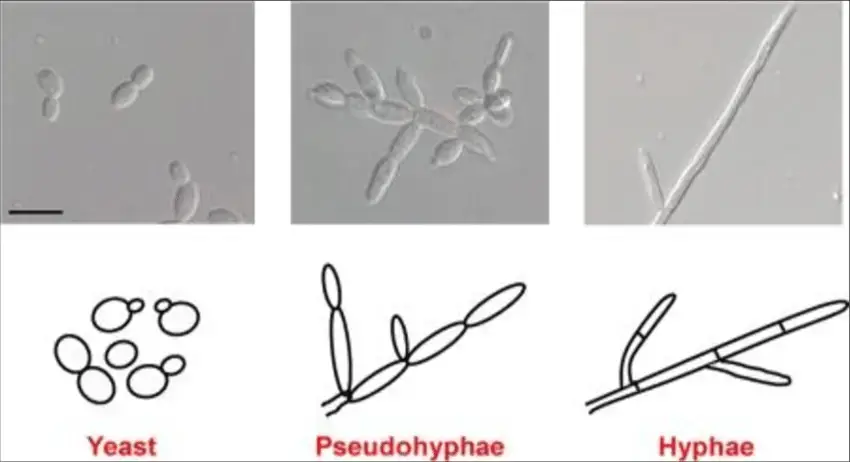
Candida albicans is a dimorphic fungus, indicating that, depending on its environment, it can exist in two distinct forms. Here is an overview of Candida albicans’ morphology:
- Yeast form: Candida albicans, in its yeast form, appears as single-celled, ovoid to spherical structures known as yeast cells. Typically, the size of these cells ranges from 2 to 10 micrometers. They reproduce via budding, in which a smaller progeny cell forms on the surface of the parent cell.
- Round or oval in shape
- 5-10 micrometers in diameter
- Reproduced by budding
- Pseudohyphae: Candida albicans can endure a morphological change from yeast to pseudohyphae under certain circumstances, such as nutrient limitation or contact with a surface. Pseudohyphae are elongated structures composed of linked yeast cells. The chain’s cells remain connected but are elongated, giving the impression of a filamentous structure.
- Hyphae: Candida albicans can also develop genuine hyphae, which are long, branching filamentous structures, in addition to pseudohyphae. Hyphae are typically observed when environmental conditions are favorable, such as when specific nutrients are present or when fungal cells encounter an appropriate surface for attachment. The hyphal form of Candida albicans allows for tissue penetration and invasion.
- Long, thread-like structures
- Can grow up to several centimeters in length
- Formed when yeast cells elongate and form a long, narrow filament
- Can branch and form a network of interconnected filaments
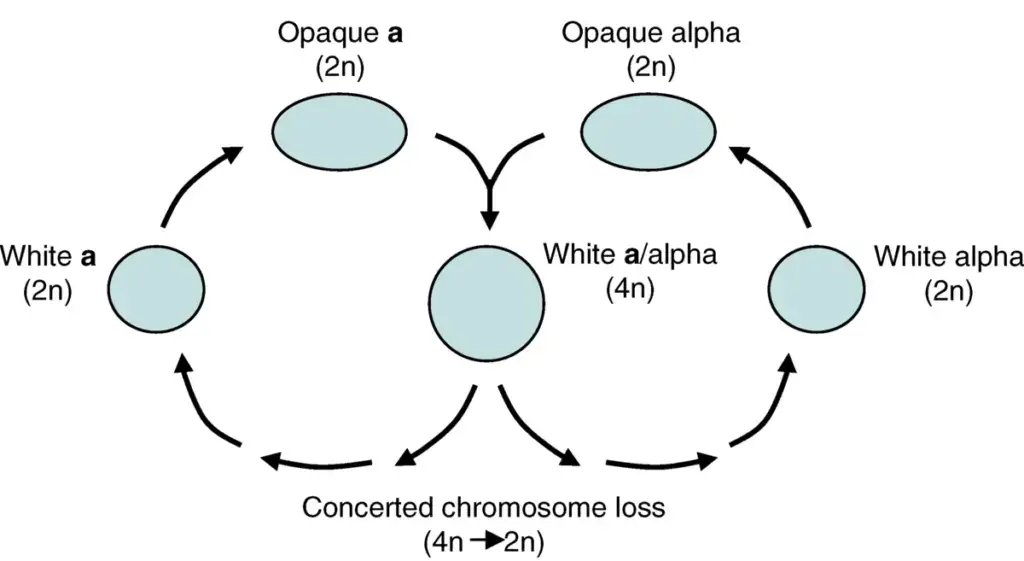
Important to Candida albicans’ pathogenicity is its ability to switch between various morphological forms. The transformation from yeast to filamentous forms permits the fungus to adhere to and invade host tissues, thereby enhancing its capacity to cause infections.
Cultural Characteristics of Candida albicans
As a yeast, Candida albicans exhibits certain cultural characteristics when cultivated in the laboratory. Here are the cultural characteristics that are typical of Candida albicans:
- Growth on solid media: Candida albicans can thrive on a variety of solid media, including Sabouraud dextrose agar (SDA) and Chromagar Candida, both of which are commonly used in laboratories. On SDA, Candida albicans colonies appear as homogeneous, white or cream-colored colonies. The colonies are typically spherical and may have slightly wrinkled or filamentous borders.
- Colony morphology: Candida albicans colonies on solid media can differ in size and texture in terms of colony morphology. Young colonies are typically tiny and smooth, gradually growing larger and acquiring a surface that is slightly wrinkled or folded. As colonies age, they may take on a creamy or light beige hue. The texture can range from delicate and moist to powdery.
- Formation of pseudohyphae: Candida albicans is capable of producing pseudohyphae, or chains of elongated yeast cells. This trait is observable when Candida albicans is grown on suitable media or under particular conditions. The formation of pseudohyphae can lend colonies a filamentous or string-like appearance.
- Germ tube formation: Candida albicans has the ability to form germ tubes under specific incubation conditions, which is one of its distinguishing characteristics. Germ tubes are protrusions that extend from the yeast cells. This characteristic is frequently used as a laboratory diagnostic test to identify Candida albicans.

Culture Media used for the growth of Candida albicans and growth conditions
Candida albicans requires specific growth conditions to thrive on different culture plates. Here are the general growth conditions required for Candida albicans on various culture plates commonly used in laboratories:

- Sabouraud Dextrose Agar (SDA): SDA is a commonly used culture medium for Candida albicans. The growth conditions for Candida albicans on SDA typically include:
- Temperature: Candida albicans grows well at a temperature of approximately 30 to 37 degrees Celsius, which corresponds to human body temperature.
- pH: SDA is usually adjusted to a slightly acidic pH range of 5.6 to 6.8, which is conducive for Candida albicans growth.
- Nutrients: SDA contains a carbon source (dextrose) and peptones that provide essential nutrients for the yeast to grow.
- Chromagar Candida: Chromagar Candida is a selective and differential culture medium designed specifically for the identification of Candida species. The growth conditions for Candida albicans on Chromagar Candida are similar to those on SDA:
- Temperature: Candida albicans grows well at a temperature of approximately 30 to 37 degrees Celsius.
- pH: The pH of Chromagar Candida is typically adjusted to a slightly acidic range of 5.6 to 6.8.
- Nutrients: The medium contains specific nutrients that support the growth of Candida species while inhibiting the growth of other microorganisms.
- Blood Agar: Blood agar is a nutrient-rich medium often used to support the growth of various microorganisms, including Candida albicans. The growth conditions for Candida albicans on blood agar include:
- Temperature: Candida albicans grows well at a temperature of approximately 30 to 37 degrees Celsius.
- pH: Blood agar is typically prepared with a neutral pH, around 7.2 to 7.4.
- Nutrients: Blood agar provides a rich source of nutrients for the yeast to grow, including amino acids, vitamins, and minerals.
Life Cycle of Candida albicans
The life cycle of Candida albicans is intricate and comprises numerous stages. The yeast form of C. albicans is the most prevalent form. Yeast cells are round or oval in shape and range in diameter from 5 to 10 micrometers. They reproduce through budding, a process in which a small bud forms on the cell’s surface and then separates to create a new cell.
Under specific circumstances, yeast cells can form hyphae. Hyphae are long, thread-like structures with a maximum length of several centimeters. When yeast cells elongate and form a long, thin filament, these are produced. Hyphae are capable of branching and forming a network of filamentous connections.
Hyphae are more likely to cause an infection and are more invasive than yeast cells. They are also capable of forming biofilms, a type of protective membrane that makes it difficult for the immune system to combat the infection.
The C. albicans life cycle can be divided into the following stages:
- Asexual reproduction: Yeast cells reproduce asexually through budding. On the surface of the cell, a small bud forms and then separates to create a new cell.
- Sexual reproduction: Candida albicans is capable of sexual reproduction. This method entails the fusion of two haploid cells into a diploid cell. Following meiosis, the diploid cell divides into four haploid cells.
- Germination: When yeast cells are incubated at 37°C in a nutrient-rich environment, long, slender projections known as germ tubes develop. C. albicans uses germ filaments to invade host tissues.
- Invasion: Once C. albicans has invaded host tissues, it is capable of causing infection. The infection could be localized or widespread.
- Spread: C. albicans can be transmitted from one individual to another via contact with infected skin or mucous membranes. Additionally, it can be transmitted through contact with contaminated objects, such as linens and bedding.
- Death: C. albicans can be eliminated by the immune system or antifungal medications.
Understanding how C. albicans causes disease requires an understanding of the fungus’ life cycle. By comprehending the life cycle of fungi, scientists can create more effective treatments for fungal infections.
Virulence Factors of Candida albicans
Multiple virulence factors in Candida albicans contribute to its capacity to cause infections and evade the host immune system. Here are some of Candida albicans’ main virulence factors:
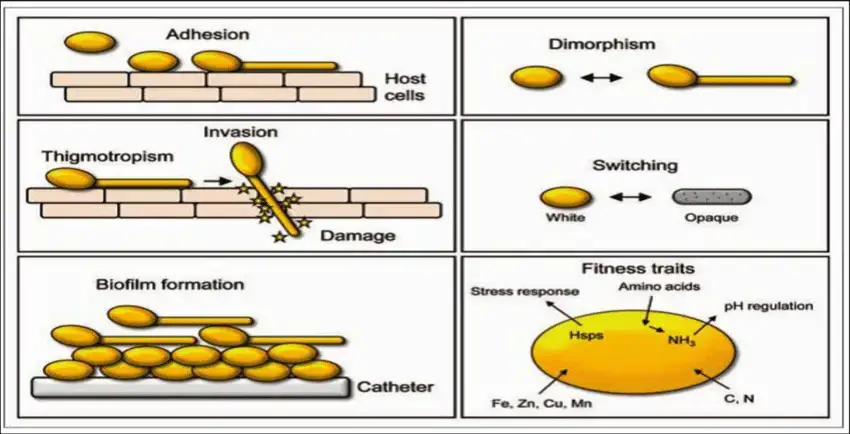
- Adhesion factors: Candida albicans expresses adhesins, surface proteins that permit the fungus to adhere to host tissues. Adhesion factors enable Candida albicans to adhere to host cells and form biofilms, thereby facilitating colonization and persistence at diverse sites.
- Invasion: Once C. albicans adheres to host cells, it is able to invade tissues by secreting enzymes that degrade the host cell membrane.
- Biofilm formation: Candida albicans is capable of forming biofilms, which are complex communities of cells surrounded by an extracellular matrix. Biofilms offer protection against host immune responses and enhance antifungal agent resistance, making them difficult to eradicate. Biofilms are frequently associated with infections caused by medical devices, such as catheter-associated infections.
- Phenotypic switching: Candida albicans is capable of phenotypic switching, which is the ability to transition between various forms, including the yeast form, pseudohyphal form, and hyphal form. This phenotypic plasticity enables Candida albicans to adapt to various environments, invade host tissues, and elude the host immune system.
- Secreted hydrolytic enzymes: Candida albicans secretes an assortment of hydrolytic enzymes, including proteases, phospholipases, and hemolysins. These enzymes facilitate nutrient acquisition from the host and contribute to tissue invasion.
- Evasion of immune response: Candida albicans possesses mechanisms for evading or modulating the immune response of the host. It can manipulate host immune cells, such as neutrophils and macrophages, reducing their ability to eradicate the fungus effectively. Additionally, Candida albicans can generate factors that interfere with the complement system, a crucial component of the innate immune response.
- Antifungal resistance: Candida albicans can develop resistance to antifungal medications, which makes treatment difficult. Multiple mechanisms, including alterations in drug target sites, overexpression of drug efflux pumps, and changes in cell wall composition, are attributed to the development of resistance.
Pathogenesis of Candida albicans/How does Candida albicans Infect?
Candida albicans infections typically involve multiple phases, from initial colonization to the development of invasive disease. The general phases of Candida albicans infection are as follows:
- Adhesion and colonization: Candida albicans adheres to and colonizes host tissues or mucosal surfaces, including the oral cavity, gastrointestinal tract, and genital tract. The expression of specific adhesins facilitates adhesion, allowing the fungus to bind to host cells or extracellular matrix components.
- Invasion and tissue damage: Once Candida albicans has effectively adhered and colonized, it can invade and damage host tissues. The formation of invasive hyphae allows the fungus to penetrate and injure the epithelial barriers. The invasion process entails the secretion of tissue-damaging hydrolytic enzymes, such as proteases and phospholipases.
- Evasion of host immune response: Candida albicans possesses numerous mechanisms to evade or modulate the immune response of its host. It is resistant to phagocytosis by immune cells and impairs neutrophil and macrophage killing mechanisms. The fungus can also manipulate the immune signaling pathways of the host, preventing the infection from being effectively eliminated.
- Dissemination: In some instances, Candida albicans can spread via the bloodstream from the initial site of infection to other organs or tissues. This can result in systemic candidiasis, a severe and potentially fatal condition. Individuals with weakened immune systems, such as those with immunodeficiency disorders or those enduring immunosuppressive treatments, are typically the carriers of infectious diseases.
- Host response and inflammation: Inflammation and host response: When Candida albicans invades host tissues, the immune system triggers an inflammatory response. This response is characterized by the recruitment and activation of immune cells, the release of cytokines and chemokines, and the induction of an immune-inflammatory cascade. Both protective immunity and tissue injury can result from the host’s response.
- Resolution or persistent infection: Candida albicans infections can result in either a resolution or a persistent infection. In certain instances, the immune response of the host is effective at eliminating the infection, resulting in resolution and recovery. In other instances, the infection may persist, particularly in those with compromised immune systems, resulting in chronic or recurrent infections.
Types of Candidiasis
Candidiasis is a collection of fungal infections induced by Candida species, most frequently Candida albicans. The following are some varieties of candidiasis:
- Oropharyngeal Candidiasis (Thrush): This form of candidiasis affects both the mouth and the throat. Infants, individuals with compromised immune systems, such as those with HIV/AIDS, and individuals taking certain medications, such as corticosteroids or antibiotics, are frequently affected. In addition to discomfort or pain when swallowing, symptoms may include white patches on the tongue, inner cheeks, or pharynx.
- Vulvovaginal Candidiasis: Vulvovaginal candidiasis affects the female genital region. It manifests as itching, irritation, and a viscous, white vaginal discharge. Vulvovaginal candidiasis is quite common, and factors such as hormonal fluctuations, pregnancy, antibiotic use, and immune system impairment can increase the risk of developing this infection.
- Cutaneous Candidiasis: Cutaneous candidiasis refers to fungal cutaneous infections. It is commonly found in warm, moist areas of the body, such as the armpits, groin, and skin fissures. Symptoms include a rash that is scarlet, itchy, and surrounded by satellite lesions.
- Intertrigo: Intertrigo is a form of cutaneous candidiasis that manifests in skin folds, such as under the breasts, between the toenails, and in the groin. It is characterized by a red, raw, and sometimes moist dermatitis that is frequently accompanied by discomfort and itching.
- Candidemia: Candidemia is an infection of the bloodstream produced by Candida species. It is a serious condition that commonly affects hospitalized patients, especially those with compromised immune systems or who have undertaken invasive medical procedures. Candidemia can result in systemic candidiasis, in which the infection extends to multiple organs of the body, causing potentially fatal complications.
- Invasive Candidiasis: Invasive candidiasis refers to infections of the internal organs induced by Candida species. This condition is severe and potentially fatal, particularly for those with compromised immune systems. Those undergoing chemotherapy, organ transplantation, or residing in intensive care units are frequently affected. Candida invasive necessitates a prompt diagnosis and aggressive treatment.
Lab Diagnosis of Candida albicans
Identifying and confirming the presence of Candida albicans in the laboratory requires the use of multiple techniques. Here are some common laboratory techniques for diagnosing Candida albicans:
- Microscopic examination: A preliminary step in diagnosing Candida albicans is the microscopic examination of clinical samples. A wet mount or Gram stain can disclose the presence of yeast cells or hyphae characteristic of Candida species in the sample. Direct microscopy enables a rapid initial evaluation of the infection.
- Culture: Standard procedure for the isolation and identification of Candida albicans is the cultivation of clinical specimens on appropriate culture media. SDA is frequently used as a principal culture medium. After 24 to 48 hours of incubation at 30 to 37 degrees Celsius, Candida albicans typically forms uniform, creamy-to-white colonies on SDA. Subculturing and additional assays can be used to identify colonies further.
- Chromogenic agar: Chromogenic agar, such as CHROMagar Candida, can help identify Candida species, including Candida albicans. These specialized agar media contain chromogenic substrates that interact with particular enzymes produced by Candida species, resulting in color differentiation. On chromogenic agar, Candida albicans colonies may exhibit distinct colors or characteristics that distinguish them from other Candida species.
- Germ tube test: The germ tube test is a diagnostic test that is specific to Candida albicans. It entails incubating yeast cells in human or animal serum at 37 degrees Celsius for a specific amount of time (usually two to three hours). Microscopically, germ tubes, which are elongated projections emanating from yeast cells, are observed. Positive germ tube formation strongly suggests the presence of Candida albicans.
- Biochemical tests: Biochemical tests can provide additional assistance in identifying Candida albicans. These assays evaluate various metabolic properties of yeast. Using biochemical test systems such as the API 20C AUX or VITEK 2 yeast identification systems, for instance, the capacity to ferment or assimilate specific carbohydrates or the production of specific enzymes can be determined.
- Molecular methods: Molecular methods, such as polymerase chain reaction (PCR), can identify Candida albicans quickly and precisely. Assays based on polymerase chain reaction (PCR) can detect genetic markers or sequences unique to Candida albicans, allowing for the sensitive and accurate identification of the fungus.
Treatments of Candida albicans
The treatment of Candida albicans infections is dependent on the infection’s site and severity. Here are several common Candida albicans treatments:
- Antifungal medications: antifungal medications are the primary treatment for Candida albicans infections. The choice of antifungal agent depends on the infection’s location and severity. Typical antifungal medications include:
- Azoles: Azole antifungals, such as fluconazole, itraconazole, and voriconazole, are frequently prescribed for mucosal infections, including oropharyngeal and vulvovaginal candidiasis.
- Echinocandins: Echinocandins, including caspofungin, micafungin, and anidulafungin, are frequently prescribed for systemic and invasive Candida infections.
- Polyenes: Polyene antifungals, such as amphotericin B, are reserved for the treatment of severe systemic infections or when other antifungals have failed.
- The choice of antifungal medication and the duration of treatment may vary based on the patient’s unique circumstances and characteristics. It is essential to adhere to the prescribed treatment plan and finish the entire course of medication.
- Topical treatments: Localized cutaneous Candida infections, such as intertrigo or diaper dermatitis, may be treated topically with antifungal creams or ointments. Clotrimazole, miconazole, and nystatin are frequently used antifungal topical agents. These medications are typically applied directly to the afflicted area for a predetermined period of time.
- Management of underlying conditions: Successful treatment requires the management of underlying conditions that contribute to Candida albicans infections. This may involve addressing diabetes, immunodeficiency, or the discontinuation or adjustment of medications that impair the immune system or disturb the normal balance of microbial flora.
- Prevention and hygiene measures: For the prevention of recurrent Candida albicans infections, it is essential to maintain excellent hygiene practices. This includes keeping the affected areas clean and dry, avoiding tight-fitting apparel, and employing the proper hygiene products. Individuals susceptible to recurrent vulvovaginal candidiasis may be advised to wear cotton underwear, avoid irritants, and practice good genital hygiene.
Prevention and Control of Candida albicans
Candida albicans infection prevention and control focuses on reducing the risk of colonization and infection. Here are some methods for preventing and controlling Candida albicans:
- Good hygiene practices: In order to prevent Candida albicans infections, it is essential to maintain good sanitation. This includes routine handwashing with detergent and water, especially before and after handling potentially contaminated materials or surfaces.
- Keep the skin dry: Candida thrives in warm and moist environments, so keep the epidermis dry. Keeping the skin dry, particularly in sweat-prone areas or skin fissures, can help prevent Candida overgrowth. Consider using absorbent powders in areas prone to moisture accumulation, particularly after cleansing or perspiring.
- Avoid irritants: Irritants, such as harsh soaps, perfumed products, and tight-fitting clothing, can disturb the natural equilibrium of microorganisms on the skin and mucous membranes, making them more susceptible to Candida infections. Utilize gentle, fragrance-free products and loose-fitting, breathable fabrics for apparel.
- Manage underlying medical conditions: Certain medical conditions, such as diabetes, immunodeficiency disorders, and hormonal imbalances, can increase the risk of Candida albicans infections and should be managed. It is essential to effectively manage these underlying conditions in order to reduce the likelihood of infection.
- Use probiotics: Probiotics, such as lactobacilli, can assist in maintaining a healthy microbial balance in the body. They are especially useful in preventing and treating vulvovaginal candidiasis. Under the supervision of a healthcare professional, probiotics may be administered orally or as vaginal suppositories.
- Avoid unnecessary use of antibiotics: Antibiotics can disrupt the normal microbial flora, allowing Candida albicans to proliferate out of control. Avoid unnecessary or protracted use of antibiotics, and when necessary, always adhere to the prescribed dosage and duration.
- Education and awareness: Promoting education and awareness about Candida albicans infections can help individuals understand the risk factors, symptoms, and preventative measures. This includes providing information on personal hygiene, strategies for risk reduction, and pursuing prompt medical care for suspected infections.
- Environmental control: In healthcare contexts, infection control measures are essential for preventing the spread of Candida albicans through the environment. This includes cleansing and disinfecting surfaces, medical equipment, and healthcare facilities. Important factors include the observance of strict hand hygiene protocols and the use of appropriate personal protective equipment.
FAQ
What is Candida albicans?
Candida albicans is a type of yeast that is commonly found in the human body, particularly in the mouth, gastrointestinal tract, and genital areas. It can cause infections when it overgrows and disrupts the normal microbial balance.
What causes Candida albicans infections?
Candida albicans infections can be caused by factors such as weakened immune system, hormonal changes, antibiotic use, uncontrolled diabetes, pregnancy, or use of immunosuppressive medications. These factors can disrupt the natural balance of microorganisms and allow Candida to overgrow.
How are Candida albicans infections diagnosed?
Candida albicans infections can be diagnosed through various methods, including microscopic examination, culture of clinical samples, biochemical tests, and molecular methods. These tests help identify the presence of Candida albicans and determine the site and severity of infection.
What are the common symptoms of a Candida albicans infection?
Common symptoms of Candida albicans infection can vary depending on the site of infection. For example, oral thrush may cause creamy white patches in the mouth, while vulvovaginal candidiasis can cause itching, irritation, and a white discharge. Systemic infections may present with fever, chills, and organ-specific symptoms.
Can Candida albicans infections be prevented?
Candida albicans infections can be prevented by maintaining good hygiene practices, keeping the skin dry, avoiding irritants, managing underlying medical conditions, using probiotics, and practicing safe sex. It is also important to follow appropriate antibiotic use and infection control measures in healthcare settings.
Are Candida albicans infections contagious?
Candida albicans infections are generally not considered contagious in healthy individuals. However, some cases, such as oral thrush or genital yeast infections, can be transmitted through direct contact or intimate contact. In individuals with weakened immune systems, caution should be exercised to prevent transmission.
What is the treatment for Candida albicans infections?
Treatment for Candida albicans infections typically involves antifungal medications, such as azoles, echinocandins, or polyenes, depending on the site and severity of the infection. Topical treatments may be used for localized infections. Managing underlying conditions and practicing good hygiene are also important aspects of treatment.
Can Candida albicans infections recur?
Yes, Candida albicans infections can recur, especially in individuals with underlying risk factors or those who have incomplete or inadequate treatment. Recurrent infections may require a thorough evaluation to identify and address any predisposing factors.
Are there any complications associated with Candida albicans infections?
In severe cases or when left untreated, Candida albicans infections can lead to complications. These can include the spread of the infection to other organs (systemic candidiasis), the formation of biofilms, persistent or recurrent infections, or complications related to invasive procedures or medical devices.
Can natural remedies or dietary changes help with Candida albicans infections?
Some individuals may try natural remedies or dietary changes to complement conventional treatment. While there is limited scientific evidence to support their efficacy, some people find relief with measures such as probiotic supplementation, avoiding sugar-rich foods, or following an anti-Candida diet. It is important to consult with a healthcare professional before making any significant changes to your treatment plan or diet.
References
- Mayer FL, Wilson D, Hube B. Candida albicans pathogenicity mechanisms. Virulence. 2013 Feb 15;4(2):119-28. doi: 10.4161/viru.22913. Epub 2013 Jan 9. PMID: 23302789; PMCID: PMC3654610.
- Turner SA, Butler G. The Candida pathogenic species complex. Cold Spring Harb Perspect Med. 2014 Sep 2;4(9):a019778. doi: 10.1101/cshperspect.a019778. PMID: 25183855; PMCID: PMC4143104.
- Calderone RA, Clancy CJ. Candida and Candidiasis. 2nd edition. ASM Press; 2012.
- Pappas PG, Kauffman CA, Andes DR, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the Infectious Diseases Society of America. Clin Infect Dis. 2016;62(4):e1-e50.
- Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369(9577):1961-1971.
- Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev. 2007;20(1):133-163.
- Naglik JR, Gaffen SL, Hube B. Candidalysin: discovery and function in Candida albicans infections. Curr Opin Microbiol. 2019;52:100-109.
- Odds FC, Brown AJ, Gow NA. Antifungal agents: mechanisms of action. Trends Microbiol. 2003;11(6):272-279.
- Mayer FL, Wilson D, Hube B. Candida albicans pathogenicity mechanisms. Virulence. 2013;4(2):119-128.
- Richardson JP, Moyes DL, Ho J, Naglik JR. Candida innate immunity at the mucosa. Semin Cell Dev Biol. 2019;89:58-70.
- Silva S, Henriques M, Oliveira R, Williams DW, Azeredo J. In vitro biofilm activity of non-Candida albicans Candida species. Curr Microbiol. 2011;62(2):354-360.
- Mayer FL, Kronstad JW. Disarming fungal pathogens: Bacillus safensis inhibits virulence factor production and biofilm formation by Candida albicans and Candida glabrata. mBio. 2017;8(3):e00710-17.