What is Bone?
- Bones are integral components of the skeletal system in the human body. There are a total of 206 bones in the adult human skeleton, which can be classified into five main types based on their shape, placement, and additional properties. These types include flat, long, short, irregular, and sesamoid bones.
- The skeletal system serves several crucial functions in the body. First and foremost, bones provide somatic rigidity, giving the body its structural outline and enabling an erect posture and movement, such as the bipedal gait unique to humans. Additionally, bones act as protective structures, safeguarding internal organs and other vital structures within the body.
- Bone is a rigid connective tissue that constitutes the skeletal framework. It is comprised of various types of cells and possesses an internal matrix with a honeycomb-like structure, which imparts rigidity to the bones. The primary role of bones is to provide structural support to the body and facilitate mobility. Furthermore, bones play a role in the production of red blood cells (RBCs) and white blood cells (WBCs), and they also serve as storage sites for minerals.
- Bone tissue is a form of calcified connective tissue. It consists of a matrix composed of ground substance and collagen fibers, within which osteocytes are embedded. Osteocytes are the most abundant cells found in mature bone and are responsible for maintaining bone growth and density. Calcium and phosphate are abundant within the bone matrix, contributing to the strength and density of the bone structure.
- Each bone in the body is connected to one or more other bones through joints, with the exception of the hyoid bone. Through the attachment of tendons and musculature, the skeletal system acts as a lever, generating the force required for movement. The inner core of bones, known as the medulla, contains either red bone marrow, which serves as the primary site of hematopoiesis (formation of blood cells), or yellow bone marrow, which is predominantly composed of adipose tissue.
- Bone development can occur through two main processes: endochondral and membranous ossification. These processes determine the development of various bones in the body, including those in the skull. The specific characteristics of bone development, combined with the overall shape of the bone, are utilized in the classification of the skeletal system.
Definition of Bone
Bone is a rigid connective tissue that forms the framework of the skeletal system in humans and other vertebrates. It provides structural support, protects internal organs, enables movement, produces blood cells, stores minerals, and maintains overall body rigidity.
Features of Bone
Bones possess several notable features that contribute to their structure and function within the body:
- Rigidity: Bones are highly rigid and provide structural support to the body. Their hardness and strength come from the mineralized matrix of calcium salts, particularly hydroxyapatite, which gives bones their characteristic hardness.
- Cellular Composition: Bones are composed of various types of cells. Osteoblasts are responsible for bone formation, while osteoclasts are involved in bone resorption. Osteocytes are mature bone cells that maintain bone health and regulate mineral metabolism.
- Matrix: The matrix of bone is a unique combination of organic and inorganic substances. It consists of collagen fibers that provide flexibility and resilience, as well as a ground substance composed of proteins, glycoproteins, and proteoglycans. The inorganic component, primarily calcium and phosphate, gives bones their hardness.
- Marrow Cavity: Many bones contain a central marrow cavity, which can house either red bone marrow or yellow bone marrow. Red bone marrow is responsible for the production of blood cells, including red blood cells, white blood cells, and platelets. Yellow bone marrow is primarily composed of adipose tissue and serves as a site for energy storage.
- Joints and Articulations: Bones are connected to each other at joints or articulations. These connections can be immovable (as in the skull sutures) or movable (such as the ball-and-socket joint of the hip). Joints allow for movement and flexibility in the skeletal system.
- Blood Supply: Bones have a rich blood supply through a network of blood vessels. Blood vessels penetrate the bone through channels called Haversian canals, supplying nutrients and oxygen to the bone cells and aiding in waste removal.
- Growth and Remodeling: Bones have the ability to grow and remodel throughout life. During growth, the growth plates at the ends of long bones allow for longitudinal bone growth. Remodeling involves the ongoing process of bone resorption by osteoclasts and bone formation by osteoblasts, maintaining bone health and adjusting bone structure according to mechanical demands.
These features collectively contribute to the strength, flexibility, and functional adaptability of bones in the human body.
Bone Structure
Gross Anatomy of Bones
The gross anatomy of bones reveals important structural features that contribute to their function and protection within the body:
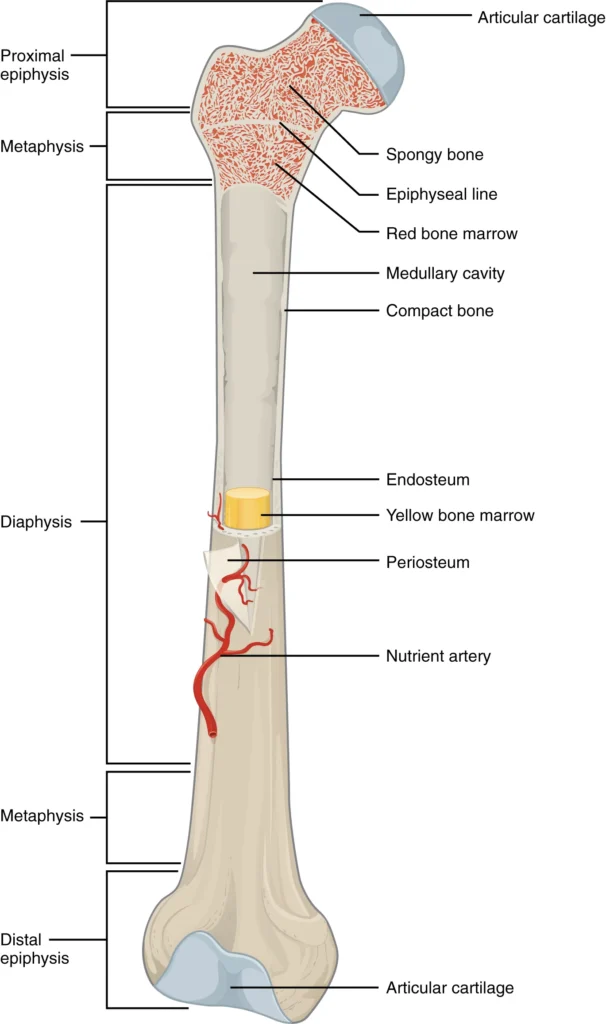
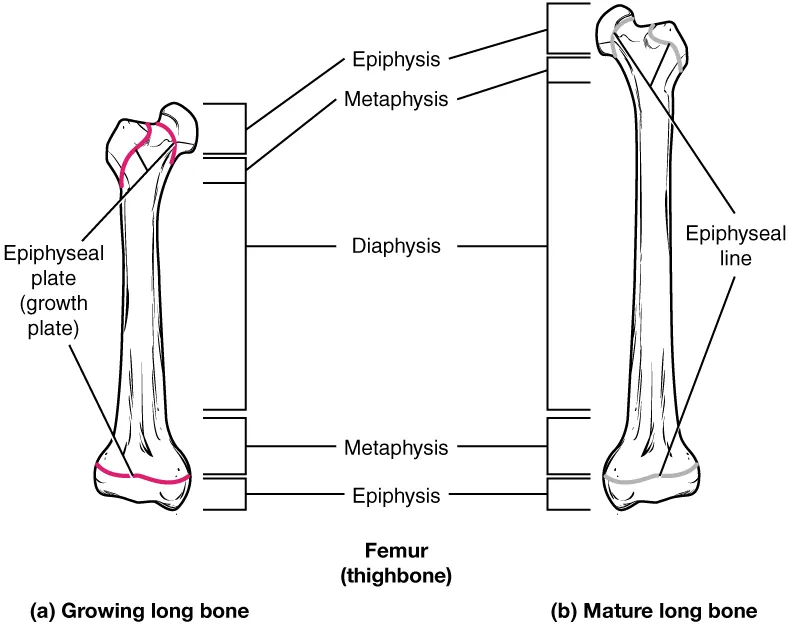
- Long Bones: Long bones, such as the femur or humerus, consist of two main regions: the diaphysis and the epiphysis. The diaphysis refers to the tubular shaft that extends between the proximal and distal ends of the bone. It contains a hollow space called the medullary cavity, which is filled with yellow bone marrow in adults. The outer walls of the diaphysis are composed of dense and hard compact bone.
- Epiphysis: The wider sections at each end of a long bone are known as the epiphyses. Internally, the epiphyses contain spongy bone, which is another type of osseous tissue. In some long bones, such as the femur, red bone marrow fills the spaces within the spongy bone. The epiphyses meet the diaphysis at the metaphysis. During growth, the metaphysis contains the epiphyseal plate, a site of longitudinal bone elongation. In early adulthood, when bone growth ceases, the epiphyseal plate is replaced by an epiphyseal line.
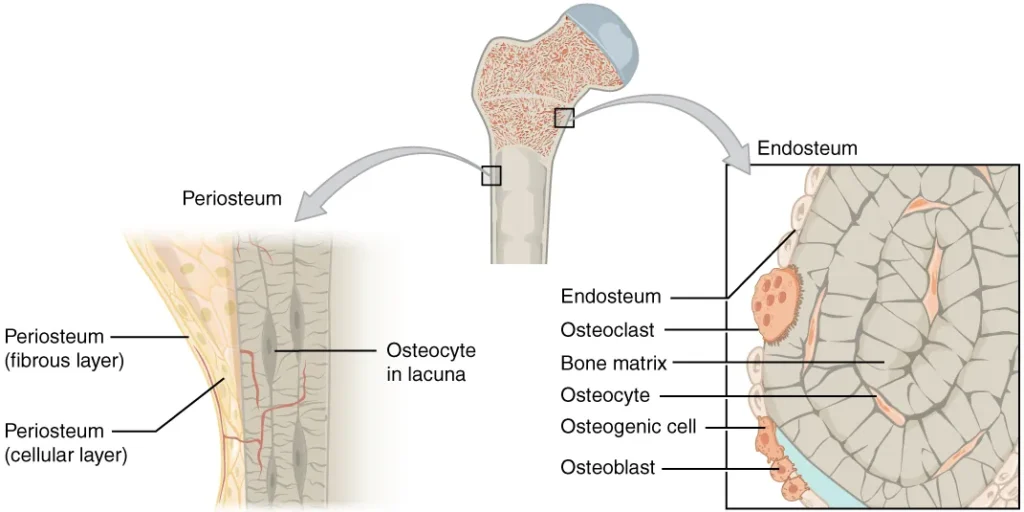
- Endosteum and Periosteum: The inner lining of the bone adjacent to the medullary cavity is called the endosteum. It is a layer of bone cells that contribute to bone growth, repair, and remodeling throughout life. On the outside of the bone, there is the periosteum, a double-layered structure. The cellular layer of the periosteum is adjacent to the cortical bone and is covered by an outer fibrous layer of dense irregular connective tissue. The periosteum contains blood vessels, nerves, and lymphatic vessels that nourish compact bone. Tendons and ligaments attach to bones at the periosteum. The periosteum covers the entire outer surface of the bone, except at the regions where the epiphyses meet other bones to form joints. In these joint regions, the epiphyses are covered with articular cartilage, which acts as a friction-reducing and shock-absorbing layer.
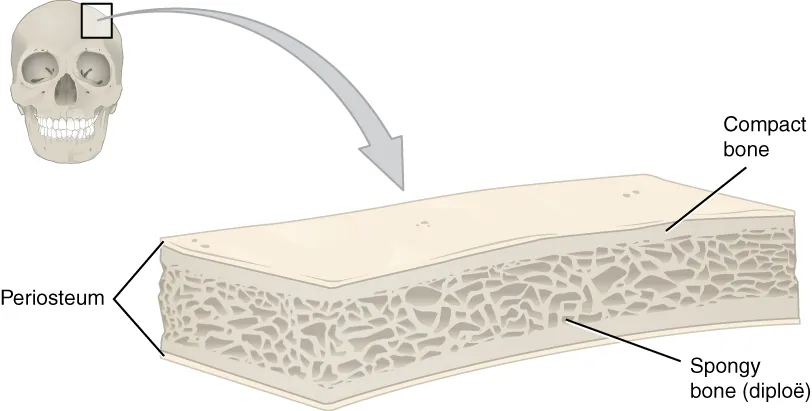
- Flat Bones: Flat bones, such as those in the cranium, have a layered structure. They consist of an inner layer of spongy bone called diploë, sandwiched between two layers of compact bone. This layered arrangement provides protection to internal organs. If the outer layer of a cranial bone fractures, the intact inner layer still offers protection to the brain.
Bone Markings
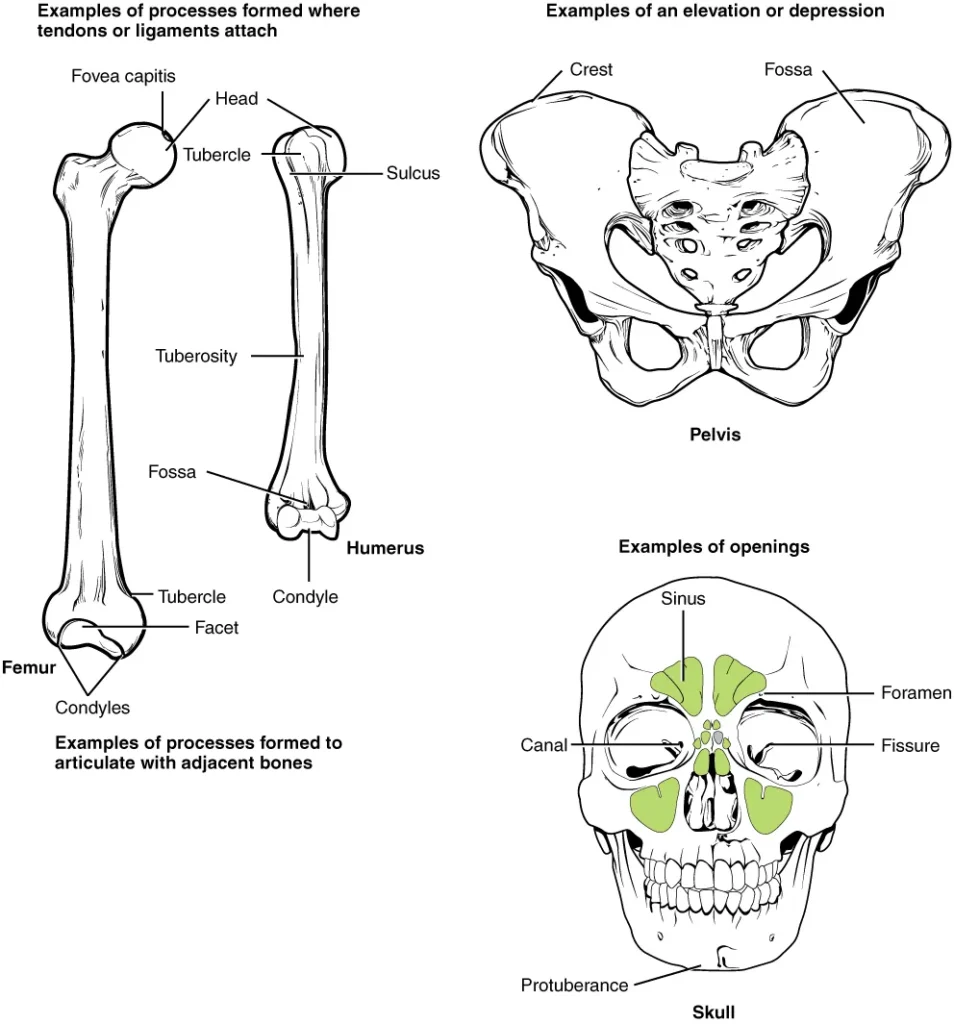
Bone markings refer to the surface features of bones, which vary depending on their function and location in the body. There are three general classes of bone markings: articulations, projections, and holes.
- Articulations: Articulations are where two bone surfaces come together to form a joint. These surfaces are designed to fit each other, such as one being rounded and the other cupped, to facilitate joint movement. An example of an articulation is the knee joint.
- Projections: Projections are raised markings on the surface of a bone. They serve as attachment points for tendons and ligaments, indicating the forces exerted through those attachments. Examples of projections include the spinous process of the vertebrae or the chin.
- Holes: Holes in bones allow the passage of blood vessels and nerves. The size and shape of these holes correspond to the size of the vessels and nerves that enter the bone. Examples of holes include the foramen (holes through which blood vessels pass) and the external auditory meatus.
The following table provides examples of different types of bone markings:
| Marking | Description | Example |
|---|---|---|
| Articulations | Where two bones meet | Knee joint |
| Projections | Raised markings | Spinous process of the vertebrae |
| Holes | Holes and depressions | Foramen magnum in the occipital bone |
Understanding bone markings is essential for studying bone structure, identifying attachment points for muscles and ligaments, and comprehending the functional interactions between bones and other structures in the body.
Bone Matrix and Cells
Bone Matrix
- The bone matrix is a crucial component of osseous tissue, providing the structure and strength necessary for the function of bones. It is primarily composed of collagen fibers and calcium phosphate salt, with collagen accounting for about one-third of the matrix and the calcium phosphate salt comprising the remaining two-thirds.
- Collagen, a protein, forms a scaffold within the bone matrix, providing a surface for the attachment of inorganic salt crystals. These salt crystals, mainly hydroxyapatite, result from the combination of calcium phosphate and calcium carbonate. As the hydroxyapatite crystallizes, it also incorporates other inorganic salts like magnesium hydroxide, fluoride, and sulfate. These crystallized minerals give bones their hardness and strength.
- The collagen fibers within the bone matrix play a vital role in calcification. They provide a framework for the mineralization process, allowing the hydroxyapatite crystals to adhere and grow. Additionally, collagen fibers contribute to the flexibility of bones, preventing them from becoming brittle. Without the collagen matrix, bones would lack the necessary support and crumble easily.
- Conversely, if the inorganic matrix, or minerals, were removed from the bone while leaving the collagen intact, the bone would become overly flexible and lose its ability to bear weight. The balance between the organic collagen matrix and the inorganic mineral matrix is crucial for the proper functioning of bones, providing both strength and flexibility.
- Overall, the bone matrix, with its combination of collagen fibers and mineral salts, provides the necessary framework, strength, and flexibility that allow bones to withstand mechanical stress, support body structures, and perform their essential functions in the skeletal system.
Bone Cells
Bone cells play a crucial role in the functioning and maintenance of bone tissue. There are four main types of bone cells: osteoblasts, osteocytes, osteogenic cells, and osteoclasts.
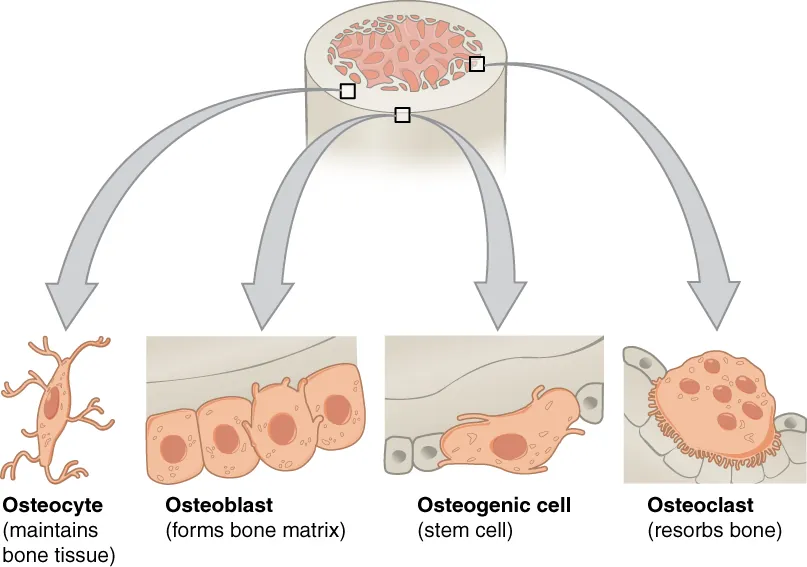
- Osteoblasts: Osteoblasts are responsible for the formation of new bone tissue. They are found in the growing portions of bone, such as the endosteum (inner surface) and the cellular layer of the periosteum (outer surface). Osteoblasts synthesize and secrete the collagen matrix and other proteins that make up the bone matrix.
- Osteocytes: Osteocytes are the most abundant type of bone cell and are considered the primary cells of mature bone. They develop from osteoblasts that become trapped within the calcified bone matrix. Each osteocyte resides in a small cavity called a lacuna. Osteocytes play a crucial role in maintaining the mineral concentration of the bone matrix through the secretion of enzymes. They communicate with each other and receive nutrients through long cytoplasmic processes that extend through canaliculi, which are channels within the bone matrix.
- Osteogenic cells: Osteogenic cells, also known as osteoprogenitor cells, are undifferentiated cells with a high mitotic activity. They are capable of dividing and differentiating into osteoblasts. Immature osteogenic cells are found in the cellular layer of the periosteum and the endosteum.
- Osteoclasts: Osteoclasts are responsible for bone resorption, which is the breakdown of old or damaged bone tissue. These multinucleated cells originate from monocytes and macrophages, types of white blood cells, rather than from osteogenic cells. Osteoclasts continuously break down old bone, while osteoblasts simultaneously form new bone. The balance between osteoblasts and osteoclasts is essential for the constant remodeling and reshaping of bone tissue.
The interaction and coordinated activity of these different bone cells ensure the dynamic nature of bone tissue, with new bone constantly being formed and old bone being broken down and replaced. This ongoing process helps maintain the integrity and strength of the skeletal system.
| Bone Cells (Table 6.3) | ||
|---|---|---|
| Cell type | Function | Location |
| Osteogenic cells | Develop into osteoblasts | Endosteum, cellular layer of the periosteum |
| Osteoblasts | Bone formation | Endosteum, cellular layer of the periosteum, growing portions of bone |
| Osteocytes | Maintain mineral concentration of matrix | Entrapped in matrix |
| Osteoclasts | Bone resorption | Endosteum, cellular layer of the periosteum, at sites of old, injured, or unneeded bone |
Compact and Spongy Bone
Most bones have compact and spongy osseous tissue, but the distribution and concentration of this tissue varies depending on the bone’s overall function. Although compact and spongy bone are formed of the same matrix components and cells, they are structured differently. Compact bone is dense enough to sustain compressive stresses, whereas spongy bone (also known as cancellous bone) has open spaces and is supporting, but it is also lightweight and easily reshaped to fit changing body needs.
Compact Bone
- Compact bone is the denser and stronger type of osseous tissue that forms the outer cortex of all bones and is in direct contact with the periosteum. It is characterized by a highly organized arrangement of concentric circles known as osteons or Haversian systems.
- When observed under a microscope, compact bone appears as a series of concentric circles resembling tree trunks. Each concentric circle is called a lamella, and it is composed of collagen fibers and calcified matrix. The collagen fibers in adjacent lamellae run in perpendicular directions to provide resistance against twisting forces.
- At the center of each osteon, there is a central canal, also known as the Haversian canal, which contains blood vessels, nerves, and lymphatic vessels. These vessels and nerves extend through perforating canals, called Volkmann’s canals, at right angles to reach the periosteum and endosteum. The central canal is lined by the endosteum, which allows for the removal, remodeling, and rebuilding of osteons over time.
- Osteocytes, the primary cells of mature bone, are located within small spaces called lacunae. These lacunae are situated at the borders of adjacent lamellae. Canaliculi, tiny channels, connect the lacunae and allow for communication and nutrient exchange between osteocytes. Despite the calcified nature of the matrix, this system of canaliculi enables the transport of nutrients to the osteocytes and the removal of waste materials from them.
- Compact bone provides strength and support to the skeletal system and plays a vital role in protecting internal organs and providing a framework for movement and locomotion. Its highly organized structure and the network of blood vessels, nerves, and osteocytes contribute to its resilience and ability to adapt to mechanical stress.
Spongy (Cancellous) Bone
- Spongy bone, also known as cancellous bone, differs from compact bone in terms of its structure and arrangement of osteocytes. While both types of bone contain osteocytes housed in lacunae, spongy bone does not have the concentric circles seen in compact bone. Instead, the osteocytes and lacunae are distributed within a lattice-like network of matrix spikes called trabeculae.
- The trabeculae in spongy bone are covered by the endosteum, a cellular layer that facilitates the remodeling of the bone. Although the trabeculae may appear random in their arrangement, each trabecula forms along lines of stress to efficiently direct forces towards the more solid compact bone, providing strength and support to the bone structure.
- One of the important functions of spongy bone is to balance the dense and heavy nature of compact bone. It achieves this by making bones lighter, allowing muscles to move them more easily. The lattice-like structure of spongy bone also serves to distribute forces and stresses throughout the bone, enhancing its overall resilience.
- Moreover, the spaces within some spongy bones contain red bone marrow, which is protected by the trabeculae. Red bone marrow is the site of hematopoiesis, the process of blood cell formation. This crucial function of spongy bone highlights its role in producing and maintaining the body’s blood cells.
- Overall, spongy bone complements the structural properties of compact bone, contributing to the strength, flexibility, and lightweight nature of the skeletal system, while also supporting essential physiological processes such as hematopoiesis.
Blood and Nerve Supply
- Blood and nerve supply play crucial roles in maintaining the health and functionality of bone tissue.
- The blood supply to bones involves arteries that pass through the compact bone to reach the spongy bone and medullary cavity. These arteries enter the bone through small openings called nutrient foramina, which are located in the diaphysis (the tubular shaft of a long bone). This allows for the delivery of oxygen, nutrients, and other essential substances to the bone tissue. The spongy bone receives nourishment from blood vessels of the periosteum, which penetrate the spongy bone and supply nutrients to the osteocytes. Additionally, blood circulates within the marrow cavities, providing nourishment to the bone marrow. As the blood passes through the marrow cavities, it is collected by veins, which then exit the bone through the nutrient foramina.
- Nerve supply to the bone follows a similar pathway as the blood vessels. Nerves enter the bone through the same channels and tend to concentrate in the metabolically active regions of the bone. These nerve fibers play important roles in the regulation of blood supply to the bone, as well as in bone growth. They are also responsible for sensing pain, which is vital for the body’s protective mechanisms. The concentration of nerves in metabolically active sites of the bone reflects their involvement in regulating the bone’s metabolic processes and responding to any potential damage or injury.
- The coordinated supply of blood and nerves ensures the proper functioning and maintenance of bone tissue. It enables the delivery of essential nutrients, oxygen, and regulatory signals, while also facilitating the removal of waste products. This intricate network of blood vessels and nerve fibers supports bone growth, repair, and overall bone health.
Classification of Bone
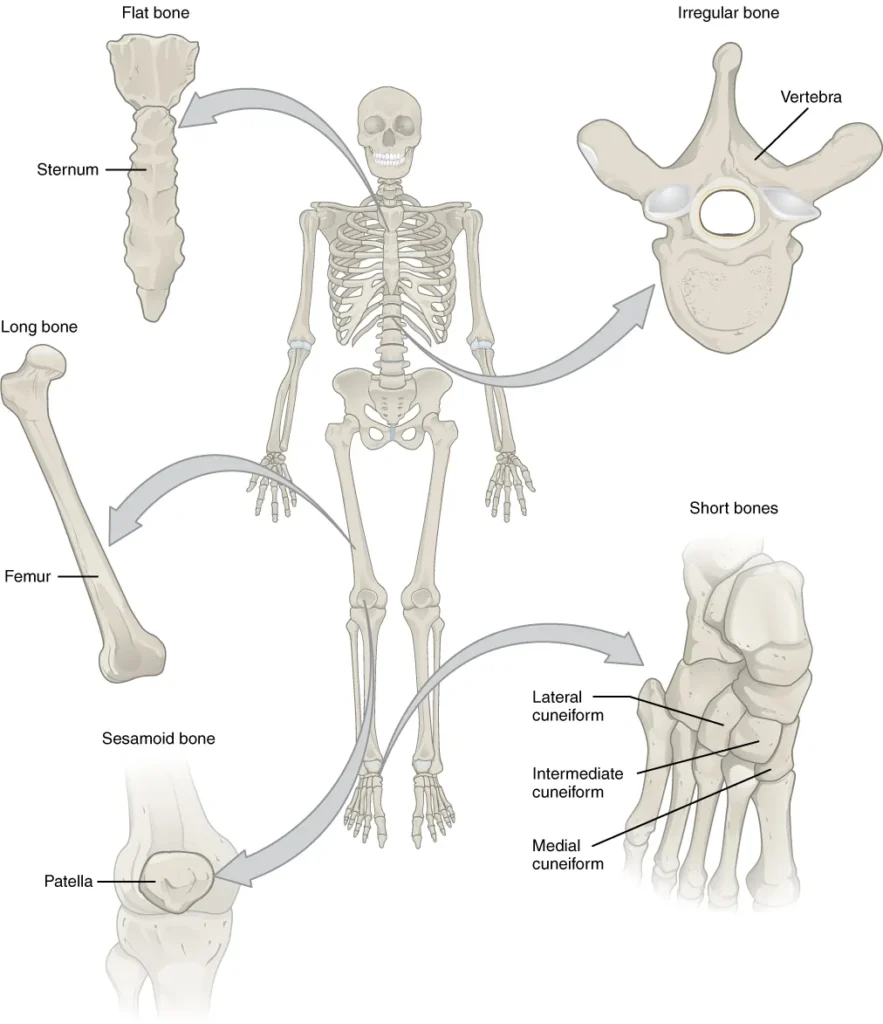
1. Long Bones
- Long bones are a specific type of bone characterized by their cylindrical shape, being longer than they are wide. It’s important to note that the term “long” refers to the shape of the bone, not its size. Long bones are primarily found in the limbs, such as the arms, legs, fingers, and toes. Examples of long bones include the humerus, ulna, radius, femur, tibia, fibula, metacarpals, phalanges, metatarsals, and phalanges.
- The main function of long bones is to act as levers, facilitating movement when muscles contract. They provide support, stability, and mobility for the body. The structure of long bones consists of a shaft called the diaphysis, which contains a marrow cavity filled with bone marrow. The diaphysis is surrounded by a dense layer of compact bone that provides strength and protection. At the ends of the long bones are the epiphyses, which have a rounded shape. The epiphyses are covered with a layer of smooth and slippery articular cartilage, which allows for smooth joint movement. Within the epiphyses, red bone marrow is present, responsible for the production of blood cells through a process called hematopoiesis.
- While most limb bones are classified as long bones, there are a few exceptions. The patella, or kneecap, is a sesamoid bone that develops within the tendon of the quadriceps femoris muscle and is located in the knee joint. Additionally, the bones of the wrist (carpals) and ankle (tarsals) are categorized as short bones due to their cube-like shape.
- Overall, long bones play a vital role in supporting the body, enabling movement, and serving as sites for blood cell production in the bone marrow.
2. Short Bones
- Short bones are a specific type of bone characterized by their cube-like shape, with approximately equal length, width, and thickness. Unlike long bones, short bones do not have a shaft or distinct epiphyses. They are primarily found in the wrists and ankles, specifically in the carpals of the wrists and the tarsals of the ankles.
- The main function of short bones is to provide stability and support to the body, as well as contribute to some limited motion. Due to their compact and sturdy structure, they play a crucial role in maintaining the overall integrity of the skeletal system. The cube-like shape of short bones allows for a greater degree of stability and resistance to compressive forces.
- In the wrists, the short bones known as carpals are arranged in two rows of four bones each, forming the structure of the wrist joint. These carpals work together to provide stability and flexibility to the wrist, allowing for movements such as flexion, extension, and lateral deviation.
- Similarly, in the ankles, the short bones called tarsals are arranged to form the structure of the ankle joint. The tarsals provide stability and support to the foot, allowing for movements such as dorsiflexion, plantarflexion, inversion, and eversion.
- While short bones primarily contribute to stability and support, they also participate in limited motion, facilitating smooth movements and weight distribution. Their compact and solid nature makes them resistant to bending and compression, enhancing their role in providing structural support to the body.
- Overall, short bones, such as the carpals and tarsals, are essential components of the skeletal system, providing stability, support, and some degree of motion in the wrists and ankles. Their cube-like shape and compact structure contribute to the overall strength and integrity of the skeleton.
3. Flat Bones
- Flat bones are a specific type of bone characterized by their thin and broad structure. These bones play a crucial role in providing extensive protection to vital organs and offering broad surfaces for muscle attachment. They are primarily found in areas of the body where protection and muscle attachment are of utmost importance.
- Examples of flat bones include the sternum, ribs, scapulae (shoulder blades), and the roof of the skull. The sternum, commonly known as the breastbone, is a flat bone located in the center of the chest. It serves as a protective shield for the underlying organs, such as the heart and major blood vessels.
- The ribs are another example of flat bones. They form a curved structure that wraps around the thoracic cavity, providing protection to vital organs like the lungs and heart. The ribs also serve as attachment points for muscles involved in respiration and movements of the upper body.
- The scapulae, or shoulder blades, are large flat bones located on the upper back. They provide attachment sites for several muscles involved in arm and shoulder movements, contributing to the stability and flexibility of the shoulder joint.
- The roof of the skull, known as the cranial vault, is composed of flat bones. These bones, including the parietal and frontal bones, encase and protect the brain. The flat nature of these bones helps distribute forces and protect the delicate neural tissue from external trauma.
- Due to their thin and broad structure, flat bones offer a larger surface area for muscle attachment. Muscles, tendons, and ligaments can attach to these broad surfaces, allowing for efficient movement and stability. Additionally, the flat shape of these bones helps to distribute forces and absorb impacts, reducing the risk of injury to underlying organs.
- In summary, flat bones are thin and broad bones that serve important functions in the body. They provide extensive protection to vital organs and offer broad surfaces for muscle attachment. Examples of flat bones include the sternum, ribs, scapulae, and the roof of the skull. Their flat shape and structural characteristics contribute to the overall stability, protection, and functionality of the skeletal system.
4. Irregular Bones
- Irregular bones are a category of bones that do not conform to a specific easily recognizable shape or fit into any other classification of bone shapes. They exhibit complex and unique forms, often serving specialized functions in the body. These bones are typically found in areas where protection and structural support are crucial, but their shapes do not fit the standard descriptions of long, short, or flat bones.
- One prominent example of an irregular bone is the vertebra, which forms the spinal column and protects the delicate spinal cord from compressive forces. The vertebrae are stacked upon one another to create a flexible and protective structure that allows for movement and provides support to the body. Their irregular shape, with distinct features such as the vertebral arch and processes, enables them to interlock and form the spinal canal, safeguarding the spinal cord.
- Many bones of the face are also classified as irregular bones. These include the bones that house the paranasal sinuses, such as the frontal, ethmoid, sphenoid, and maxillary bones. The irregular shape of these facial bones accommodates the sinuses, air-filled cavities that help lighten the skull and contribute to the resonance of the voice. Additionally, the irregular bones of the face, such as the mandible (lower jaw) and the bones of the orbit (eye socket), provide protection for delicate structures like the teeth, eyes, and surrounding soft tissues.
- Irregular bones demonstrate a wide range of shapes and structures that are specifically adapted to their functions. Their unique characteristics make them well-suited for their roles in the body, including protection, support, and housing of specialized features. While irregular bones do not fit into the traditional categories of bone shapes, their complex forms serve important purposes in maintaining the overall structure and function of the skeletal system.
5. Sesamoid Bones
- Sesamoid bones are unique small bones that resemble the shape and size of a sesame seed. They are typically found embedded within tendons, which are fibrous tissues connecting bones to muscles. These specialized bones develop in locations where tendons are subjected to significant pressure within a joint. By forming within tendons, sesamoid bones serve to protect the tendons and assist in overcoming compressive forces during movement.
- The number and placement of sesamoid bones can vary among individuals, but they are commonly found in association with the feet, hands, and knees. In fact, the patellae, commonly known as the kneecaps, are the only sesamoid bones present in every person. The patellae are situated within the quadriceps tendon, which connects the thigh muscles to the tibia bone of the lower leg. These sesamoid bones enhance the mechanical advantage of the quadriceps muscle by improving its leverage during movements such as walking, running, and jumping.
- The presence of sesamoid bones in other areas of the body, particularly in the hands and feet, aids in reducing friction and stress on the tendons as they pass over bony prominences. For example, sesamoid bones can be found near the base of the thumb or big toe, where the corresponding tendons experience high pressure and repetitive motion. These sesamoid bones act as pulleys, altering the direction and reducing the strain on the tendons, thereby improving their efficiency and protecting them from wear and tear.
- While the number and location of sesamoid bones can vary, their general function remains consistent. They play a crucial role in maintaining the integrity and proper functioning of tendons, especially in areas where pressure and stress are prominent. The sesamoid bones help distribute forces evenly, reduce friction, and protect tendons from excessive wear, ultimately contributing to the smooth and efficient movement of the joints.
| Bone Classifications | |||
|---|---|---|---|
| Bone classification | Features | Function(s) | Examples |
| Long | Cylinder-like shape, longer than it is wide | Leverage | Femur, tibia, fibula, metatarsals, humerus, ulna, radius, metacarpals, phalanges |
| Short | Cube-like shape, approximately equal in length, width, and thickness | Provide stability, support, while allowing for some motion | Carpals, tarsals |
| Flat | Thin and curved | Points of attachment for muscles; protectors of internal organs | Sternum, ribs, scapulae, cranial bones |
| Irregular | Complex shape | Protect internal organs | Vertebrae, facial bones |
| Sesamoid | Small and round; embedded in tendons | Protect tendons from compressive forces | Patellae |
Bone Formation or Ossification
The embryo’s skeleton is made up of fibrous membranes and hyaline cartilage in the early stages of development. The true process of bone growth, ossification (osteogenesis), begins by the sixth or seventh week of embryonic life. There are two osteogenic pathways: intramembranous ossification and endochondral ossification, although bone is the same no matter which pathway creates it.
Cartilage Templates
- Cartilage serves as a vital template for the formation of bone during skeletal development. In the early stages of fetal development, a flexible and semi-solid matrix is created by specialized cells called chondroblasts. This matrix, produced by chondroblasts, consists of components such as hyaluronic acid, chondroitin sulfate, collagen fibers, and water. As the matrix surrounds and encapsulates the chondroblasts, they become mature cartilage cells known as chondrocytes.
- Unlike many other connective tissues, cartilage is avascular, meaning it lacks a direct blood supply. Consequently, cartilage relies on diffusion through its matrix to obtain nutrients and eliminate metabolic waste products. This avascular nature of cartilage makes it less capable of self-repair compared to other tissues in the body.
- During fetal development and throughout childhood, bone gradually replaces the cartilaginous template. The process of ossification involves the deposition of a mineral matrix onto the existing cartilage scaffold. By the time a fetus is born, a significant portion of the initial cartilage has been transformed into bone. However, bone growth and development continue during childhood, leading to the replacement of additional cartilage with bone. While most cartilage is replaced by bone, some remnants of cartilage persist in the adult skeleton, primarily in areas requiring flexibility and shock absorption, such as the joints and the external ear.
- The cartilage template plays a critical role in establishing the framework for bone formation and subsequent skeletal development. It serves as a foundation upon which bone can be deposited, providing the necessary structure and shape. Over time, the cartilage is gradually replaced by the stronger and more rigid mineralized matrix of bone, contributing to the growth and maturation of the skeleton.
Intramembranous Ossification
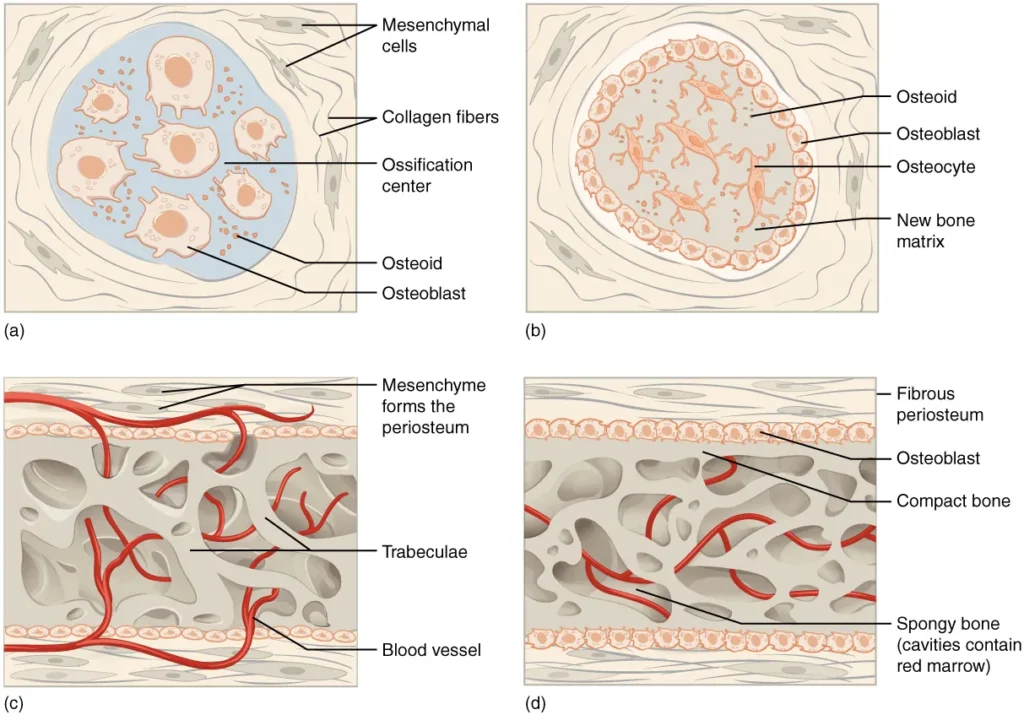
- Intramembranous ossification is a process in which bone develops directly from mesenchymal connective tissue without the presence of a cartilage precursor. This type of ossification is responsible for the formation of flat bones in the face, most cranial bones, and the clavicles.
- The process begins with mesenchymal cells gathering together in the embryonic skeleton and undergoing differentiation into specialized cells. Some of these cells differentiate into capillaries, while others become osteogenic cells and then osteoblasts. The osteoblasts, initially clustered together in an area called an ossification center, secrete osteoid, which is an uncalcified bone matrix.
- Over time, the osteoid calcifies as mineral salts are deposited onto it, resulting in the hardening of the matrix. This calcification process entraps the osteoblasts within the bone matrix, causing them to transform into osteocytes. Simultaneously, the surrounding osteogenic cells differentiate into new osteoblasts, ensuring the ongoing formation of bone tissue.
- As the osteoblasts become osteocytes, the osteoid secreted around the capillaries forms a trabecular matrix. Additionally, the osteoblasts on the surface of the newly formed spongy bone give rise to the periosteum, which is a protective layer surrounding the bone. The periosteum eventually generates a superficial layer of compact bone.
- During intramembranous ossification, the trabecular bone begins to crowd nearby blood vessels, leading to the condensation of these vessels into red marrow. This red marrow contributes to the blood cell production within the bone.
- Intramembranous ossification initiates during fetal development and continues throughout adolescence. At birth, certain bones, such as the skull and clavicles, are not fully ossified, and the sutures of the skull remain open. This flexibility allows for deformations during passage through the birth canal. The final bones to undergo intramembranous ossification are the flat bones of the face, which attain their adult size by the end of the adolescent growth spurt.
Endochondral Ossification
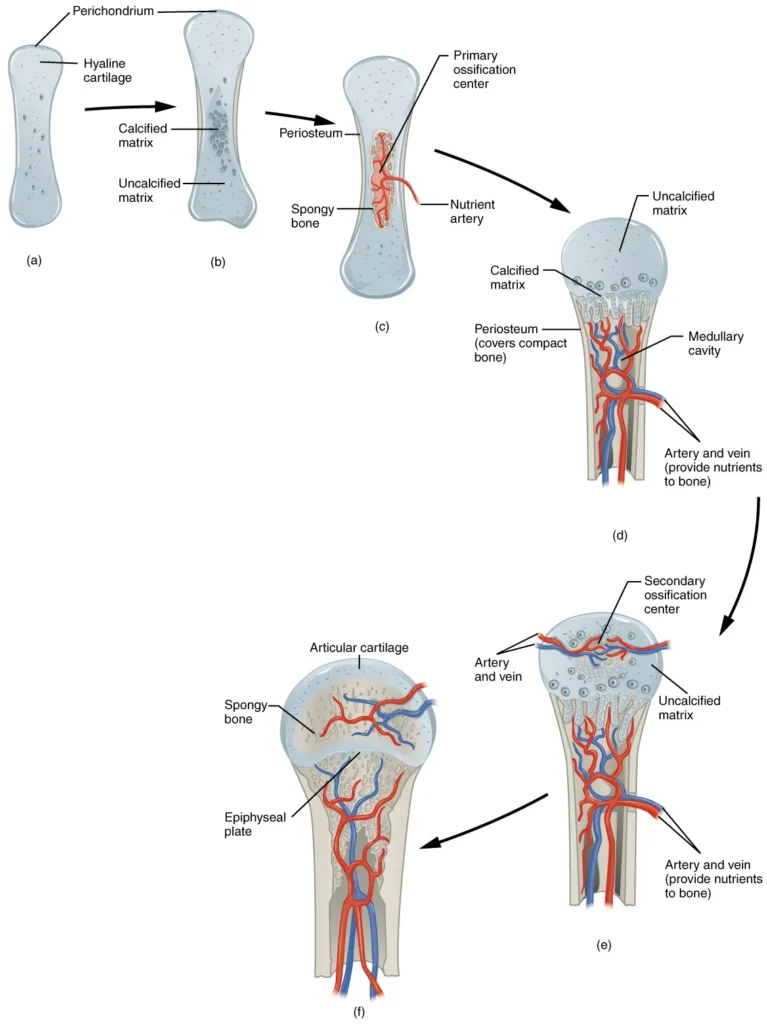
- Endochondral ossification is the process by which bone develops by replacing hyaline cartilage. Unlike in intramembranous ossification, where bone forms directly from mesenchymal connective tissue, in endochondral ossification, cartilage serves as a template that is gradually replaced by bone. This process takes longer compared to intramembranous ossification. Bones at the base of the skull and long bones, such as the femur and humerus, are formed through endochondral ossification.
- During endochondral ossification, at around 6 to 8 weeks after conception, some mesenchymal cells differentiate into chondrocytes, which are cartilage cells that form the cartilaginous skeleton precursor of the bones. The cartilage is covered by a membrane called the perichondrium. As the cartilage matrix is produced, chondrocytes in the center of the cartilage model increase in size. The matrix eventually calcifies, leading to the death of chondrocytes and the disintegration of the surrounding cartilage.
- Blood vessels invade the resulting spaces left by the disintegrating cartilage, enlarging the cavities and carrying osteogenic cells with them. These osteogenic cells differentiate into osteoblasts, which are responsible for bone formation. The enlarging spaces eventually merge to form the medullary cavity within the bone.
- Simultaneously, as the cartilage continues to grow, capillaries penetrate it, initiating the transformation of the perichondrium into the periosteum, which is essential for bone production. Osteoblasts in the periosteum form a collar of compact bone around the cartilage in the diaphysis (shaft) of the bone. This marks the formation of the primary ossification center.
- As the bone develops, chondrocytes and cartilage continue to grow at the ends of the bone, known as the epiphyses. This contributes to the bone’s lengthening while the cartilage in the diaphysis is replaced by bone. By the time the fetal skeleton is fully formed, cartilage remains only at the joint surfaces as articular cartilage and between the diaphysis and epiphysis as the epiphyseal plate, which allows for longitudinal bone growth. After birth, a similar sequence of events occurs in the epiphyseal regions, leading to the formation of secondary ossification centers.
- In summary, endochondral ossification involves the replacement of hyaline cartilage by bone. It begins with the formation of a cartilaginous model, followed by the invasion of blood vessels and the differentiation of osteogenic cells into osteoblasts. The process continues throughout fetal development and into postnatal growth, ultimately resulting in the formation of mature bone.
Bones Growth in Length
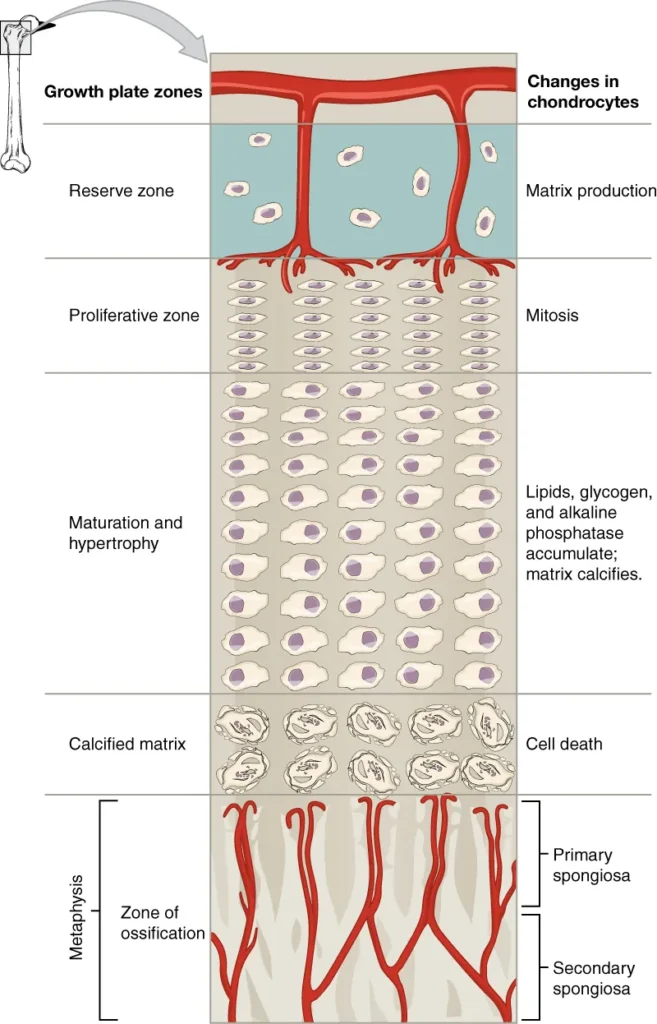
- The growth of bones in length occurs at the epiphyseal plate, which is a layer of hyaline cartilage located at the ends of long bones. The epiphyseal plate is responsible for ossification and bone growth in immature bones. The process of bone growth in length involves different zones within the epiphyseal plate.
- Starting from the epiphyseal side of the plate, cartilage is formed in the reserve zone, which is the region closest to the epiphysis. The chondrocytes in this zone secure the epiphyseal plate to the osseous tissue of the epiphysis but do not actively participate in bone growth.
- Moving towards the diaphysis, the proliferative zone is the next layer of the epiphyseal plate. It consists of slightly larger chondrocytes that undergo mitosis to generate new chondrocytes. These new cells replace the ones that die at the diaphyseal end of the plate.
- Adjacent to the proliferative zone is the zone of maturation and hypertrophy. Chondrocytes in this layer are older and larger than those in the proliferative zone. The cells become more mature as they approach the diaphyseal end of the plate. Cellular division in the proliferative zone and the maturation of cells in the zone of maturation and hypertrophy contribute to the longitudinal growth of the bone.
- The zone closest to the diaphysis is the zone of calcified matrix. In this zone, most chondrocytes are dead because the surrounding matrix has calcified. Capillaries and osteoblasts from the diaphysis invade this zone. Osteoblasts deposit bone tissue onto the remaining calcified cartilage. This process connects the epiphyseal plate to the diaphysis and adds osseous tissue to the diaphysis, resulting in the growth of the bone in length.
- Bone growth in length continues until early adulthood and is regulated by hormones. Once the chondrocytes in the epiphyseal plate stop their proliferation and bone replaces the cartilage, longitudinal growth ceases. The epiphyseal plate then becomes the epiphyseal line, indicating the closure of the growth plate.
- In summary, bones grow in length at the epiphyseal plate through a process involving the proliferation and maturation of chondrocytes. As new bone tissue is added to the diaphysis, the bone grows in length. This growth is controlled by hormones and ceases when the epiphyseal plate closes and becomes the epiphyseal line.
Bones Growth in Diameter
- Bones have the ability to grow in diameter through a process called appositional growth. Unlike longitudinal growth, which determines bone length, appositional growth allows bones to increase in thickness even after longitudinal growth has ceased.
- Appositional growth involves two key activities: bone resorption and bone deposition. Osteoclasts are responsible for resorbing or breaking down old bone that lines the medullary cavity. This resorption of old bone helps create space within the medullary cavity. On the other hand, osteoblasts, through intramembranous ossification, produce new bone tissue beneath the periosteum, which is the dense connective tissue covering the outer surface of bones.
- As osteoclasts resorb old bone along the medullary cavity, osteoblasts deposit new bone beneath the periosteum. This simultaneous process of resorption and deposition increases both the diameter of the diaphysis (the shaft of a long bone) and the diameter of the medullary cavity. The deposition of new bone beneath the periosteum adds layers of compact bone, contributing to the increase in diameter.
- This process of modeling, where old bone is eroded and new bone is formed, allows bones to grow in diameter and become stronger and more structurally sound. It helps maintain the balance between bone resorption and bone deposition, ensuring that bone remains healthy and adapts to mechanical stresses.
- Appositional growth continues throughout life and is influenced by various factors, including mechanical stress, hormonal regulation, and nutritional factors. It plays a crucial role in maintaining bone integrity and adapting bone structure to the changing demands placed on the skeleton.
Resorption and Remodeling of Bone
- Bone remodeling is a continuous process that occurs throughout life to maintain the strength and integrity of the skeleton. It involves the coordinated activity of bone-resorbing cells called osteoclasts and bone-forming cells called osteoblasts. The process of remodeling allows for the removal of old or damaged bone tissue and the replacement with new bone.
- During bone remodeling, matrix resorption and deposition occur on the same bone surface. Osteoclasts are responsible for resorbing or breaking down the existing bone matrix, while osteoblasts are involved in the synthesis and deposition of new bone matrix. This dynamic process helps repair microdamage, adapt bone to mechanical stresses, and regulate calcium and phosphate levels in the body.
- While bone modeling primarily occurs during periods of growth, such as childhood and adolescence, bone remodeling continues in adulthood. Various factors can influence bone remodeling, including injury, exercise, hormonal regulation, and nutritional factors. For example, in response to mechanical stress from weight-bearing activities or exercise, bone remodeling is stimulated to enhance bone strength and density in specific regions.
- Interestingly, even without external influences like injury or exercise, a certain percentage of the skeleton is remodeled annually. Approximately 5 to 10 percent of the bone tissue is remodeled each year, involving the destruction of old bone by osteoclasts and the subsequent renewal of fresh bone by osteoblasts. This ongoing remodeling process helps maintain bone health, repair minor damage, and ensure the replacement of aging bone tissue.
- Bone remodeling is a tightly regulated process that relies on the intricate coordination between osteoclasts and osteoblasts. Imbalances in bone remodeling can lead to conditions such as osteoporosis, where bone resorption exceeds bone formation, resulting in weakened and fragile bones.
- Overall, bone remodeling plays a crucial role in the maintenance, repair, and adaptation of the skeleton, allowing bones to withstand mechanical forces and maintain their structural integrity throughout life.
Fractures: Bone Repair
A fracture is defined as a broken bone. It will heal whether or not it is returned to its anatomical location by a physician. If the bone is not properly reset, the healing process will keep it in the distorted position.
A closed reduction occurs when a broken bone is manipulated and placed into its normal position without the use of surgery. Surgery is required for open reduction to expose the fracture and fix the bone. While some fractures are modest, some are severe and cause serious problems. A broken diaphysis of the femur, for example, has the ability to release fat globules into the bloodstream. These can become trapped in the lungs’ capillary beds, causing respiratory distress and, if not treated promptly, death.
Types of Fractures
Fractures, or broken bones, can be classified based on various characteristics such as their complexity, location, and specific features. Understanding the different types of fractures is important for proper diagnosis and treatment. Here are some common types of fractures:
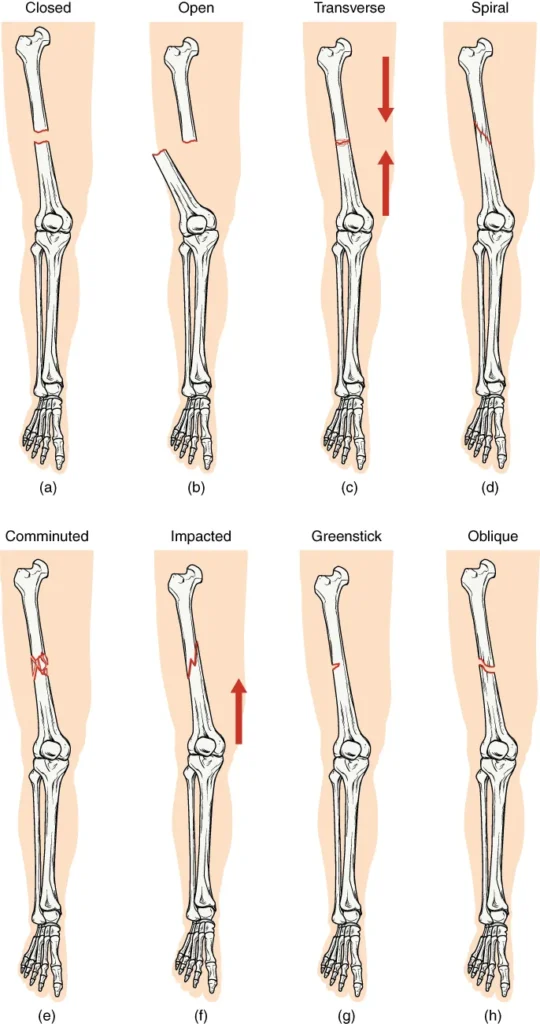
- Transverse Fracture: This type of fracture occurs straight across the long axis of the bone. The break is perpendicular to the bone’s length.
- Oblique Fracture: An oblique fracture is characterized by a diagonal break that occurs at an angle other than 90 degrees. The fracture line runs obliquely across the bone.
- Spiral Fracture: Spiral fractures are the result of a twisting or rotational force applied to the bone. This causes the bone segments to be pulled apart, resulting in a spiral-shaped fracture pattern.
- Comminuted Fracture: In comminuted fractures, the bone breaks into several pieces, resulting in many small fragments between two main segments. This type of fracture often occurs due to high-energy trauma.
- Impacted Fracture: Impacted fractures involve one fragment of the bone being driven or wedged into another fragment. This commonly occurs due to compression forces, causing the bone ends to impact each other.
- Greenstick Fracture: Greenstick fractures are partial fractures seen primarily in children. In this type of fracture, one side of the bone is broken, while the other side bends or remains intact. The fracture resembles the way a green stick breaks.
- Open (or Compound) Fracture: An open fracture occurs when at least one end of the broken bone pierces and tears through the overlying skin. This type of fracture carries a higher risk of infection due to the exposure of the bone to the external environment.
- Closed (or Simple) Fracture: In contrast to an open fracture, a closed fracture does not break through the skin. The skin remains intact despite the underlying bone being fractured.
It’s worth noting that some fractures may exhibit features of more than one type. For example, an open fracture can also be transverse or oblique, depending on the orientation of the fracture line.
Understanding the type of fracture is essential for appropriate treatment planning, including immobilization, realignment (reduction), and potential surgical intervention. Different fractures may require different approaches to promote proper healing and restore normal bone function.
Bone Repair
Bone repair is a complex process that occurs when a bone is fractured. Here’s a breakdown of the stages involved in bone repair:
- Formation of Fracture Hematoma: When a bone breaks, blood vessels in the periosteum, osteons, and medullary cavity are torn, leading to bleeding. Within a few hours after the fracture, the blood begins to clot, forming a fracture hematoma. The lack of blood flow to the bone results in the death of bone cells around the fracture.
- Callus Formation: Within approximately 48 hours, chondrocytes from the endosteum (internal membrane lining the medullary cavity) start creating an internal callus. These chondrocytes secrete a fibrocartilaginous matrix between the broken bone ends. At the same time, periosteal chondrocytes and osteoblasts (bone-forming cells) generate an external callus. The external callus consists of hyaline cartilage and bone, stabilizing the fracture.
- Bone Resorption and Osteoblast Activity: Over the next few weeks, specialized cells called osteoclasts resorb the dead bone tissue. Osteogenic cells, which are precursor cells, become active, divide, and differentiate into osteoblasts. These osteoblasts are responsible for producing new bone tissue.
- Cartilage Replacement by Trabecular Bone: The cartilage present in the calli is gradually replaced by trabecular bone through a process called endochondral ossification. This process involves the transformation of cartilage into bone tissue, resulting in the formation of a bony callus.
- Remodeling and Healing Completion: As the healing process continues, the internal and external calli unite, and the fractured bone becomes more stable. Compact bone replaces spongy bone at the outer margins of the fracture, restoring the bone’s strength. Over time, the bone undergoes remodeling, which involves resorption of unnecessary bone tissue and deposition of new bone to achieve the optimal structure and strength. This remodeling phase helps to restore the bone to its original shape and function.
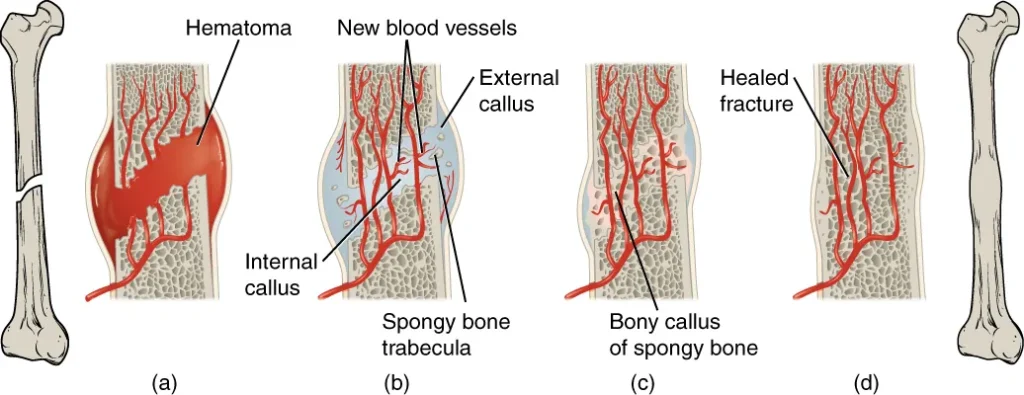
In most cases, after complete healing, there may be no visible evidence of the fracture externally. However, slight swelling or remodeling may occur on the outer surface of the bone, but it usually resolves, leaving no noticeable signs of the previous fracture.
It’s important to note that the timeline and progression of bone repair can vary depending on the individual, the location and severity of the fracture, and other factors such as age and overall health. Proper medical management and support, including immobilization and rehabilitation, are crucial for successful bone repair and functional recovery.
Functions of Bone
- Support: One of the fundamental functions of bones is to provide structural support for the body. They form the framework that gives shape and stability to the body, allowing us to maintain an upright posture and perform various movements.
- Protection: Bones act as protective shields for vital organs and tissues. For example, the skull protects the brain, the ribcage safeguards the heart and lungs, and the vertebrae shield the spinal cord. The hard and durable nature of bone helps prevent damage from external forces.
- Movement: Bones work together with muscles, tendons, and ligaments to enable movement. The attachment points of muscles on bones, through tendons, allow muscles to exert force and generate movement around joints. The skeletal system provides a lever system that facilitates the body’s ability to perform various types of motion.
- Blood Cell Production: Within the bone marrow, a soft and spongy tissue located in the center of many bones, the production of blood cells occurs. Red blood cells, white blood cells, and platelets are produced in the bone marrow through a process called hematopoiesis. These blood cells are essential for carrying oxygen, fighting infections, and promoting clotting.
- Mineral Storage and Homeostasis: Bones act as reservoirs for minerals, especially calcium and phosphorus. These minerals are stored in the bone matrix and can be released into the bloodstream as needed to maintain mineral balance and support vital functions such as muscle contraction, nerve conduction, and blood clotting. Bones also play a role in regulating the levels of calcium in the body through interactions with hormones like parathyroid hormone and calcitonin.
- Endocrine Regulation: Bones produce and release hormones that are involved in various physiological processes. One example is osteocalcin, a hormone produced by bone cells, which plays a role in regulating glucose metabolism and insulin sensitivity.
- Acid-Base Balance: Bones participate in maintaining the acid-base balance of the body by acting as a buffer system. They can release or absorb ions, such as bicarbonate and phosphate, to help regulate the pH level of body fluids.
Collectively, these functions highlight the crucial role that bones play in supporting the body’s structure, protecting vital organs, enabling movement, and contributing to various physiological processes necessary for overall health and well-being.
FAQ
What is the skeletal system?
The skeletal system is the framework of bones, cartilage, and connective tissues that provide support, protect organs, and enable movement in the human body.
How many bones are in the human body?
An adult human body typically has 206 bones. However, the number can vary slightly depending on factors such as age and individual variations.
How are bones classified?
Bones can be classified into four main types: long bones (e.g., femur), short bones (e.g., wrist bones), flat bones (e.g., skull bones), and irregular bones (e.g., vertebrae).
How do bones grow?
Bones grow through a process called ossification. During growth, bones increase in length through the growth plates (epiphyseal plates) and in diameter through appositional growth.
What is a fracture?
A fracture is a broken bone. It can occur due to trauma, such as a fall or impact, or as a result of certain medical conditions weakening the bone.
How do bones heal after a fracture?
After a fracture, bones heal through a process called bone remodeling. The broken ends of the bone are first stabilized, and then new bone tissue is formed to bridge the gap. Over time, the bone remodels and strengthens.
What is osteoporosis?
Osteoporosis is a condition characterized by low bone density and increased bone fragility, leading to an increased risk of fractures. It is more common in older individuals, particularly women after menopause.
Can bones repair themselves?
Yes, bones have the ability to repair themselves. When a bone is fractured, the body initiates a healing process in which new bone tissue is formed to reconnect the broken ends.
What is the role of calcium in bone health?
Calcium is a vital mineral for bone health. It is a major component of the bone matrix and is necessary for the strength and integrity of bones. Adequate calcium intake, along with other nutrients, is essential for maintaining healthy bones.
How can I keep my bones healthy?
References
- https://www.biologydiscussion.com/human-body/bone/ossification/process-of-ossification-in-human-body-connective-tissues-biology/80833
- https://courses.lumenlearning.com/wm-biology2/chapter/types-of-bone/
- https://www.medicalnewstoday.com/articles/320444
- https://www.kenhub.com/en/library/anatomy/bones
- https://www.lecturio.com/concepts/structure-of-bones/
- https://open.oregonstate.education/aandp/chapter/6-3-bone-structure/
- https://pressbooks-dev.oer.hawaii.edu/anatomyandphysiology/chapter/bone-classification/
- https://www.deshbandhucollege.ac.in/pdf/resources/1587723684_BC(H)-IV-Human_Physiology_Bone_Structure_and_formation-1.pdf
- https://openstax.org/books/anatomy-and-physiology-2e/pages/6-3-bone-structure
- https://www.biologydiscussion.com/human-body/bone/classification-of-bone-connective-tissue-human-body-biology/80822