Sourav Pan
Transcript
What are Non-Communicable Diseases, or NCDs?
Non-communicable diseases are medical conditions that cannot be transmitted from person to person. Unlike infectious diseases such as the flu or COVID-19, NCDs cannot spread through direct contact.
NCDs are typically chronic in nature, meaning they last for long periods of time and progress gradually.
These diseases result from a combination of four main factors:
Genetic factors, which include hereditary predispositions passed down through families.
Physiological factors, such as high blood pressure or obesity.
Environmental influences, including air pollution and workplace hazards.
And behavioral factors, such as tobacco use, physical inactivity, and poor diet.
The global impact of NCDs is staggering.
They account for seventy four percent of all deaths worldwide, making them by far the leading cause of mortality globally.
The four major categories of NCDs are:
Cardiovascular diseases, which affect the heart and blood vessels.
Cancer, characterized by abnormal cell growth.
Chronic respiratory diseases, which impact the lungs and airways.
And diabetes, a metabolic disorder affecting blood sugar regulation.
Understanding these non-communicable diseases is crucial for developing effective prevention and management strategies.
Cardiovascular diseases are a major category of non-communicable diseases affecting the heart and blood vessels.
Common cardiovascular conditions include heart disease, which involves narrowed or blocked coronary arteries.
Stroke occurs when blood flow to the brain is blocked, causing brain cell death.
Hypertension, or high blood pressure, damages blood vessels over time and is a major risk factor for other cardiovascular diseases.
Cardiovascular diseases affect how blood flows through your vessels. In a healthy blood vessel, blood flows freely.
In a diseased blood vessel, plaque buildup and narrowing restrict blood flow, reducing oxygen delivery to vital organs.
This restriction of blood flow can lead to tissue damage and impaired organ function.
Several key risk factors increase the likelihood of developing cardiovascular diseases.
High blood pressure puts stress on artery walls, making them more susceptible to damage.
High cholesterol leads to plaque buildup in blood vessels.
Smoking damages blood vessels and reduces oxygen in the blood.
And obesity increases strain on the heart and is linked to high blood pressure and diabetes.
These modifiable risk factors account for over ninety percent of cardiovascular disease risk.
Cardiovascular diseases have an enormous global impact.
They are the number one cause of death globally among all non-communicable diseases.
CVDs account for thirty-two percent of all global deaths, compared to sixteen percent for cancer.
Respiratory diseases and diabetes account for seven and four percent respectively.
This translates to approximately seventeen point nine million deaths annually from cardiovascular diseases.
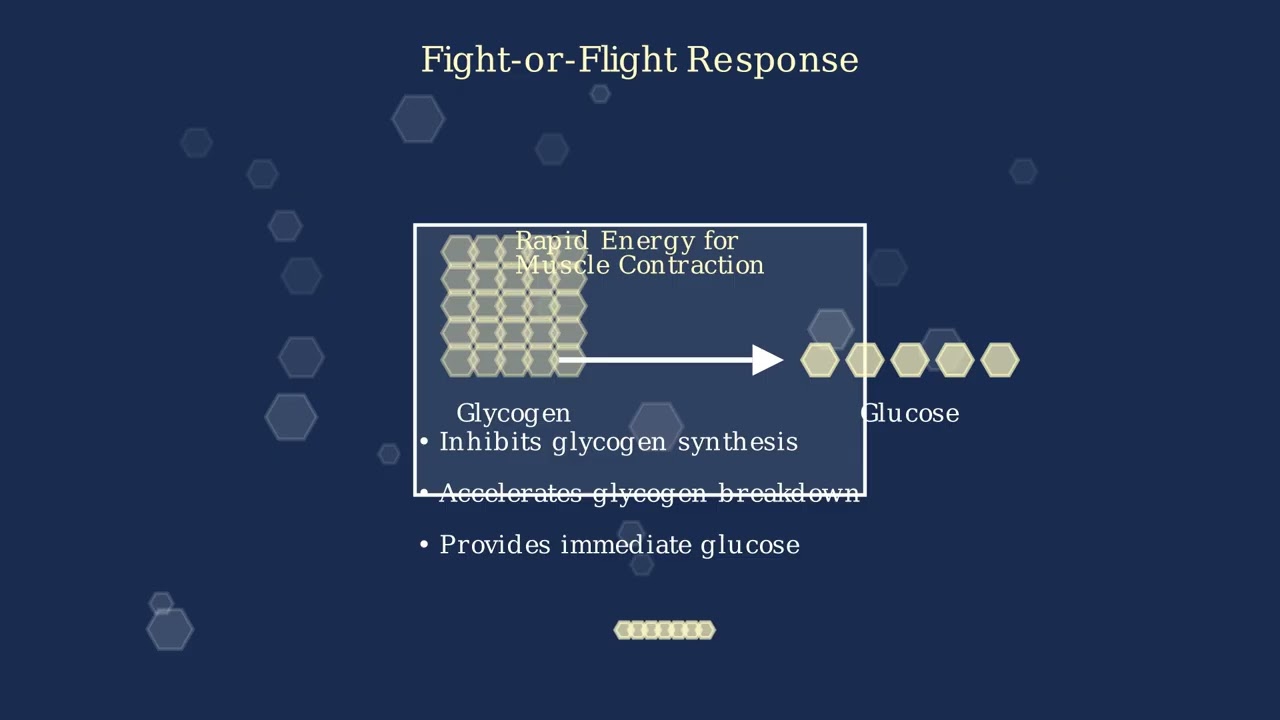
Diabetes is a metabolic disorder characterized by high blood sugar levels. This occurs when the body either doesn’t produce enough insulin or can’t effectively use the insulin it produces.
Insulin, produced by the pancreas, is critical for regulating blood sugar. It allows cells to take in glucose from the bloodstream and use it for energy.
There are two main types of diabetes. Type 1 is an autoimmune condition where the body attacks and destroys insulin-producing cells in the pancreas.
Type 2 diabetes is when the body becomes resistant to insulin or doesn’t produce enough. It’s often associated with lifestyle factors and typically develops in adulthood, though it’s increasingly seen in younger populations.
Diabetes affects multiple body systems and can lead to serious complications if not properly managed.
Cardiovascular complications are common, increasing the risk of heart attack and stroke.
Kidney disease, or diabetic nephropathy, is a serious complication and a leading cause of kidney failure.
Diabetic retinopathy can damage blood vessels in the retina, potentially leading to vision loss or blindness.
Nerve damage, or diabetic neuropathy, can cause pain, numbness, and increase the risk of infections, especially in the feet.
Let’s examine the key risk factors for Type 2 diabetes, which accounts for about 90 percent of all diabetes cases worldwide.
Obesity, especially abdominal obesity, is strongly linked to insulin resistance. A BMI over 30 significantly increases risk.
Physical inactivity reduces the body’s ability to use insulin effectively. Less than 150 minutes of moderate activity per week increases risk.
Poor diet, particularly one high in processed foods, sugars, and unhealthy fats, contributes to weight gain and affects blood glucose regulation.
Genetic factors play a role too. Having a first-degree relative with Type 2 diabetes increases your risk between two and six times.
Age is another factor, with risk increasing after age 45. Other risk factors include ethnicity, gestational diabetes history, and certain medical conditions.
Diabetes has become a global epidemic, with prevalence rising dramatically over the past few decades.
According to the International Diabetes Federation, as of 2021, approximately 537 million adults are living with diabetes worldwide, and this number is projected to reach 783 million by 2045.
The burden is particularly heavy in developing countries, with three in four people with diabetes living in low and middle-income countries.
What’s particularly concerning is that approximately one in two adults with diabetes remain undiagnosed, increasing their risk of developing serious complications.
Prevention strategies are crucial in reducing the global burden of non-communicable diseases.
Prevention strategies fall into four main categories: health promotion and education, creating supportive environments, policy interventions, and encouraging healthy individual behaviors.
Health promotion and education campaigns are essential for raising awareness about NCDs and their risk factors. These include public awareness campaigns, school-based education, community outreach, and digital health platforms.
Creating supportive environments makes healthy choices easier for people. This includes providing accessible recreational spaces, implementing workplace wellness programs, establishing smoke-free zones, and ensuring healthy food options in schools.
Policy interventions are powerful tools governments use to influence health behaviors on a population level. These include tobacco taxes and plain packaging, alcohol minimum pricing and age restrictions, and food labeling requirements and sugar taxes.
These policies can lead to significant population-wide improvements in NCD risk factors, with tobacco interventions showing the highest impact.
Individual health behaviors play a critical role in NCD prevention. The four key behaviors include regular physical activity, balanced nutrition, avoiding tobacco products, and limiting alcohol consumption.
Health guidelines recommend at least 150 minutes of moderate exercise weekly, five or more servings of fruits and vegetables daily, complete avoidance of tobacco products, and limited alcohol consumption.
Prevention strategies for NCDs are significantly more cost-effective than treatment. On average, prevention interventions cost around five thousand dollars per quality-adjusted life year gained, compared to fifteen thousand dollars for treatment.
Studies consistently show that prevention strategies are approximately three times more cost-effective than treatment approaches for reducing the global burden of non-communicable diseases.
Study Materials
No study materials available for this video.
Helpful: 0%
Related Videos
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.