Sourav Pan
Transcript
Histology is the scientific study of microscopic structures of biological tissues.
As a fundamental branch of biology and medicine, histology examines tissues at the cellular level using microscopes.
Histology serves as a bridge between several scientific disciplines.
It connects biochemistry, which studies the chemical processes within living organisms…
…to molecular biology, which focuses on molecular interactions…
…and to physiology, which examines how organisms function.
To understand histology better, let’s compare it with related fields in biology and medicine.
While histology focuses on normal tissue structure, pathology studies disease in tissues. Cytology examines individual cells, and anatomy looks at macroscopic structures.
Histologists study four main types of tissues found in the human body.
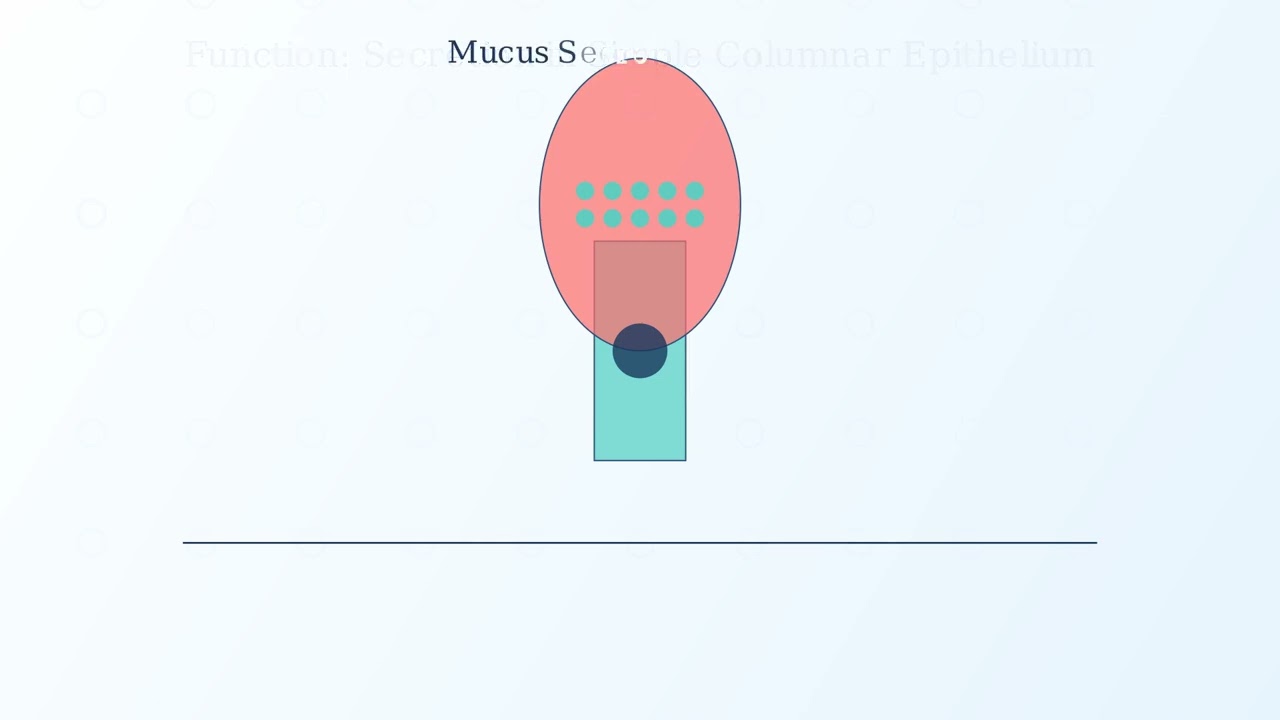
Epithelial tissues cover body surfaces and line cavities. Connective tissues provide support and connect different tissue types.
Muscle tissues enable movement, while nervous tissues transmit signals throughout the body.
Understanding these tissue types through histology is essential for diagnosing diseases and advancing medical research.
Now that we understand what histology is, let’s explore its various subfields.
The field of histology is divided into three main subfields, each focusing on different levels of biological organization.
These subfields are organology, cytology, and tissue studies.
Let’s examine each subfield more closely, starting with organology.
Organology is the study of organs and their structures. It focuses on how different tissues work together to form functional organs.
This subfield examines cross-sections of organs to understand their internal organization, including the arrangement of different tissue layers.
Organologists study various organs including the liver, kidney, heart, and lungs, to understand their structure-function relationships.
Moving to our second subfield, cytology.
Cytology is the study of individual cells. It examines the structure, function, and behavior of cells as the basic units of life.
Cytologists study the internal components of cells, including the cell membrane, nucleus, and various organelles like mitochondria.
This subfield examines various cell types, such as epithelial cells, blood cells, nerve cells, and muscle cells, each with specialized structures and functions.
Our final subfield is tissue studies.
Tissue studies examine how cells organize and function together to form tissues. This subfield bridges the gap between cytology and organology.
This area focuses on how cells with similar structures and functions are arranged together within boundaries to perform coordinated activities.
Histologists study four main tissue types: epithelial tissue, connective tissue, muscle tissue, and nervous tissue, each with distinctive cellular arrangements and functions.
Now let’s see how these three subfields of histology complement each other to provide a complete understanding of biological structures.
These subfields form a continuous spectrum of study, from individual cells to complete organs.
Organology examines how tissues form functional organs, while tissue studies examine how cells organize into tissues.
Cytology provides the foundation for understanding both tissues and organs, as cells are the fundamental building blocks of all biological structures.
Together, these subfields provide a comprehensive view of biological structures at multiple scales of organization.
Sample preparation is a critical first step in histological analysis.
The process involves several key steps: fixation, selection and trimming, and tissue processing.
The first step is fixation, which preserves the tissue’s structure and prevents decay.
Fixation uses chemicals like formalin to cross-link proteins, which preserves the cellular structures and prevents autolysis.
After fixation, the next step is selecting and trimming the tissue to obtain representative sections.
This involves choosing representative tissue samples, trimming them to the proper size of about two to three millimeters thick, and ensuring proper orientation.
The final preparation stage is processing, which prepares the tissue for embedding.
Processing involves three main steps. First, dehydration removes water using a series of increasing alcohol concentrations. Next, clearing with xylene replaces the alcohol. Finally, infiltration allows paraffin wax to permeate the tissue.
Each of these preparation steps is essential to maintain the cellular structure while preventing degradation of the tissue sample.
After processing, tissues need stability for sectioning. This is achieved through embedding.
Embedding involves surrounding processed tissue with a supportive medium that provides rigidity.
The process starts with processed tissue, which is then infiltrated and surrounded by an embedding medium.
Common embedding media include paraffin for routine histology, resin for electron microscopy, and OCT compound for frozen sections.
The purpose of embedding is to provide structural support, enable precise sectioning, and preserve tissue architecture.
Now let’s examine how microtomes are used to cut these embedded tissues into ultrathin sections.
A microtome is a precision instrument used to cut extremely thin sections from embedded tissue blocks. These sections typically range from 2 to 10 micrometers in thickness.
Sections must be thin enough to allow light to pass through for microscopic examination. This enables clear visualization of cellular structures at a single focal plane.
There are several types of microtomes, each designed for specific applications.
The rotary microtome is the most common type. It moves the specimen up and down past a fixed blade and is primarily used for paraffin sections.
The sliding microtome uses a horizontal blade movement. It’s better for larger specimens and produces less compression of the tissue.
The cryostat is a specialized microtome with a built-in freezing chamber, used for cutting frozen sections. It’s particularly valuable for rapid diagnostic applications.
Now let’s explore why proper sectioning technique is crucial for accurate histological analysis.
The quality of sectioning dramatically affects histological analysis. A good section has even thickness, no tears or folds, and shows clear cellular detail.
Poor sectioning technique results in artifacts such as uneven thickness, folds, tears, and compression of the tissue. These artifacts can lead to misinterpretation of the sample.
Let’s look at some common sectioning artifacts and their causes.
To achieve high-quality sections, follow these best practices. Always use sharp, clean blades and ensure proper tissue embedding. Control section thickness consistently, maintain appropriate temperature for the embedding medium, and practice proper handling of the section ribbons.
With proper embedding and sectioning techniques, histologists can produce high-quality slides that enable accurate microscopic analysis of tissues.
Staining Methods in Histology are crucial for visualizing cellular components.
Unstained tissue sections are nearly transparent. Without staining, it’s almost impossible to distinguish cellular structures under a microscope.
This is why staining techniques are essential. The most common method is Hematoxylin and Eosin staining, or H&E for short.
H&E staining uses two main components. Hematoxylin stains cell nuclei blue to purple, highlighting basophilic structures. Eosin stains cytoplasm and extracellular components pink to red, showing acidophilic structures.
The contrast between these two stains makes cellular structures clearly visible, transforming nearly transparent tissue into detailed microscopic views.
H&E staining reveals incredible detail about tissue structure and organization. Here are some examples of different tissues stained with H&E.
H&E staining is fundamental in histology for several reasons. It reveals tissue architecture and organization. It distinguishes between different cellular components. It enables pathologists to identify abnormal cells. And it serves as the foundation for diagnostic histopathology.
This simple yet powerful technique continues to be the cornerstone of histological analysis.
Histology plays a crucial role in diagnosing numerous diseases.
Histology serves as the cornerstone of pathology, allowing for the accurate diagnosis of disease through microscopic examination of tissues.
The diagnostic process begins with tissue sampling and progresses through processing and staining to analysis under the microscope, culminating in a precise diagnosis.
In cancer, normal tissues with uniform cells and organized arrangements transform into a disorganized mass of cells with varied sizes and enlarged nuclei.
Inflammation is characterized by an influx of immune cells, dilated blood vessels, and visible tissue damage, contrasting with the normal tissue’s intact structure.
Fibrosis shows excessive collagen deposition, creating a rigid tissue structure with fewer visible cells, unlike the flexible, normally spaced cells in healthy tissue.
Pathologists identify key diagnostic features such as changes in cell morphology, tissue architecture, cell distribution patterns, and nuclear characteristics to determine disease type and severity.
Histology excels at early disease detection. Subtle microscopic changes often precede clinical symptoms by months or years.
These early changes include minor nuclear alterations and pre-cancerous transformations, which when detected early, significantly improve treatment outcomes.
Beyond diagnosis, histological features help determine the prognosis by revealing disease aggressiveness, likely progression rate, potential treatment response, and risk of recurrence.
Histology remains fundamental to modern medicine, providing the microscopic evidence needed for accurate diagnosis and effective treatment.
Through the microscope, pathologists continue to unveil the cellular secrets of disease, guiding clinical decisions and advancing medical knowledge.
Study Materials
Histology - Definition, Methods, Careers, Importance
Helpful: 0%
Related Videos