Sourav Pan
Transcript
Glycogen has a complex branched structure that allows for efficient glucose storage and release.
The basic building block of glycogen is glucose, which forms a compact hexagonal structure.
In glycogen, glucose units connect through alpha-1,4 glycosidic bonds to form linear chains.
What makes glycogen unique is its branching structure. Branch points connect through alpha-1,6 glycosidic bonds, creating a tree-like molecule.
This branched structure creates a compact molecule that resembles a tree, with many end points available for rapid glucose release.
This branching structure provides several advantages. Multiple end points allow enzymes to release glucose simultaneously from different branches. The compact design increases solubility and maximizes storage efficiency.
In summary, glycogen’s branched molecular structure provides the perfect balance between compact storage and rapid glucose mobilization, making it an ideal energy reserve for the body.
Glycogen, the primary carbohydrate storage molecule in the human body, is stored in two main locations.
The first major storage site is the liver, which contains approximately one hundred grams of glycogen.
The second and larger storage site is skeletal muscle, which holds approximately four hundred grams of glycogen.
These storage locations contain different amounts of glycogen, with muscles storing four times more than the liver.
Despite storing less glycogen, the liver plays a crucial role in maintaining blood glucose levels. When blood glucose falls, liver glycogen is broken down and released into the bloodstream.
In contrast, muscle glycogen serves a different purpose. It provides energy directly to muscle cells during physical activity, especially during high-intensity exercise.
Unlike liver glycogen, muscle glycogen cannot be released into the bloodstream. It can only be used by the muscle cells themselves, which makes it a local energy reserve rather than a contributor to blood glucose regulation.
This key difference in function reflects how the body has evolved specialized storage systems to meet different metabolic needs.
Glycogen stored in the liver plays a crucial role in maintaining stable blood glucose levels throughout the day.
The liver contains approximately 100 to 120 grams of glycogen in healthy adults, serving as our primary glucose reservoir.
Unlike muscle glycogen, which can only be used by the muscles themselves, liver glycogen can be broken down and released as glucose into the bloodstream.
This graph shows how liver glycogen helps maintain blood glucose levels within the normal range throughout the day, even between meals and during overnight fasting.
When blood glucose levels begin to fall, the liver initiates glycogenolysis – the breakdown of glycogen into individual glucose molecules.
Enzymes like glycogen phosphorylase cleave glucose units from the glycogen branches, starting from the outer ends.
Unlike skeletal muscles, liver cells contain the enzyme glucose-6-phosphatase, which allows them to release free glucose directly into the bloodstream.
This release of glucose from liver glycogen is especially important during overnight fasting, when we go many hours without consuming food.
Without liver glycogen, our blood glucose levels would drop dangerously low during sleep, potentially leading to hypoglycemia.
Let’s review the key points about liver glycogen’s role in glucose homeostasis.
The liver stores about 100 to 120 grams of glycogen in adults, which can maintain blood glucose for approximately 24 hours of fasting.
Unlike skeletal muscles, liver cells possess glucose-6-phosphatase, allowing them to release free glucose directly into the bloodstream.
Liver glycogen metabolism is tightly regulated by hormones like insulin and glucagon, ensuring blood glucose remains within the normal range.
This system is especially critical overnight, when we go 8 to 12 hours without food, preventing dangerous drops in blood glucose.
In skeletal muscles, glycogen serves as a critical energy source during physical activity.
Skeletal muscle fibers store glycogen as granules distributed throughout the sarcoplasm.
Glycogen in muscles has a highly branched structure, allowing for rapid mobilization during exercise.
During exercise, muscle glycogen is broken down in a process called glycogenolysis to provide energy.
This process ultimately leads to ATP production, which fuels muscle contraction.
The contribution of glycogen to energy production increases with exercise intensity.
During high-intensity exercise, muscle glycogen becomes the predominant fuel source, providing up to 90 percent of the energy.
Unlike liver glycogen, muscle glycogen can only be used within the muscle itself.
This is because muscle cells lack the enzyme glucose-6-phosphatase, which is needed to release free glucose into the bloodstream.
Understanding how muscle glycogen is utilized is crucial for optimizing exercise performance and recovery.
Glycogenesis is the metabolic pathway for converting glucose into glycogen for storage in the liver and muscles.
Step one of glycogenesis is glucose phosphorylation. The enzyme hexokinase, or glucokinase in the liver, transfers a phosphate group from ATP to glucose, creating glucose-6-phosphate.
In step two, the enzyme phosphoglucomutase converts glucose-6-phosphate to glucose-1-phosphate by moving the phosphate group from the sixth carbon to the first carbon position.
In step three, UDP-glucose pyrophosphorylase converts glucose-1-phosphate to UDP-glucose using UTP as a co-substrate. Then in step four, the enzyme glycogenin acts as a primer, initiating glycogen synthesis by adding the first glucose molecules to itself, creating a short initial chain.
In step five, glycogen synthase extends the glycogen chain by adding glucose units from UDP-glucose to the non-reducing end of the growing chain, forming alpha-1,4-glycosidic bonds.
In the final step, the branching enzyme transfers a segment of about 7 glucose units from the growing chain to create a branch point. This creates alpha-1,6-glycosidic bonds at branch points, giving glycogen its characteristic branched structure.
This branched structure allows glycogen to store a large amount of glucose in a compact form, while providing multiple sites for rapid glucose release when needed.
Glycogenolysis is the metabolic process by which glycogen is broken down to provide glucose during times of need.
To understand this process, let’s first look at the structure of glycogen, which consists of glucose units connected by alpha-1,4 linkages in the main chains and alpha-1,6 linkages at branch points.
Step one of glycogenolysis involves glycogen phosphorylase, which cleaves glucose units from the non-reducing ends of glycogen chains.
When phosphorylase reaches a branch point, it stops. This is where the debranching enzyme comes in with its dual functions.
In the final step, the glucose-1-phosphate produced by phosphorylase is converted to glucose-6-phosphate, which can enter glycolysis or be released into the bloodstream.
To summarize, glycogenolysis is a well-regulated process that efficiently breaks down glycogen’s complex structure to provide glucose when the body needs energy.
Glucagon is a hormone with effects opposite to insulin, primarily promoting glycogen breakdown.
Glucagon is secreted by the alpha cells of the pancreas during fasting states, when blood glucose levels fall too low.
When blood glucose levels fall too low, such as during fasting or between meals…
Alpha cells in the pancreas detect this drop and respond by secreting glucagon.
Glucagon enters the bloodstream and travels to the liver, its primary target organ.
Once glucagon reaches the liver, it triggers a signaling cascade that affects glycogen metabolism.
Glucagon has two major effects on enzymes involved in glycogen metabolism.
The net result is rapid glycogen breakdown in the liver and release of glucose into the bloodstream.
This process raises blood glucose levels back to normal, counteracting hypoglycemia and providing energy during fasting states.
Intracellular signaling in glycogen regulation involves complex cascades that translate hormonal signals into enzymatic actions.
When hormones like glucagon, epinephrine, or insulin bind to their receptors, they initiate signaling pathways that ultimately affect glycogen metabolism.
The first pathway we’ll examine is the cAMP pathway, triggered by hormones like glucagon and epinephrine.
When glucagon or epinephrine binds to a G-protein coupled receptor on the cell surface, it causes a conformational change in the receptor.
This activates a G-protein, which in turn activates the enzyme adenylyl cyclase.
Adenylyl cyclase converts ATP to cyclic AMP, or cAMP, which acts as a second messenger.
cAMP activates Protein Kinase A, or PKA, by binding to its regulatory subunits and causing the release of catalytic subunits.
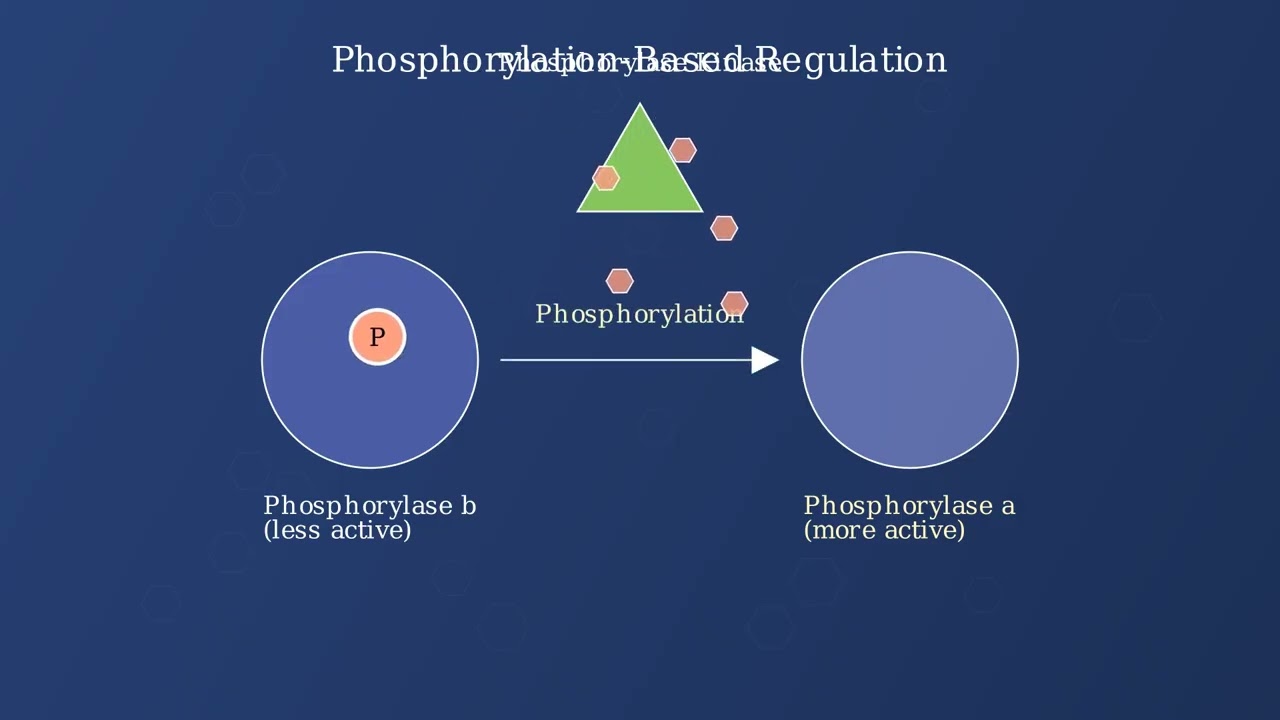
Activated PKA phosphorylates and activates glycogen phosphorylase, which breaks down glycogen, while also phosphorylating and inhibiting glycogen synthase.
A second important pathway is the calcium signaling pathway, which is activated by epinephrine binding to alpha receptors.
When epinephrine binds to an alpha receptor, it activates phospholipase C, or PLC, through a different G-protein.
PLC cleaves phosphatidylinositol 4,5-bisphosphate to produce inositol trisphosphate, or IP3, which diffuses into the cytosol.
IP3 triggers the release of calcium ions from the endoplasmic reticulum, increasing cytosolic calcium concentration.
Calcium binds to calmodulin, forming a calcium-calmodulin complex.
This complex activates phosphorylase kinase, which then phosphorylates and activates glycogen phosphorylase, leading to glycogen breakdown.
The insulin signaling pathway contrasts with the previous pathways by promoting glycogen synthesis rather than breakdown.
Insulin binds to the insulin receptor, a receptor tyrosine kinase, causing receptor autophosphorylation.
The activated receptor phosphorylates insulin receptor substrates, or IRS proteins.
IRS proteins activate phosphatidylinositol 3-kinase, or PI3K.
This leads to the activation of protein kinase B, also known as Akt.
Akt activates protein phosphatase 1, or PP1, which dephosphorylates glycogen synthase, activating it, while also dephosphorylating glycogen phosphorylase, inactivating it.
In summary, intracellular signaling pathways coordinate the regulation of glycogen metabolism.
The cAMP and calcium pathways, triggered by glucagon and epinephrine, promote glycogen breakdown.
In contrast, the insulin pathway promotes glycogen synthesis, storing excess glucose for future energy needs.
These opposing pathways ensure precise control of glycogen metabolism in response to changing energy demands and nutritional states.
GSD Type I, also known as von Gierke disease, is a glycogen storage disorder caused by a deficiency in glucose-6-phosphatase.
The pathophysiology involves a missing glucose-6-phosphatase enzyme, which prevents the conversion of glucose-6-phosphate to glucose in the liver.
Without this enzyme, glucose cannot be released from the liver into the bloodstream, leading to glycogen accumulation in the liver and kidneys.
This disorder presents with several distinct clinical manifestations.
Diagnosis of von Gierke disease involves several different approaches.
Management strategies for von Gierke disease focus on preventing hypoglycemia and managing complications.
With proper management, patients with von Gierke disease can lead relatively normal lives, although careful monitoring is required throughout their lifetime.
Dietary carbohydrates significantly impact glycogen stores in the body. The quantity and quality of carbohydrates directly affect how much glycogen we can store.
Higher carbohydrate intake typically leads to larger glycogen stores, while complex carbohydrates provide sustained glycogen synthesis. The fiber content of food affects absorption rate and glycogen formation.
The timing of carbohydrate intake is crucial for glycogen synthesis. There are three key periods to consider: pre-exercise, during exercise, and post-exercise.
Consuming carbohydrates one to four hours before exercise enhances glycogen availability. During exercise, simple carbohydrates help maintain blood glucose levels. After exercise, there’s a ‘glycogen window’ of thirty to sixty minutes when synthesis is optimal. For best recovery, athletes should consume one to one-point-two grams of carbohydrate per kilogram of body weight.
Carbohydrate loading is a strategy used by athletes to maximize glycogen stores before competition. The graph shows how muscle glycogen levels change during a typical carb loading protocol.
The classic protocol involves a three-day depletion phase followed by a three-day loading phase. Modern protocols often skip the depletion phase and focus on three to four days of high carbohydrate intake, ranging from eight to twelve grams per kilogram of body weight per day. This strategy can increase glycogen stores by fifty to one hundred percent above normal levels, which is particularly beneficial for endurance events lasting more than ninety minutes.
Different dietary approaches have varying effects on glycogen storage. Let’s examine how carbohydrate percentage in the diet impacts glycogen levels.
High-carbohydrate diets, containing fifty-five to seventy percent carbs, maximize glycogen stores. Moderate-carbohydrate diets provide adequate stores, while low-carbohydrate diets significantly reduce glycogen capacity. Ketogenic diets, with less than ten percent carbohydrates, result in minimal glycogen storage.
When following a low-carbohydrate diet, the body undergoes metabolic adaptation over two to four weeks. This adaptation reduces dependence on glycogen by shifting to fat utilization. While this may impair high-intensity performance, research suggests it can preserve endurance capacity after full adaptation.
To summarize, carbohydrate quantity, quality, and timing all affect glycogen synthesis. The post-exercise glycogen window is crucial for recovery. Carbohydrate loading can dramatically increase glycogen stores for endurance events. Your dietary approach should match your performance goals and metabolic needs. And while low-carbohydrate diets require adaptation, they can be viable for some athletes depending on their training and competition requirements.
Study Materials
Glycogen - Structure, Functions, Examples
Helpful: 0%
Related Videos