Sourav Pan
Transcript
Amoebiasis is an infection that affects millions of people worldwide. Understanding what it is and how it works is the first step in learning about this important health condition.
Amoebiasis is an infection caused by a parasite called Entamoeba histolytica. This tiny organism is so small you need a microscope to see it.
Think of this parasite as a tiny invader. It’s a single-celled organism that can enter your body and cause problems.
Amoebiasis primarily affects your intestines. This is where the parasite usually sets up shop and causes the most trouble.
But sometimes, this parasite doesn’t stay put. It can travel through your bloodstream and affect other organs, most commonly the liver.
Amoebiasis is much more common in tropical and subtropical areas around the world. These regions often have challenges with sanitation and clean water access.
Poor sanitation is a major factor that increases the risk of getting amoebiasis. When waste management and clean water access are limited, this parasite can spread more easily.
To summarize what we’ve learned about amoebiasis: it’s caused by a parasite called Entamoeba histolytica, mainly affects your intestines but can spread to other organs like the liver, and is most common in tropical areas with poor sanitation.
Understanding these basics helps us appreciate why amoebiasis is an important global health concern, especially in developing regions where sanitation infrastructure may be limited.
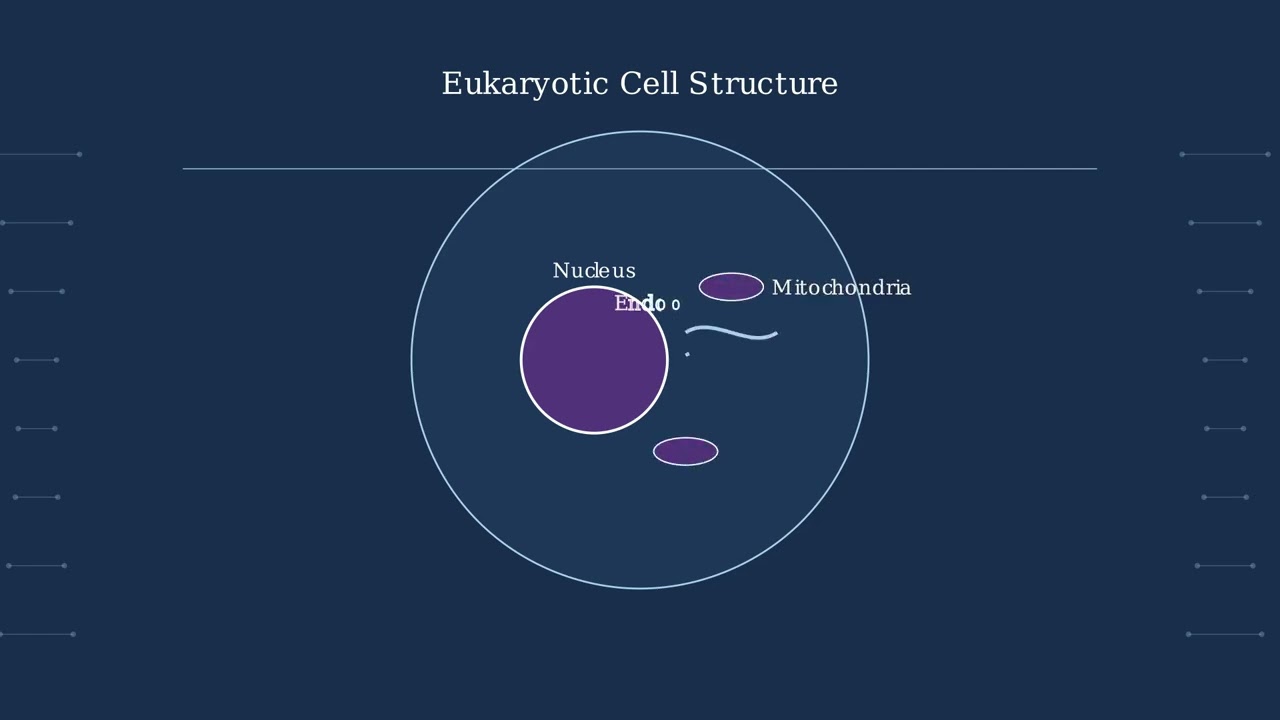
Now we meet the villain of our story: Entamoeba histolytica. This microscopic organism is the single-celled protozoan parasite responsible for causing amoebiasis.
As a protozoan, Entamoeba histolytica is a single-celled organism that belongs to the group of parasites. Despite being just one cell, it’s remarkably sophisticated and dangerous.
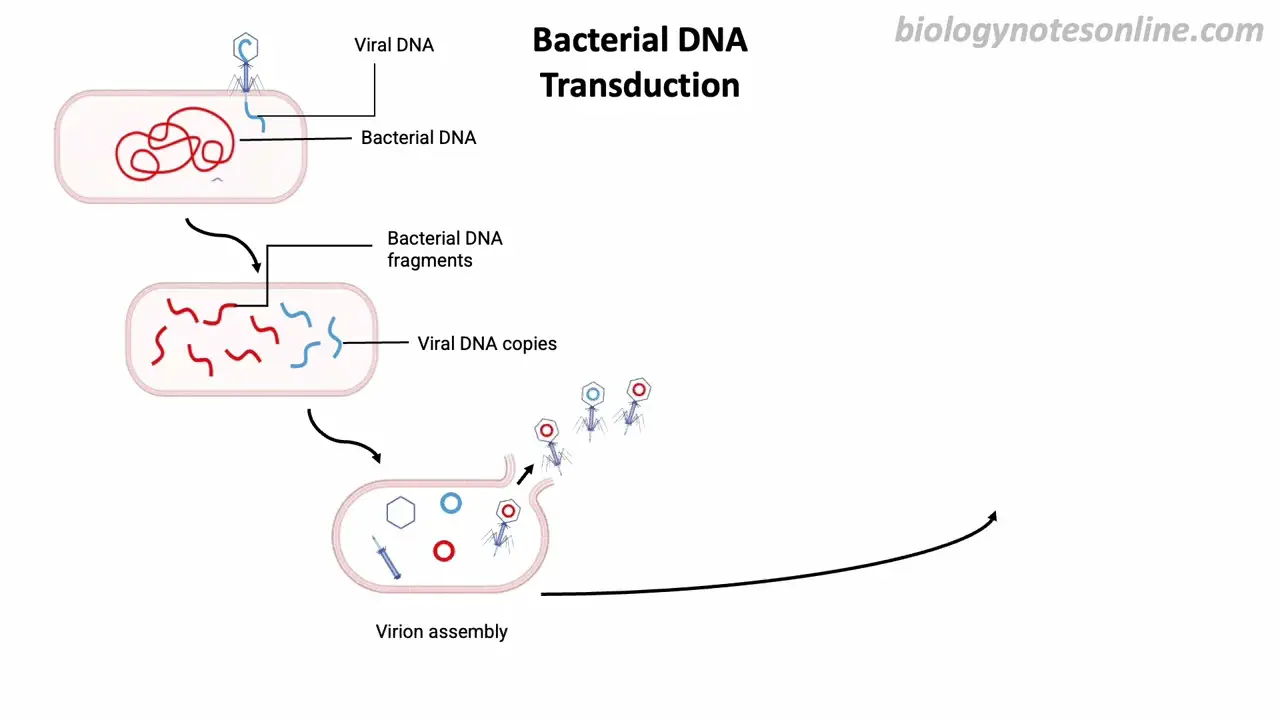
What makes Entamoeba histolytica particularly interesting is that it exists in two distinct forms during its life cycle. Understanding these two forms is absolutely crucial to understanding how the disease spreads.
On the left, we have the cyst form. This is the infective stage with a thick protective wall that makes it incredibly resistant to harsh environmental conditions. Cysts are typically found in formed stool and can survive outside the body for extended periods.
On the right is the trophozoite form. This is the active, motile stage that actually causes disease. Trophozoites are larger, have an irregular shape with extending pseudopods, and actively invade intestinal tissues. They’re typically found in liquid, diarrheal stool.
The trophozoite is constantly moving and changing shape through its pseudopods, which are temporary extensions of its cell membrane. This movement allows it to migrate through tissues and cause damage.
Here’s the key takeaway: cysts are responsible for spreading the infection from person to person, while trophozoites are what actually cause the disease symptoms. Understanding both forms helps us comprehend how amoebiasis spreads and why it can be so persistent.
The life cycle of Entamoeba histolytica begins when you accidentally ingest cysts from contaminated food or water. These microscopic parasites are waiting for their chance to enter your body.
Once you drink contaminated water or eat contaminated food, the cysts travel down to your stomach. These cysts are incredibly tough – they can survive stomach acid, chlorine treatment, and even drying out.
The real transformation happens in your small intestine. Here, the protective cyst wall breaks down in a process called excystation, and the parasite emerges as an active trophozoite.
The newly formed trophozoites are now mobile and hungry. They migrate from the small intestine to the large intestine, where they find their preferred environment and begin to cause problems.
In the large intestine, trophozoites can invade the intestinal wall, causing inflammation and damage. This is where the trouble begins – leading to symptoms like diarrhea, abdominal pain, and potentially serious complications.
This completes the basic life cycle – from tough, resistant cysts that survive harsh conditions, to active trophozoites that invade and damage intestinal tissue. Understanding this cycle helps explain how amoebiasis develops and spreads.
Cysts are the infective form of Entamoeba histolytica. These microscopic structures are the parasite’s survival strategy, designed to withstand harsh environmental conditions and spread infection.
Cysts have several key characteristics that make them highly effective at spreading infection. They’re found in formed stool, have a thick protective wall, contain one to four nuclei, and represent the infective stage of the parasite’s life cycle.
What makes cysts particularly dangerous is their remarkable resistance to environmental factors that would normally kill other microorganisms.
First, cysts are highly resistant to desiccation or drying out. While most microorganisms die quickly when exposed to dry conditions, these cysts can survive for weeks without moisture.
Second, cysts are resistant to stomach acid. The human stomach produces powerful hydrochloric acid that destroys most pathogens, but these cysts pass through unharmed.
Third, cysts are even resistant to chlorination, the standard method used to disinfect drinking water. This means they can survive in treated water supplies, making them particularly effective at spreading infection.
Think of cysts as tiny armored capsules. They have a protective outer shell that keeps the parasite safe inside, waiting for the right conditions. When someone ingests contaminated food or water containing these cysts, they’re ready to hatch and begin infection.
The key takeaway is that cysts are highly resistant survival forms that make Entamoeba histolytica extremely effective at spreading infection. Their ability to withstand harsh environmental conditions means they can persist in contaminated food and water for extended periods, waiting for their next host.
Now we meet the trophozoites – the active, motile stage of Entamoeba histolytica. Unlike the dormant cysts, these are the parasites in action.
Trophozoites are the feeding and moving form of the parasite. They have an irregular, constantly changing shape with extending pseudopodia that help them move and capture food.
Key characteristics of trophozoites include their motility – they can move using pseudopodia, their feeding ability – they actively consume bacteria and tissue, and their fragility – they cannot survive outside the host for long.
Unlike cysts which are found in formed stool, trophozoites are typically found in diarrheal or loose stool. This is because they thrive in the liquid environment of the inflamed intestine.
The most important ability of trophozoites is their power to invade. They can penetrate the intestinal wall, causing tissue damage and the symptoms we associate with amebiasis.
Think of trophozoites as the active soldiers in this parasitic invasion. While cysts are like dormant spores waiting for the right moment, trophozoites are the troops on the battlefield, actively attacking and causing damage.
Key takeaway: Trophozoites are the active, disease-causing form of the parasite. They move, feed, invade tissue, and are responsible for the symptoms of amebiasis. Finding them in stool indicates active infection.
Amoebiasis spreads primarily through a pathway called the fecal-oral route. This happens when people accidentally ingest cysts of Entamoeba histolytica that have contaminated food or water sources.
When someone drinks this contaminated water or eats food prepared with it, the cysts enter their digestive system. Even tiny amounts of contamination can cause infection, making this a very efficient transmission route.
Areas with poor sanitation create ideal conditions for amoebiasis transmission. When human waste contaminates water sources or food preparation areas, the risk of infection increases dramatically.
Several factors increase transmission risk in these environments: open sewage systems, lack of access to clean water, poor waste management, and inadequate handwashing facilities.
Amoebiasis can also spread through oral-anal sexual contact. This represents direct transmission of cysts from an infected person to their partner, bypassing environmental contamination.
This transmission route highlights the importance of understanding all pathways of infection and practicing safe behaviors to prevent transmission.
Good hygiene practices are crucial for preventing amoebiasis transmission. These simple but effective measures can break the cycle of infection and protect individuals and communities.
By understanding how amoebiasis spreads and implementing these prevention strategies, we can significantly reduce the risk of infection and protect public health.
When someone gets infected with Entamoeba histolytica, the parasite doesn’t always cause obvious illness. In fact, most people who are infected don’t even know they have it.
Here’s a remarkable fact: about 90 percent of people infected with this parasite are completely asymptomatic. That means 9 out of every 10 infected people show no symptoms at all.
The remaining 10 percent develop symptomatic infections, meaning they actually get sick from the parasite.
But here’s the important thing to understand about asymptomatic carriers: even though they feel perfectly fine, they’re still spreading the infection.
Asymptomatic carriers continuously pass infectious cysts in their stool. They become unknowing sources of infection, spreading the parasite to others through contaminated food, water, or poor hygiene.
Now let’s look at the 10 percent who do develop symptoms. These symptomatic infections fall into two main categories.
The first type is intestinal amebiasis, where the parasite invades the intestinal wall. This causes symptoms like diarrhea, abdominal pain, and sometimes blood in the stool.
The second type is extraintestinal amebiasis, where the parasite spreads beyond the intestines to other organs, most commonly the liver. This can cause liver abscesses, fever, and pain in the upper right abdomen.
The key takeaway is that most people with this infection don’t know they have it, but they can still spread it to others. Meanwhile, the minority who do get sick can develop serious complications that require medical treatment.
When trophozoites successfully invade the intestinal lining, they cause intestinal amebiasis. This invasion transforms a healthy intestinal wall into an inflamed, damaged tissue that produces characteristic symptoms.
The trophozoites use their pseudopods to move through the intestinal mucosa, causing direct tissue damage and triggering an inflammatory response. This invasion process disrupts the normal function of the intestinal lining.
This intestinal invasion produces four primary symptoms that patients experience. These symptoms can range from mild discomfort to severe, life-threatening complications.
The four primary symptoms of intestinal amebiasis are diarrhea, dysentery which is bloody diarrhea, abdominal pain, and fever. Each symptom results from specific damage caused by the invading trophozoites.
In severe cases, intestinal amebiasis can progress to life-threatening complications. The two most serious complications are intestinal hemorrhage and intestinal perforation.
Intestinal hemorrhage occurs when the parasites damage blood vessels in the intestinal wall, leading to severe bleeding. Intestinal perforation is even more dangerous, creating holes in the intestinal wall that allow intestinal contents to leak into the abdominal cavity.
Early recognition of intestinal amebiasis symptoms is crucial for preventing these severe complications. Prompt medical attention can prevent the progression from mild symptoms to life-threatening conditions.
Sometimes, the trophozoites don’t stay in the intestines. They can break through the intestinal wall and enter the bloodstream, spreading to other organs throughout the body. This is called extraintestinal amebiasis.
Watch as trophozoites move from the intestines into the bloodstream. Once in the blood, they can travel anywhere in the body, but they have preferred destinations.
The liver is by far the most common destination. About 95% of extraintestinal cases involve the liver. Here, trophozoites form what we call amoebic liver abscesses – pockets of infection that can grow quite large and become dangerous.
Less commonly, trophozoites can reach the lungs or even the brain. Lung infections can cause chest pain and breathing problems, while brain infections are extremely serious and can be fatal.
Extraintestinal amebiasis is much more serious than the intestinal form. It requires immediate medical attention and aggressive treatment. The mortality rate is significantly higher, especially when the brain is involved.
When Entamoeba histolytica trophozoites invade beyond the intestinal wall, they can travel through the bloodstream to other organs. The liver is by far the most common destination, leading to what we call an amoebic liver abscess.
Trophozoites that have invaded the intestinal mucosa can enter blood vessels and be carried to the liver through the portal circulation. This is how the infection spreads from the gut to become extraintestinal.
Once in the liver, the trophozoites begin to destroy liver tissue, creating areas of necrosis and inflammation. This leads to the formation of an abscess – essentially a collection of pus and dead tissue within the liver.
Patients with amoebic liver abscess typically present with several characteristic symptoms. The most common include fever, pain in the right upper quadrant of the abdomen, weight loss, and severe fatigue.
Without prompt diagnosis and treatment, amoebic liver abscess can lead to serious, potentially life-threatening complications. These include rupture of the abscess into the chest cavity, secondary bacterial infections, spread to other organs like the lungs or brain, and severe sepsis.
The key takeaway is that amoebic liver abscess represents the most common extraintestinal complication of amebiasis. Early recognition of symptoms and prompt medical treatment are absolutely crucial to prevent the serious complications we just discussed.
Amoebiasis has a distinct global distribution pattern. The disease is not evenly spread across the world, but concentrates in specific regions where certain conditions create the perfect environment for the parasite to thrive.
The highest rates of amoebiasis are found in subtropical and tropical regions. These areas, highlighted in teal, include much of sub-Saharan Africa, parts of South and Southeast Asia, and regions of Central and South America.
Three key factors make these regions particularly vulnerable to amoebiasis: poor sanitation, overcrowding, and malnutrition. Let’s examine how each of these creates conditions that allow the parasite to spread easily.
Poor sanitation is the primary driver. When sewage systems are inadequate and water sources become contaminated, Entamoeba cysts can easily spread through the community water supply and food chain.
Overcrowding amplifies the problem. In densely populated areas with poor infrastructure, the close contact between people increases the chances of transmission through contaminated food and water.
Malnutrition creates a perfect storm. When people don’t have access to adequate nutrition, their immune systems become weakened, making them more susceptible to infection and more likely to develop severe symptoms.
The numbers tell the story clearly. Approximately 500 million people worldwide are infected with Entamoeba species, with the vast majority living in these vulnerable regions where all three risk factors converge.
These regions face a disproportionate burden. While amoebiasis can occur anywhere, about 90 percent of cases are concentrated in areas where poverty, inadequate infrastructure, and limited healthcare access create ideal conditions for the parasite to flourish.
Understanding this global distribution pattern is crucial for public health efforts. It shows us that amoebiasis is not just a medical problem, but a socioeconomic challenge that requires improvements in sanitation, nutrition, and living conditions to truly address the root causes of transmission.
Diagnosing amoebiasis can be challenging because the symptoms often mimic other intestinal diseases. Fortunately, we have several diagnostic methods available, each designed for specific situations and types of infections.
We can organize these diagnostic methods into two main categories. Laboratory tests analyze samples from the patient, while imaging and procedures help us visualize internal structures and obtain tissue samples.
Each method serves a specific purpose in the diagnostic process. Let me explain when and why we use each approach.
The first three methods focus on detecting the parasite or its components in stool samples. Stool examination looks directly for the parasite under a microscope. Antigen detection identifies specific proteins from E. histolytica. PCR testing detects the parasite’s DNA and is the most accurate method.
The remaining methods are used for different situations. Blood serology detects antibodies and is especially useful for extraintestinal infections. Imaging helps locate abscesses in organs like the liver. Aspirate examination analyzes fluid from these abscesses.
The key to successful diagnosis is choosing the right method for each situation. Intestinal infections typically require stool-based tests, while extraintestinal infections often need serology and imaging. Combining multiple methods increases diagnostic accuracy and helps guide appropriate treatment.
Stool examination is the most basic method for diagnosing amoebiasis. A laboratory technician takes a small sample of stool and examines it under a microscope to look for the parasite.
First, we look for cysts. These are the dormant, protective stage of the parasite. Under the microscope, cysts appear as small, round structures with a thick wall and visible nuclei inside.
We also look for trophozoites, which are the active, feeding stage of the parasite. These appear larger and more irregular in shape, with extending pseudopodia that they use for movement and feeding.
However, stool examination has a major limitation. Under the microscope, Entamoeba histolytica looks nearly identical to other harmless Entamoeba species like E. dispar and E. moshkovskii.
It’s like trying to identify a specific car model by just looking at the tires. The tires might look very similar, but they could belong to completely different types of cars – a sports car or a family sedan.
The key takeaway is that while stool examination can detect Entamoeba parasites, it cannot distinguish between the harmful E. histolytica and harmless species. This is why additional, more specific tests are often needed for accurate diagnosis.
While basic stool examination can detect Entamoeba histolytica, stool antigen detection offers a much more specific and sensitive approach to diagnosis.
Stool antigen detection works by identifying specific proteins, called antigens, that are unique to Entamoeba histolytica in stool samples.
The immunoassay uses specific antibodies that are designed to bind only to Entamoeba histolytica antigens, like a lock and key mechanism.
When these antibodies encounter the target antigens in the stool sample, they bind together, creating a detectable signal.
Compared to basic stool examination, antigen detection offers several key advantages that make diagnosis much more reliable.
Basic stool examination relies on microscopic observation, which can miss small numbers of parasites and cannot distinguish between different Entamoeba species.
In contrast, antigen detection specifically identifies Entamoeba histolytica proteins, providing highly sensitive and species-specific results with much greater accuracy.
Stool antigen detection provides four major advantages that make it the preferred diagnostic method for Entamoeba histolytica infections.
It offers higher sensitivity to detect even small amounts of parasites, better specificity to distinguish the pathogenic species, faster results without extensive microscopy, and more reliable outcomes that reduce misdiagnosis.
Stool antigen detection has become the gold standard for diagnosing Entamoeba histolytica infections, providing healthcare providers with the accuracy they need for proper patient care.
PCR, or Polymerase Chain Reaction, represents the gold standard for detecting Entamoeba histolytica DNA in stool samples. This molecular technique provides unparalleled accuracy in diagnosing amoebiasis.
The PCR process begins with extracting DNA from a stool sample. This DNA contains genetic material from all organisms present, including any Entamoeba parasites.
The extracted DNA is then placed into a PCR machine, which uses specific primers designed to target only Entamoeba histolytica DNA sequences. These primers are like molecular keys that only fit the lock of our target parasite.
PCR works through repeated cycles of heating and cooling. Each cycle doubles the amount of target DNA. Starting with just a few DNA molecules, we can create millions of copies in about 30 to 40 cycles.
The key advantage of PCR is its ability to differentiate between Entamoeba species. While microscopy cannot distinguish between them, PCR specifically detects only Entamoeba histolytica, the pathogenic species that causes disease.
PCR offers several key advantages for diagnosing amoebiasis. It provides over 99 percent accuracy, specifically identifies the pathogenic species, and delivers results in just 2 to 4 hours. This makes it the gold standard for confirming Entamoeba histolytica infections.
Serology is a blood test that detects antibodies against Entamoeba histolytica. This diagnostic method is particularly valuable for identifying invasive amoebiasis.
When our immune system encounters Entamoeba histolytica, it produces specific antibodies to fight the infection. These antibodies remain in the blood and can be detected through serology testing.
These Y-shaped antibodies are specifically designed to recognize and bind to Entamoeba histolytica proteins. Their presence indicates that the immune system has encountered this parasite.
Serology is especially useful for diagnosing invasive amoebiasis. When Entamoeba histolytica spreads beyond the intestines to organs like the liver, it triggers a stronger immune response.
Liver abscesses are the most common form of extraintestinal amoebiasis. When parasites reach the liver through the bloodstream, they cause tissue damage and abscess formation.
A positive serology test shows elevated levels of antibodies against Entamoeba histolytica. Both IgM and IgG antibodies may be present, indicating current or recent invasive infection.
The key takeaway is that serology is most valuable when we suspect invasive amoebiasis. Unlike stool tests that detect the parasite directly, serology reveals the body’s immune response, indicating that Entamoeba histolytica has spread beyond the intestinal tract.
When amoebiasis spreads beyond the intestines, doctors need to see inside the body to assess the damage. Medical imaging techniques provide crucial visual evidence of complications like liver abscesses.
Ultrasound is typically the first imaging technique used. It’s non-invasive, widely available, and can quickly identify liver abscesses, which appear as dark, fluid-filled areas on the ultrasound image.
CT scans provide detailed cross-sectional images with excellent tissue contrast. They can precisely show the size and location of abscesses and detect complications like rupture or spread to nearby organs.
MRI provides the highest resolution for soft tissues without radiation exposure. It’s particularly valuable for detecting brain abscesses and provides detailed tissue characterization to distinguish abscesses from other conditions.
On imaging, doctors look for specific signs of damage. A normal liver appears as uniform tissue, while an infected liver shows dark, fluid-filled areas representing abscesses.
Doctors specifically look for round or oval fluid collections with thick walls, surrounding inflammation, and assess the size, number, and location of lesions to plan appropriate treatment.
Imaging techniques are essential tools for detecting and monitoring extraintestinal amoebiasis complications. They not only help diagnose liver abscesses but also guide treatment decisions and track healing progress over time.
When doctors suspect a liver abscess caused by Entamoeba histolytica, they can perform aspirate examination. This involves using a needle to draw fluid directly from the abscess cavity.
The procedure uses ultrasound or CT guidance to safely insert a needle into the abscess. The fluid that’s drawn out appears yellowish and may contain pus, debris, and most importantly for diagnosis, living trophozoites.
The aspirated fluid is then immediately examined under a microscope. This direct examination allows doctors to identify trophozoites in the actual infected tissue.
Under the microscope, the aspirate fluid reveals its contents. The yellowish background represents the pus and inflammatory fluid from the abscess.
The key finding in aspirate examination is the presence of trophozoites. These are the active, motile forms of Entamoeba histolytica that have invaded the liver tissue and caused the abscess.
Each trophozoite shows characteristic features: a distinct nucleus and extending pseudopodia, which are the finger-like projections used for movement and feeding. These features help confirm the diagnosis.
Aspirate examination offers several advantages. It provides direct evidence of the parasite in the infected organ, helps differentiate from bacterial abscesses, and can guide targeted treatment decisions.
This diagnostic method is particularly valuable because it gives doctors immediate, direct evidence of the infection right where it’s causing damage, leading to faster and more targeted treatment for patients.
The field of amoebiasis research is rapidly evolving with exciting new developments. Scientists worldwide are pursuing innovative approaches to combat this parasitic infection through multiple research avenues.
One major trend is the adoption of combination therapies. Instead of using single drugs, researchers are combining multiple medications to enhance treatment effectiveness and reduce the risk of drug resistance developing.
Vaccine development represents another promising research direction. Scientists are working to create a preventive vaccine against Entamoeba histolytica. While still in early research phases, this could revolutionize prevention strategies in endemic areas.
Researchers are also advancing drug delivery systems. Instead of traditional oral medications, scientists are developing targeted nanoparticles and other sophisticated delivery methods that can better reach infected tissues while minimizing side effects.
An exciting emerging trend is the use of artificial intelligence in amoebae research. AI systems can predict the presence of amoebae in environmental samples, suggest personalized treatment options for patients, and accelerate the discovery of new drugs.
These research trends are addressing critical challenges in amoebiasis treatment. By developing combination therapies, vaccines, better drug delivery systems, and using AI, researchers aim to overcome drug resistance, improve treatment effectiveness, reduce treatment duration, and enable personalized medicine approaches.
The amoebiasis treatment market is experiencing significant growth. In 2024, the market was valued at 0.82 billion dollars, and it’s projected to reach 1.14 billion dollars by 2029.
This growth represents a compound annual growth rate of 6.6 percent. But what’s driving this expansion in the amoebiasis treatment market?
Several key factors are driving this market growth. Increased global travel to endemic areas exposes more people to the parasite. Limited access to clean drinking water in developing regions continues to be a major issue.
Additionally, rising immunocompromised populations are more susceptible to severe infections. Greater awareness of the disease is also leading to improved diagnosis and treatment demand.
This market growth is also fueling increased investment in research and development for new treatments and diagnostic methods.
Research efforts are focusing on several key areas. Scientists are developing combination drug therapies for more effective treatment. Vaccine development is a major priority to prevent infections.
Advanced drug delivery systems are being developed to improve treatment effectiveness. New antiprotozoal drugs are also being researched to overcome resistance mechanisms.
The growing amoebiasis treatment market reflects both the ongoing global health challenge posed by this parasite and the increasing commitment to developing better solutions for prevention, diagnosis, and treatment.
Poor sanitation and hygiene create the perfect conditions for amoebiasis to spread. Understanding these factors is essential for prevention.
Three critical factors create conditions where amoebiasis thrives. First, poor sanitation facilities allow human waste to contaminate the environment.
Second, inadequate waste management means sewage and contaminated materials are not properly disposed of, creating multiple sources of infection.
Third, limited access to clean water forces people to use contaminated sources, directly exposing them to infectious cysts.
These factors work together to create a cycle of contamination. Poor sanitation leads to environmental contamination, which then spreads through water and food sources.
Here’s how the contamination cycle works. Contaminated human waste enters the environment through poor sanitation systems.
This waste then pollutes water sources, either directly or through runoff and inadequate treatment systems.
Humans are then exposed to the contaminated water through drinking, cooking, or contact, leading to infection.
Infected individuals then contribute more contaminated waste to the environment, perpetuating the cycle.
Breaking this cycle requires comprehensive improvements in sanitation infrastructure and hygiene practices.
Effective prevention requires three key improvements. First, building proper sanitation facilities that safely contain and treat human waste.
Second, implementing comprehensive waste treatment systems that prevent contamination from reaching water sources.
Third, ensuring universal access to clean, treated water for drinking, cooking, and hygiene purposes.
Improving sanitation and hygiene infrastructure represents the most effective long-term strategy for preventing amoebiasis transmission in communities worldwide.
Prevention is your most powerful tool against amoebiasis. By following simple but effective strategies, you can significantly reduce your risk of infection.
First and most important: practice excellent hand hygiene. Wash your hands thoroughly with soap and clean water for at least twenty seconds, especially before eating, after using the bathroom, and after any contact with potentially contaminated surfaces.
Water safety is crucial. Always drink bottled water from sealed containers, or boil tap water for at least one minute before drinking. Avoid ice cubes, fountain drinks, and beverages that may contain contaminated water.
Food safety requires careful attention. Eat only foods that are served hot and freshly cooked. Avoid raw vegetables, unpeeled fruits, street food, and anything that may have been washed with contaminated water.
When traveling to endemic areas, take extra precautions. Research your destination, pack water purification tablets, bring hand sanitizer, and consider consulting a travel medicine specialist before your trip.
Now let’s talk about when to seek medical attention. Early recognition and treatment are essential for preventing serious complications.
Seek immediate medical attention if you experience persistent diarrhea, especially if it contains blood. Severe abdominal pain, high fever with digestive symptoms, or any symptoms after traveling to endemic areas should prompt a visit to your healthcare provider.
Remember: prevention through good hygiene, safe water and food practices, and prompt medical attention when needed are your best defenses against amoebiasis. These simple steps can protect you and your loved ones from this preventable infection.
The future of amoebiasis treatment is evolving rapidly to address current challenges. Today’s treatments face issues with drug resistance, long treatment durations, and limited therapeutic options.
Pharmaceutical companies are developing innovative drug approaches. Combination therapies use multiple drugs simultaneously to increase effectiveness and reduce resistance. Novel antiprotozoal compounds target specific parasite pathways, while targeted therapies focus on unique parasite vulnerabilities.
Vaccine development represents a major breakthrough opportunity. Researchers are identifying key antigens from Entamoeba histolytica that could provide long-term immunity. Current vaccine candidates are progressing through preclinical testing toward clinical trials.
Advanced drug delivery systems are revolutionizing treatment approaches. Nanoparticle delivery systems can target drugs directly to infected tissues. Sustained release formulations reduce dosing frequency, while targeted delivery minimizes side effects by concentrating drugs where they’re needed most.
Artificial intelligence is transforming amoebiasis research. AI algorithms can accelerate drug discovery by predicting molecular interactions and identifying promising compounds. Machine learning helps personalize treatments based on patient characteristics and can predict resistance patterns before they emerge clinically.
The amoebiasis treatment market is experiencing significant growth, projected to reach over one billion dollars by 2029. This growth is driving substantial investment in research and development. Pharmaceutical companies and research institutions are increasing funding for novel treatments, vaccine development, and improved diagnostic methods.
The future of amoebiasis treatment is bright. Within the next few years, we expect to see new combination therapies reaching patients. Vaccine trials should be completed by 2030, potentially offering prevention for the first time. AI-driven personalized treatments will optimize therapy for individual patients, and long-term goals include significant reduction in global disease burden.
Study Materials
Amoebiasis, Entamoeba Histolytica, Life cycle, Diagnosis
Helpful: 0%
Related Videos
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.