What is Testicle (Testis)?
- The testicles, also known as testes (plural of testis), are the primary male reproductive organs, responsible for producing both sperm and hormones, primarily testosterone. These organs are homologous to the ovaries in females and serve critical roles in both the endocrine and exocrine systems. Testosterone, an essential androgen for male development and reproductive function, is regulated by the luteinizing hormone (LH) from the anterior pituitary gland. Meanwhile, sperm production is controlled by the follicle-stimulating hormone (FSH) and the testosterone produced by the testes themselves.
- Structurally, the testes are oval-shaped and located in the scrotum, a skin-covered sac that hangs outside the body, providing an optimal environment for sperm development by maintaining a temperature slightly lower than body temperature. Each testis is around 3-5 cm in length and 2-3 cm in width, and they are separated by a scrotal septum. The left testis typically hangs lower than the right, and both are supported by the spermatic cord, which also houses nerves and blood vessels.
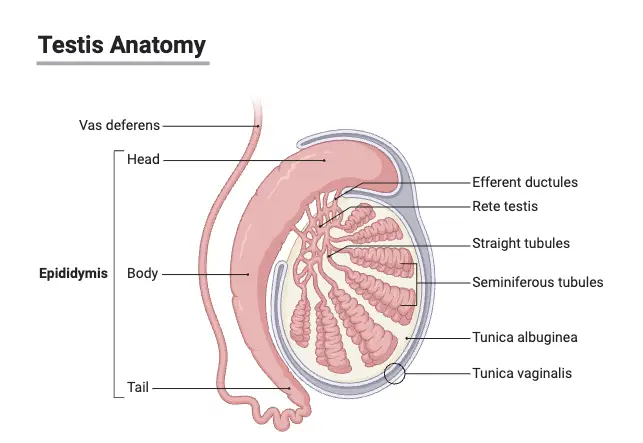
- The testes are encased by a two-layered membrane called the tunica vaginalis, which surrounds all but the posterior and superior regions where the epididymis and spermatic cord are attached. Beneath this layer is a thick, protective covering called the tunica albuginea. Inside the testes, sperm are produced in small, coiled structures called seminiferous tubules.
- Sperm mature and are stored in the epididymis, a highly coiled structure located on the posterior side of each testis. The epididymis is divided into three parts: the head (caput), body (corpus), and tail (cauda). The head receives immature sperm from the testis, which then travel through the epididymis as they mature and gain the ability to fertilize an egg. The total length of the epididymis, if uncoiled, can reach up to 20 feet, providing ample space for sperm storage and maturation.
- The scrotum, which holds the testes, also plays a role in regulating temperature. It is divided into two chambers by a vertical septum, with each chamber containing one testis. The dartos muscle within the scrotal tissue contracts or relaxes in response to temperature changes, giving the scrotum a wrinkled appearance when contracted and smooth when relaxed. Another muscle, the cremaster, can pull the testes closer to the body when it’s cold or when a man is sexually aroused, helping to regulate temperature for optimal sperm production.
- Testicular function is crucial for male fertility and the maintenance of secondary sexual characteristics, making it a key component of the male reproductive system.
Definition of Testicle (Testis)
A testicle, or testis, is a male reproductive gland responsible for producing sperm and the hormone testosterone. Located in the scrotum, the testicles are essential for male fertility and the regulation of male secondary sexual characteristics.
Structure of Testes
The structure of the testes is integral to male reproductive physiology, encompassing various components that facilitate the production and maturation of spermatozoa as well as the synthesis of male hormones. Understanding this anatomical structure is crucial for both educational and clinical contexts.
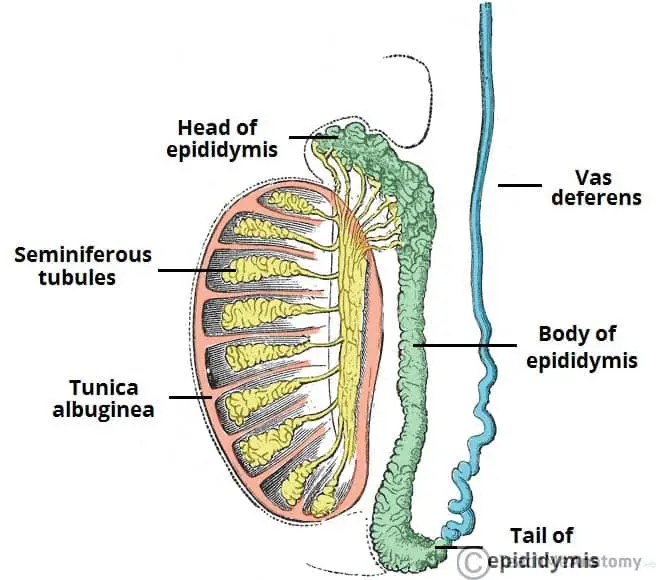
- External Structure: Each testis is oval-shaped, measuring approximately 5 cm in length and 3 cm in diameter. They are suspended in the scrotum by a structure known as the spermatic cord. This cord consists of connective tissue and muscle, housing the vas deferens, blood vessels, lymphatic vessels, and nerves, thereby ensuring the testes are anchored securely and supplied with necessary resources.
- Protective Layers: The testicles are enveloped by the tunica, which comprises two distinct layers:
- Tunica Vaginalis: This outer layer is a closed sac derived from the parietal peritoneum, providing a lubricated environment that reduces friction during movement.
- Tunica Albuginea: The inner layer is a tough fibrous capsule that protects the testicular parenchyma. It extends inward to form septa, which subdivide the testes into approximately 250 lobules.
- Lobular Structure: The testicular lobules are vital for spermatogenesis:
- Seminiferous Tubules: Each lobule contains 1 to 4 seminiferous tubules, totaling around 800 tightly coiled structures within each testis. These tubules are lined with Sertoli cells, which provide support and nourishment to developing sperm cells.
- Interstitial Cells: Located between the seminiferous tubules, the Leydig cells (or interstitial cells) produce testosterone, a critical hormone for male sexual development and function.
- Sperm Pathway: The process of sperm maturation and transportation involves several components:
- Rete Testis: The seminiferous tubules converge into the rete testis, a network of channels where sperm begin their journey.
- Efferent Ducts: From the rete testis, sperm travel through short efferent ducts that connect to the epididymis.
- Epididymis: This is a single, heavily coiled duct that plays a crucial role in sperm maturation and storage. It is divided into three sections:
- Head: Formed by the efferent ducts that carry sperm from the testes.
- Body: Composed of the highly coiled portion of the epididymis, which is where sperm undergo maturation.
- Tail: This distal segment marks the beginning of the vas deferens, which transports sperm to the urethra during ejaculation.
- Lymphatic Drainage: Lymphatic fluid from the testes is transported through vessels in the spermatic cord and drains into the retroperitoneal lymph nodes located at the back of the abdomen. This drainage is essential for immune responses and fluid balance.
Hormones of Testes
The testes play a pivotal role in the male endocrine system by producing essential hormones, primarily testosterone. These hormones are critical for male reproductive health and influence various physiological functions. Understanding the hormones produced by the testes provides insight into their importance in male development and health.
- Testosterone:
- Testosterone is the principal male sex hormone, synthesized and secreted by the Leydig cells located in the interstitial tissue of the testes.
- It is the most prevalent hormone produced by the testes, and a significant portion is converted into dihydrotestosterone (DHT) upon reaching target tissues. DHT is a more active form that exerts potent effects on various tissues.
- This hormone is responsible for the development of male secondary sexual characteristics, such as increased muscle mass, body hair growth, and the deepening of the voice.
- Testosterone also influences overall male body composition, contributing to protein synthesis, muscle growth, increased red blood cell production, and elevated basal metabolic rate, thereby supporting general health.
- During fetal development, testosterone production begins early, stimulated by chorionic gonadotropin from the placenta, facilitating the development of male reproductive structures.
- Regulation of Testosterone Production:
- The synthesis and secretion of testosterone are tightly regulated by the hypothalamus through the release of gonadotropin-releasing hormone (GnRH).
- GnRH stimulates the anterior pituitary gland to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which further influence testicular function.
- LH specifically acts on the Leydig cells, prompting them to produce testosterone, while FSH supports spermatogenesis within the seminiferous tubules.
- Role of Hormonal Feedback:
- The levels of testosterone in the bloodstream are subject to feedback regulation. Elevated testosterone levels can inhibit GnRH and LH secretion, maintaining hormonal balance within the male reproductive system.
- This feedback mechanism is essential for regulating spermatogenesis and ensuring proper reproductive function.
Diseases and disorders of testes
Diseases and disorders of the testes can significantly impact male reproductive health and overall well-being. Understanding these conditions is vital for early detection and appropriate management. Below is a detailed overview of common testicular diseases and disorders, structured for clarity and comprehension.
- Testicular Tumors:
- Testicular tumors are prevalent among children and young adults, manifesting as either benign or malignant growths. Malignant tumors, in particular, can metastasize, affecting other organs.
- Causes:
- One notable risk factor for testicular tumors is cryptorchidism, a condition in which one or both testes fail to descend into the scrotal sac at birth. This abnormal positioning may lead to altered testicular function and an increased risk of tumor formation.
- Symptoms:
- The primary clinical manifestation of testicular tumors includes the development of palpable lumps within the testes. Patients may also experience a sensation of heaviness in the scrotum.
- Types:
- Common types of testicular tumors include seminomas and non-seminomatous germ cell tumors, each with distinct histological features and prognoses.
- Hydrocele:
- Hydrocele is characterized by the accumulation of serous fluid within the tunica vaginalis, the protective sac surrounding the testes. This condition leads to noticeable swelling of the affected testis.
- Etiology:
- Hydrocele can arise as a primary condition or secondary to underlying factors such as infections, trauma, or inflammation. In some cases, it may develop due to other scrotal or testicular disorders.
- Symptoms:
- Common symptoms include swelling in the scrotum, which may vary from acute to chronic presentations. The fluid-filled sac typically does not cause pain, but discomfort may occur if the swelling is significant.
- Diagnosis and Treatment:
- Diagnosis often involves physical examination and imaging studies, such as ultrasound, to differentiate hydrocele from other conditions, such as testicular tumors. Treatment may involve surgical intervention if the hydrocele is persistent or symptomatic.
- Orchitis:
- Orchitis is an inflammation of one or both testes, often resulting from viral or bacterial infections. It can lead to significant discomfort and swelling.
- Causes:
- Common viral causes include mumps, while bacterial orchitis may arise from sexually transmitted infections.
- Symptoms:
- Symptoms typically include pain, swelling, and sometimes fever. Additionally, there may be associated urinary symptoms.
- Epididymitis:
- Epididymitis refers to the inflammation of the epididymis, the duct where sperm mature and are stored. It frequently occurs due to infections.
- Etiology:
- The condition is often linked to bacterial infections, including those caused by sexually transmitted pathogens.
- Symptoms:
- Symptoms include unilateral scrotal pain, swelling, and tenderness, along with potential fever and dysuria.
- Testicular Torsion:
- Testicular torsion is a surgical emergency characterized by the twisting of the spermatic cord, compromising blood flow to the testis.
- Symptoms:
- Symptoms include sudden, severe scrotal pain, swelling, and potentially nausea and vomiting. Immediate medical intervention is critical to prevent testicular necrosis.
Spermatogenesis Process
Spermatogenesis is the intricate biological process through which spermatozoa are produced within the seminiferous tubules of the testes. This process is essential for male fertility and involves multiple stages of cellular development and division. Below is a detailed explanation of spermatogenesis, highlighting its key components and processes.
- Initiation of Spermatogenesis:
- Spermatogenesis commences in the male fetus, when primordial germ cells migrate into the testes and differentiate into spermatogonia. These diploid cells remain dormant until puberty.
- At puberty, hormonal stimulation, primarily by testosterone and follicle-stimulating hormone (FSH), triggers the activation of spermatogonia.
- Cellular Development:
- Spermatogonia undergo mitotic divisions to produce two types of daughter cells:
- Some cells maintain their position at the periphery of the seminiferous tubules as spermatogonia, ensuring a continuous supply of stem cells.
- Others migrate toward the lumen of the tubule and differentiate into primary spermatocytes.
- Each primary spermatocyte, being diploid with 46 chromosomes, then undergoes the first meiotic division (meiosis I).
- Spermatogonia undergo mitotic divisions to produce two types of daughter cells:
- Meiosis I:
- During meiosis I, the primary spermatocyte divides to yield two secondary spermatocytes, each with a haploid number of chromosomes (23 chromosomes).
- Prior to this division, the genetic material within the primary spermatocyte is replicated, resulting in chromosomes that consist of two sister chromatids linked at a centromere.
- Each secondary spermatocyte retains half of the original genetic information, facilitating genetic diversity in subsequent generations.
- Meiosis II:
- Following meiosis I, each secondary spermatocyte undergoes a second meiotic division (meiosis II), which produces two spermatids from each secondary spermatocyte.
- This division does not involve a second replication of genetic material. Instead, the centromere divides, resulting in the separation of sister chromatids into individual, haploid spermatids.
- Consequently, from one primary spermatocyte, a total of four haploid spermatids are generated after both meiotic divisions.
- Spermiogenesis:
- The transition from spermatids to mature spermatozoa is known as spermiogenesis. This phase involves extensive morphological and structural changes, converting round spermatids into streamlined spermatozoa.
- The mature spermatozoon comprises three distinct parts:
- Head: Contains the nucleus with 23 chromosomes, encased by a nuclear membrane. The acrosome, located at the tip of the head, houses enzymes necessary for penetrating the female ovum.
- Midpiece: Packed with mitochondria that produce adenosine triphosphate (ATP), providing the energy needed for sperm motility.
- Tail (Flagellum): Functions as the locomotor apparatus, enabling the sperm to swim towards the egg for fertilization.
- Final Stages and Lifespan:
- Once fully developed, the spermatozoa are released into the lumen of the seminiferous tubules and transported to the epididymis, where they undergo final maturation.
- The entire process of spermatogenesis, from the initial stages of spermatocyte development to the release of mature spermatozoa, takes approximately 74 days.
- After ejaculation, sperm can survive in the female reproductive tract for approximately 48 hours, during which they must reach the egg for successful fertilization.
Functions of Testes
The testes perform several vital functions essential for male reproductive health and overall physiological regulation. Below are the primary functions of the testes, detailed in a structured manner:
- Spermatogenesis:
- The primary function of the testes is the production of spermatozoa, the male gametes. This process occurs within the seminiferous tubules and involves several stages of cell division and maturation.
- Spermatogonia, the germ cells located in the seminiferous tubules, undergo mitosis to produce primary spermatocytes, which then complete meiosis to form secondary spermatocytes and ultimately develop into spermatozoa.
- Hormone Production:
- The testes are responsible for the synthesis of androgens, primarily testosterone, produced by the Leydig cells located between the seminiferous tubules.
- Testosterone plays a crucial role in the development of male secondary sexual characteristics, such as increased muscle mass, body hair growth, and voice deepening during puberty.
- It also regulates libido and is essential for maintaining reproductive function and overall male health.
- Storage of Sperm:
- After their production, spermatozoa are transported to the epididymis, where they are stored and undergo maturation. This storage allows for the sperm to develop motility and the ability to fertilize an egg.
- The epididymis facilitates the gradual maturation of sperm, which can take several days to weeks, ensuring that only fully developed sperm are released during ejaculation.
- Transport of Sperm:
- The testes are connected to the reproductive tract via the vas deferens, which transports mature sperm from the epididymis to the ejaculatory duct.
- During ejaculation, sperm are expelled from the vas deferens, mixed with seminal fluid from the accessory glands, and delivered through the urethra.
- Thermoregulation:
- The testes are located in the scrotum, which helps regulate their temperature, crucial for optimal spermatogenesis. The ideal temperature for sperm production is slightly lower than the body’s core temperature (around 34-35 degrees Celsius).
- The scrotum adjusts its position to maintain this temperature, contracting or relaxing to bring the testes closer to or further from the body as needed.
- Immune Function:
- The testes possess a unique immunological environment that protects developing sperm from the immune system. Sertoli cells create a blood-testis barrier, preventing immune cells from attacking sperm, which are recognized as foreign cells due to their unique genetic composition.
- Influence on Other Hormones:
- Besides testosterone, the testes influence the production of other hormones involved in the male reproductive system, such as inhibin, which regulates the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary gland.
- Tiwana MS, Leslie SW. Anatomy, Abdomen and Pelvis: Testes. [Updated 2023 Apr 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470201/
- https://en.wikipedia.org/wiki/Testicle
- https://emedicine.medscape.com/article/1949259-overview?form=fpf
- https://www.msdmanuals.com/en-in/home/men-s-health-issues/biology-of-the-male-reproductive-system/structure-of-the-male-reproductive-system
- https://www.kenhub.com/en/library/anatomy/the-testes
- https://healthjade.net/human-testicles/
- https://www.aakash.ac.in/important-concepts/biology/testis
- https://cancer.ca/en/cancer-information/cancer-types/testicular/what-is-testicular-cancer/the-testicles
- https://training.seer.cancer.gov/anatomy/reproductive/male/testes.html
- https://teachmeanatomy.info/pelvis/the-male-reproductive-system/testes-epididymis/
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.