IB Biology 13 Views 1 Answers
Sourav PanLv 9November 8, 2024
How have some strains of bacteria evolved to resist antibiotics, and what is the impact of multiple antibiotic resistance?
How have some strains of bacteria evolved to resist antibiotics, and what is the impact of multiple antibiotic resistance?
Please login to save the post
Please login to submit an answer.
Sourav PanLv 9May 15, 2025
The evolution of antibiotic resistance in bacteria is a significant public health challenge, driven by various mechanisms that allow bacteria to survive despite the presence of antibiotics. This resistance not only complicates treatment options but also has broader implications for public health.
Mechanisms of Antibiotic Resistance
- Intrinsic Resistance:
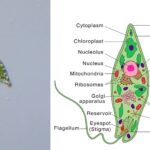
- Some bacteria possess natural characteristics that make them inherently resistant to certain antibiotics. For example, bacteria without a cell wall, like Mycoplasma, are resistant to antibiotics that target cell wall synthesis, such as penicillin.
- Acquired Resistance:
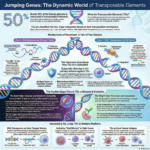
- Bacteria can acquire resistance through genetic mutations or horizontal gene transfer (HGT), where they obtain resistance genes from other bacteria. This can occur via plasmids, transposons, or integrons, which facilitate the transfer of multiple resistance genes between bacterial species. For instance, Escherichia coli can acquire genes conferring resistance to trimethoprim through HGT.
- Mechanisms of Action:
- Bacteria have developed several strategies to resist antibiotics:
- Efflux Pumps: Many bacteria use efflux pumps to expel antibiotics from their cells before they can exert their effects. These pumps can often recognize and eliminate multiple types of antibiotics, leading to multidrug resistance (MDR) .
- Enzymatic Inactivation: Some bacteria produce enzymes that chemically modify or degrade antibiotics, rendering them ineffective. For example, β-lactamases hydrolyze β-lactam antibiotics like penicillin.
- Target Modification: Bacteria may alter the antibiotic’s target site so that the drug can no longer bind effectively. This includes changes in penicillin-binding proteins (PBPs) that are targeted by β-lactam antibiotics.
- Bacteria have developed several strategies to resist antibiotics:
Impact of Multiple Antibiotic Resistance
- Treatment Challenges:
- Infections caused by multidrug-resistant (MDR) bacteria are increasingly difficult to treat, often resulting in longer hospital stays, higher medical costs, and increased mortality rates. When standard treatments fail, healthcare providers may need to resort to more toxic or less effective alternatives.
- Spread of Resistance:
- The presence of MDR bacteria facilitates the spread of resistance genes within and between bacterial populations. Environments with high antibiotic usage, such as hospitals and farms, create selective pressures that favor the survival and proliferation of resistant strains. For example, extended-spectrum beta-lactamase (ESBL)-producing E. coli is becoming more common globally, posing a significant risk for future infections.
- Public Health Threat:
- The rise of MDR bacteria is recognized as a critical public health crisis. It limits treatment options for common infections and complicates procedures such as surgeries and chemotherapy, which rely on effective antibiotics to prevent infections. The World Health Organization has identified antibiotic resistance as one of the top ten global public health threats facing humanity today.
0
0 likes
- Share on Facebook
- Share on Twitter
- Share on LinkedIn
0 found this helpful out of 0 votes
Helpful: 0%
Helpful: 0%
Was this page helpful?