Sourav Pan
Transcript
Today we’re exploring Plasmodium, a fascinating yet dangerous group of microscopic parasites that have shaped human history through the disease they cause.
Plasmodium is a genus of unicellular, eukaryotic parasites. Let’s break this down. Unicellular means each organism consists of just one cell, and eukaryotic means this cell has a true nucleus containing genetic material.
These parasites are described as obligate parasites, which means they absolutely must live inside a host cell to survive and reproduce. They cannot exist independently in the environment.
Plasmodium parasites are the causative agents of malaria, a serious disease that affects millions of people worldwide. This makes understanding these tiny organisms crucial for global health.
To summarize: Plasmodium are single-celled eukaryotic parasites that must live inside host cells to survive. They cause malaria, making them one of the most important parasites to understand in global health.
Understanding how Plasmodium is classified helps us see where this important parasite fits in the tree of life. Let’s explore its taxonomic hierarchy step by step.
Within Apicomplexa, Plasmodium belongs to the order Haemosporida. The name tells us exactly what these parasites do – they live inside blood cells of their hosts.
Moving down the hierarchy, we reach the family Plasmodiidae. This family contains the genus Plasmodium and its close relatives.
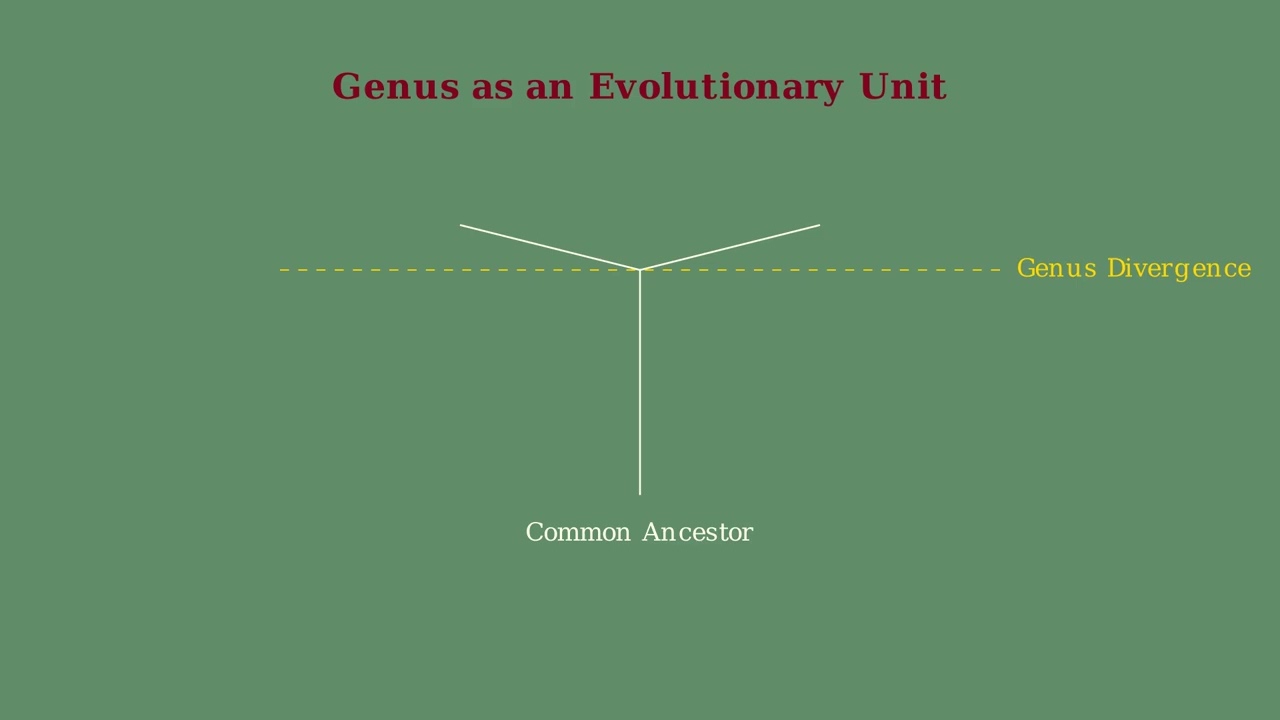
Now here’s where it gets really interesting. The genus Plasmodium contains over 200 species, and scientists have organized these into 14 different subgenera based on their physical characteristics and which types of hosts they infect.
Let’s look at some examples of these subgenera. The species that infect humans are found in two main subgenera: Plasmodium and Laverania. These are the ones that cause malaria in people.
Other subgenera infect different types of hosts. For example, the subgenus Vinckeia contains species that infect other mammals like monkeys and rodents.
Birds have their own set of subgenera including Haemamoeba, Giovannolaia, and others. And reptiles are classified into subgenera like Lacertamoeba and Sauramoeba, showing how diverse this genus really is.
This classification system helps scientists understand the evolutionary relationships between different Plasmodium species and predict which hosts they might infect. It’s a perfect example of how taxonomy organizes the incredible diversity of life on Earth.
Plasmodium vivax is one of the five Plasmodium species that commonly cause malaria in humans. Understanding this particular species is crucial because it has unique characteristics that set it apart from the others.
Plasmodium vivax is geographically dominant in most countries outside of sub-Saharan Africa. While P. falciparum dominates in Africa, P. vivax is the primary malaria parasite in Asia, Latin America, and parts of the Middle East.
The most distinctive feature of Plasmodium vivax is its ability to cause relapses. Unlike other malaria parasites, P. vivax can remain dormant in the liver for months or even years before reactivating.
These dormant forms are called hypnozoites. The term hypnozoite literally means sleeping animal. These sleeping parasites can remain inactive in liver cells for extended periods without causing symptoms.
When conditions are right, these hypnozoites can reactivate weeks, months, or even years later. This reactivation causes a relapse – a new episode of malaria symptoms without being bitten by another infected mosquito.
This relapse capability makes P. vivax particularly challenging to eliminate. Even after successful treatment of the blood-stage infection, patients can experience new episodes of malaria from reactivated hypnozoites. This is why P. vivax requires special treatment approaches.
Plasmodium is a parasitic protozoan – a single-celled organism that lives inside other organisms to survive. Understanding what Plasmodium is helps us grasp how malaria develops and spreads.
These parasites are transmitted to humans through the bite of infected female Anopheles mosquitoes. The mosquito acts as a vector, carrying the parasite from one host to another.
Once inside the human body, Plasmodium undergoes complex life cycle stages. The parasites first multiply in the liver, where they grow and reproduce without causing symptoms.
After multiplying in the liver, the parasites then infect red blood cells. This infection of red blood cells is what causes the characteristic symptoms of malaria, including fever, chills, and fatigue.
In summary, Plasmodium is a parasitic protozoan transmitted by mosquitoes that causes malaria by infecting human red blood cells after first multiplying in the liver. This understanding forms the foundation for learning about malaria prevention and treatment.
Plasmodium parasites have a unique cellular structure that makes them highly effective at invading host cells. Understanding their morphology helps us see how these microscopic organisms cause malaria.
Like all eukaryotic cells, Plasmodium has a cell membrane that defines its boundary and a nucleus containing genetic material. The cell has an elongated, flexible shape that helps it move through host tissues.
The most distinctive feature is the apical complex, located at one end of the cell. This specialized structure contains the molecular machinery needed to invade host cells – it’s like the parasite’s invasion toolkit.
Inside the apical complex are rhoptries – club-shaped organelles that release proteins to help the parasite penetrate host cell membranes. Think of them as molecular drills that break down cellular barriers.
Micronemes are smaller organelles that work alongside rhoptries. They secrete adhesive proteins that help the parasite attach to and glide along host cell surfaces during invasion.
The mitochondrion provides energy for the parasite’s activities. Unlike human mitochondria, the Plasmodium mitochondrion has a simplified structure but remains essential for the parasite’s survival and reproduction.
The apicoplast is a unique organelle found only in certain parasites. It’s essential for synthesizing fatty acids and other molecules the parasite needs. This makes it an important target for antimalarial drugs.
This specialized morphology makes Plasmodium a highly efficient parasite. The apical complex enables invasion, while the mitochondrion and apicoplast support the parasite’s metabolism throughout its complex life cycle.
Plasmodium falciparum stands out as the most dangerous of all Plasmodium species. This deadly parasite is responsible for the vast majority of malaria deaths worldwide.
Plasmodium falciparum is responsible for over ninety percent of malaria deaths globally. It is particularly devastating in Africa, where it causes the most severe form of the disease known as falciparum malaria.
The virulence of Plasmodium falciparum stems from its remarkable ability to infect a large number of red blood cells simultaneously. Unlike other Plasmodium species, P. falciparum can infect red blood cells of all ages.
Plasmodium falciparum causes severe complications that can be life-threatening. The most dangerous is cerebral malaria, where parasites affect the brain, causing swelling, seizures, and potentially coma. Other severe complications include anemia, organ failure, and respiratory problems.
To summarize, Plasmodium falciparum is the most lethal of all malaria parasites. It causes over ninety percent of malaria deaths worldwide, particularly in Africa. Its danger comes from its ability to infect large numbers of red blood cells and cause severe complications like cerebral malaria.
Plasmodium ovale is one of the five main species of Plasmodium parasites that cause malaria in humans. This single-celled parasite has distinct characteristics that set it apart from other malaria-causing species.
Plasmodium ovale is found predominantly in sub-Saharan Africa. This geographic distribution is important for understanding where this particular species of malaria parasite poses the greatest health risk.
Plasmodium ovale often overlaps geographically with Plasmodium vivax. This means that in some regions, both species can be found, making accurate diagnosis and treatment planning more complex.
Like Plasmodium vivax, Plasmodium ovale has a unique ability to form hypnozoites in the liver. These are dormant forms of the parasite that can remain inactive for weeks, months, or even years.
The presence of hypnozoites means that patients infected with Plasmodium ovale can experience relapses. Even after successful treatment of the initial infection, the dormant hypnozoites can reactivate, causing new episodes of malaria symptoms.
While Plasmodium ovale is less common than Plasmodium falciparum, it remains an important cause of malaria. Its ability to form hypnozoites means that proper treatment must address both the active infection and the dormant liver stages to prevent future relapses.
Plasmodium parasites possess several unique characteristics that make them highly effective pathogens. These features enable them to survive, reproduce, and spread between different hosts.
The first major characteristic is their complex life cycle involving both sexual and asexual reproduction in different hosts.
Plasmodium parasites have a remarkable ability to invade and multiply within different types of host cells, particularly liver cells and red blood cells.
These parasites possess specialized organelles that are crucial for host cell invasion and survival. The apical complex contains structures like rhoptries and micronemes that help the parasite penetrate and modify host cells.
In summary, Plasmodium parasites are characterized by their complex dual-host life cycle, their ability to invade multiple cell types, and their specialized cellular machinery for host invasion and survival.
The genome of Plasmodium represents one of the most important breakthroughs in malaria research. Understanding the genetic blueprint of this deadly parasite has revolutionized how we study and combat malaria.
In 1995, scientists achieved a major breakthrough by sequencing the complete genome of Plasmodium falciparum, the deadliest malaria parasite. This was a monumental achievement that opened new doors for malaria research.
The genome sequencing revealed crucial insights into three key areas. First, it helped us understand the complex biology of the parasite, including how it completes its intricate life cycle and produces essential proteins.
Second, it provided critical understanding of drug resistance mechanisms. By identifying specific gene mutations, researchers could finally understand how the parasite develops resistance to antimalarial drugs.
Third, and perhaps most importantly, it identified potential drug targets. The genome revealed essential genes and unique proteins that could be targeted by new antimalarial medications.
Genome research has enabled multiple practical applications in the fight against malaria. The genetic data serves as a foundation for developing new drugs, creating better vaccines, and improving diagnostic tools.
The key takeaway is that genome sequencing has transformed malaria research from guesswork to precision science. It has accelerated drug discovery, improved our understanding of resistance mechanisms, and opened up entirely new therapeutic strategies in the ongoing battle against this deadly disease.
Plasmodium parasites have a unique requirement that makes them particularly complex organisms. Unlike many other parasites, they cannot complete their entire life cycle in just one host.
The first host is a vertebrate, such as humans, monkeys, or other mammals. In this vertebrate host, the parasite undergoes asexual reproduction, multiplying rapidly within the host’s cells.
The second host is specifically a female Anopheles mosquito. This is where sexual reproduction occurs, allowing the parasite to create genetic diversity and produce the infective forms needed to transmit to new vertebrate hosts.
The parasite must cycle between these two hosts to survive. It cannot complete its life cycle in just the vertebrate host alone, nor can it survive only in the mosquito. This two-host requirement is what makes malaria transmission possible.
This two-host system is crucial for the parasite’s survival strategy. The asexual reproduction in vertebrates allows rapid multiplication and disease symptoms, while sexual reproduction in mosquitoes creates genetic diversity and produces the sporozoites needed to infect new hosts.
The genus Plasmodium contains over 200 different species of parasites. However, only a small fraction of these species can infect humans.
Of these many species, only five are commonly responsible for human malaria infections. These five species are the focus of medical research and treatment protocols.
Now let’s examine each of these five species in detail, starting with their names and key characteristics.
Understanding the differences between these species is crucial for medical professionals. Each species requires different treatment approaches and has varying levels of drug resistance.
Accurate species identification through laboratory testing enables healthcare providers to choose the most effective treatment and predict potential complications for each patient.
Plasmodium parasites have a sophisticated cellular structure that makes them highly effective at invading host cells. Let’s examine the key components that make up a Plasmodium cell.
Like all eukaryotic cells, Plasmodium has a cell membrane that surrounds the entire parasite. This membrane contains specialized surface structures that help the parasite interact with its environment and host cells.
The most important feature of Plasmodium is the apical complex, located at one end of the cell. This specialized structure contains organelles that are absolutely essential for invading host cells.
Within the apical complex, we find rhoptries – these club-shaped organelles contain enzymes and proteins that help the parasite break into host cells. They act like molecular drills, creating pathways for invasion.
Micronemes are smaller organelles that work alongside rhoptries. They secrete adhesive proteins that help the parasite attach to and glide along host cell surfaces before invasion.
Now let’s look at the metabolic machinery of the parasite. Plasmodium contains two crucial organelles that originated from ancient endosymbiotic bacteria.
The mitochondrion is the powerhouse of the Plasmodium cell, just like in other eukaryotes. It produces energy through cellular respiration and contains internal structures called cristae that increase its surface area for energy production.
The apicoplast is a unique organelle found only in parasites like Plasmodium. This plastid-like structure is essential for synthesizing fatty acids and other metabolic processes. It’s a remnant of an ancient algae that was engulfed by the parasite’s ancestors.
These specialized organelles work together to make Plasmodium an incredibly efficient parasite. The apical complex enables host invasion, while the mitochondrion and apicoplast maintain the metabolic processes necessary for survival and reproduction within the host.
The Plasmodium life cycle is remarkably complex, requiring two different hosts to complete its reproduction. Understanding this cycle is crucial for comprehending how malaria spreads and persists.
The cycle begins when an infected female Anopheles mosquito bites a human. During this bite, the mosquito injects sporozoites – the infective stage of the parasite – into the human bloodstream.
Once in the human body, sporozoites travel through the bloodstream to the liver. This is called the exo-erythrocytic stage. In liver cells called hepatocytes, sporozoites multiply asexually, producing thousands of merozoites.
After multiplying in the liver, merozoites are released into the bloodstream where they infect red blood cells. This blood stage is called erythrocytic schizogony and is responsible for the characteristic symptoms of malaria.
Some merozoites in red blood cells develop into gametocytes – the sexual forms of the parasite. These gametocytes are crucial for transmission because they can survive in the mosquito’s digestive system.
When another mosquito bites the infected human, it ingests these gametocytes along with the blood meal. Inside the mosquito’s gut, gametocytes develop into male and female gametes and undergo sexual reproduction.
The fertilized zygote develops into an oocyst, which produces thousands of new sporozoites. These sporozoites migrate to the mosquito’s salivary glands, ready to infect the next human host when the mosquito bites again.
This complex life cycle explains why malaria is so persistent and difficult to eliminate. The parasite’s ability to reproduce in both hosts and its multiple developmental stages make it a formidable pathogen that continues to affect millions worldwide.
The genome of Plasmodium represents one of the most important breakthroughs in our fight against malaria. Understanding the genetic blueprint of this deadly parasite has opened new doors for treatment and prevention strategies.
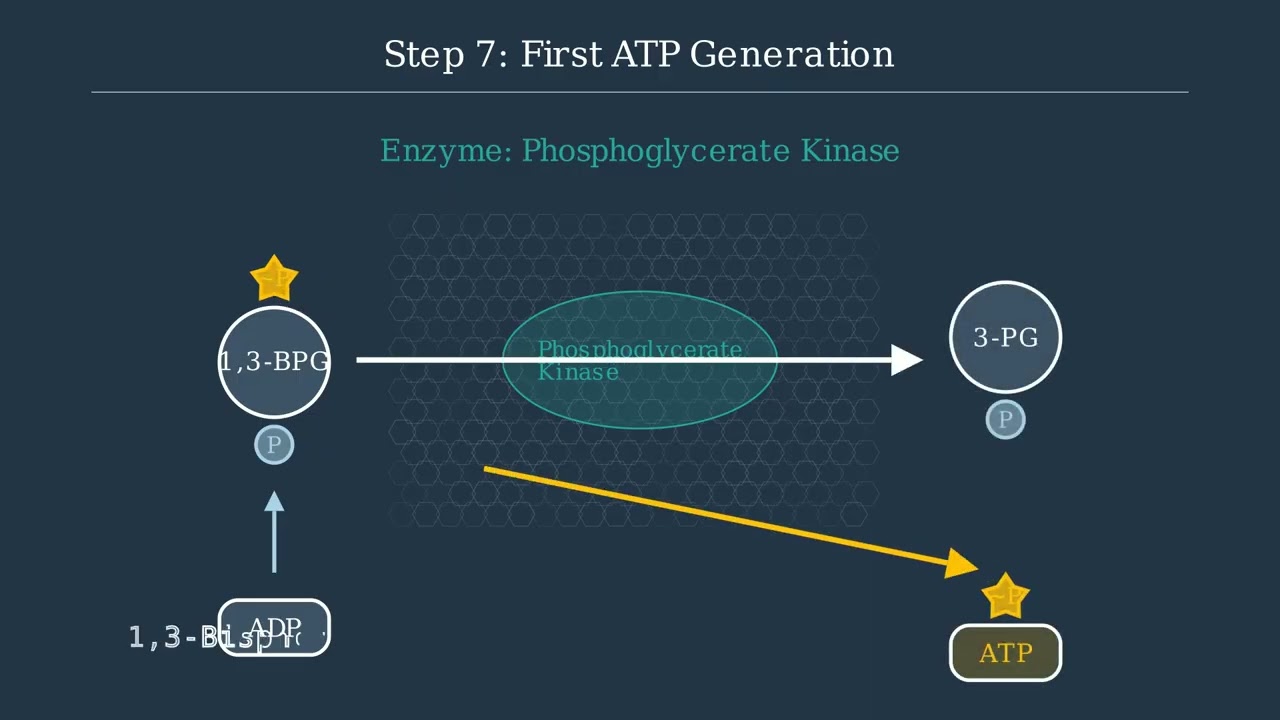
In 1995, scientists achieved a revolutionary milestone by sequencing the complete genome of Plasmodium falciparum. This breakthrough decoded 23 million base pairs and identified over 5,300 genes, providing the first comprehensive genetic map of the deadliest malaria parasite.
Genome sequencing revealed critical drug targets within the parasite. Scientists identified essential enzymes, mapped metabolic pathways, and discovered unique proteins that exist only in Plasmodium. These targets became the foundation for developing new antimalarial drugs.
The genome also revealed how drug resistance develops. When genes mutate, they can alter the shape of proteins that drugs normally target. This knowledge helps scientists understand why some treatments stop working and guides the development of new drugs that can overcome resistance.
Today, genomic research continues to advance our understanding of Plasmodium. Scientists are studying genetic variations between different parasite strains, investigating how specific genes influence disease severity, and searching for novel drug targets that could lead to more effective treatments.
The genome of Plasmodium has transformed our approach to fighting malaria. From the groundbreaking 1995 sequencing to today’s advanced genetic research, this knowledge continues to guide the development of new drugs and treatment strategies, bringing us closer to defeating this deadly disease.
Malaria remains one of the world’s most significant health challenges. Understanding where and how it occurs helps us grasp the true scale of this global problem.
In 2023, malaria affected an estimated 263 million people worldwide, resulting in approximately 597,000 deaths. These numbers represent real human suffering and highlight the urgent need for continued global health efforts.
The burden of malaria is not distributed equally around the world. The WHO African Region carries a disproportionately heavy load, accounting for 94% of all malaria cases and 95% of all deaths globally.
The most heartbreaking aspect of malaria is its impact on children. In the African Region, children under 5 years old represent about 76% of all malaria deaths. These young lives are particularly vulnerable due to their developing immune systems.
These statistics paint a clear picture: malaria is primarily a disease of poverty, affecting the most vulnerable populations in resource-limited settings. Understanding this distribution is crucial for targeting prevention and treatment efforts where they are needed most.
Malaria disease is classified based on the specific Plasmodium species that causes the infection. Each species creates a distinct type of malaria with unique characteristics, severity levels, and treatment requirements.
There are five main types of malaria, each named after the Plasmodium species responsible for the infection.
Falciparum malaria, caused by Plasmodium falciparum, is the most dangerous form. It’s responsible for over ninety percent of malaria deaths worldwide and requires immediate medical attention.
Vivax malaria, from Plasmodium vivax, is characterized by its ability to remain dormant in the liver and cause relapses months or years after the initial infection.
Ovale malaria and malariae malaria are generally milder forms. Ovale malaria is similar to vivax, while malariae malaria tends to cause chronic, long-lasting infections.
Knowlesi malaria is an emerging threat caused by Plasmodium knowlesi, originally a monkey parasite that has adapted to infect humans, particularly in Southeast Asia.
This classification system is crucial for medical professionals because each type requires different treatment approaches and management strategies.
Medical professionals classify malaria into treatment categories. Severe malaria requires immediate hospitalization, moderate forms need standard antimalarial drugs with relapse prevention, and special cases require specialized monitoring protocols.
Understanding malaria classification helps ensure patients receive the most appropriate treatment for their specific infection, improving outcomes and reducing the risk of complications or death.
Malaria disease is a serious global health threat caused by Plasmodium parasites. Understanding how this disease develops and progresses is crucial for prevention and treatment.
Malaria disease begins when an infected female Anopheles mosquito bites a human. During this bite, the mosquito injects Plasmodium parasites called sporozoites into the bloodstream.
Once in the body, the parasites travel to the liver where they invade liver cells. Inside these cells, the parasites multiply rapidly, producing thousands of new parasites called merozoites.
After multiplying in the liver, the parasites are released into the bloodstream where they invade red blood cells. This blood stage infection is what causes the symptoms of malaria disease.
Malaria disease can range from mild to life-threatening. The severity depends on factors like the Plasmodium species, the patient’s immune system, and how quickly treatment is started.
As the disease progresses without treatment, symptoms become more severe, affecting multiple body systems and potentially leading to complications.
Severe malaria is a medical emergency that can cause organ failure, brain damage, and death if not treated immediately.
Early diagnosis and treatment are absolutely critical in malaria disease. The window for effective treatment is narrow, and delays can lead to severe complications or death.
The first few days after symptom onset represent the optimal treatment window. During this time, antimalarial medications are most effective and can prevent the disease from progressing to severe stages.
Remember, malaria disease is both preventable and treatable when diagnosed early. Prompt medical attention at the first sign of symptoms can save lives and prevent serious complications.
Malaria symptoms don’t appear immediately after a mosquito bite. There’s typically a delay of 10 to 15 days before the first symptoms begin to show.
The early symptoms of malaria are often mistaken for common flu-like illness. Let’s examine these initial warning signs that patients typically experience.
The three most common early symptoms are fever, headache, and chills. Fever is usually the first sign, often accompanied by sweating. Patients experience persistent headaches and chills that make them shiver even when they have a high temperature.
If malaria is left untreated, the symptoms can progress to become much more serious and life-threatening. These severe symptoms require immediate medical attention.
Severe malaria symptoms include extreme fatigue that leaves patients bedridden, confusion and altered mental state, seizures, and difficulty breathing. These symptoms indicate that the infection has progressed to a dangerous stage.
It’s crucial to seek immediate medical attention if you experience any of these symptoms, especially if you’ve recently traveled to an area where malaria is common.
Remember these key points: seek medical help if you’ve traveled to a malaria-endemic area and develop any symptoms, don’t ignore fever and headaches, get immediate help for severe symptoms, and remember that early treatment can save lives.
Malaria symptoms can be easily mistaken for common illnesses, but the key difference is the travel history and the timing. When in doubt, always consult a healthcare professional for proper diagnosis and treatment.
Malaria infection progresses through five distinct phases, each playing a crucial role in the parasite’s life cycle and disease development. Understanding these phases helps us comprehend how the infection spreads and persists.
Phase one is pre-erythrocytic schizogony, which occurs in the liver. When an infected mosquito bites, it injects sporozoites into the bloodstream. These sporozoites travel to the liver and invade hepatocytes, where they multiply rapidly.
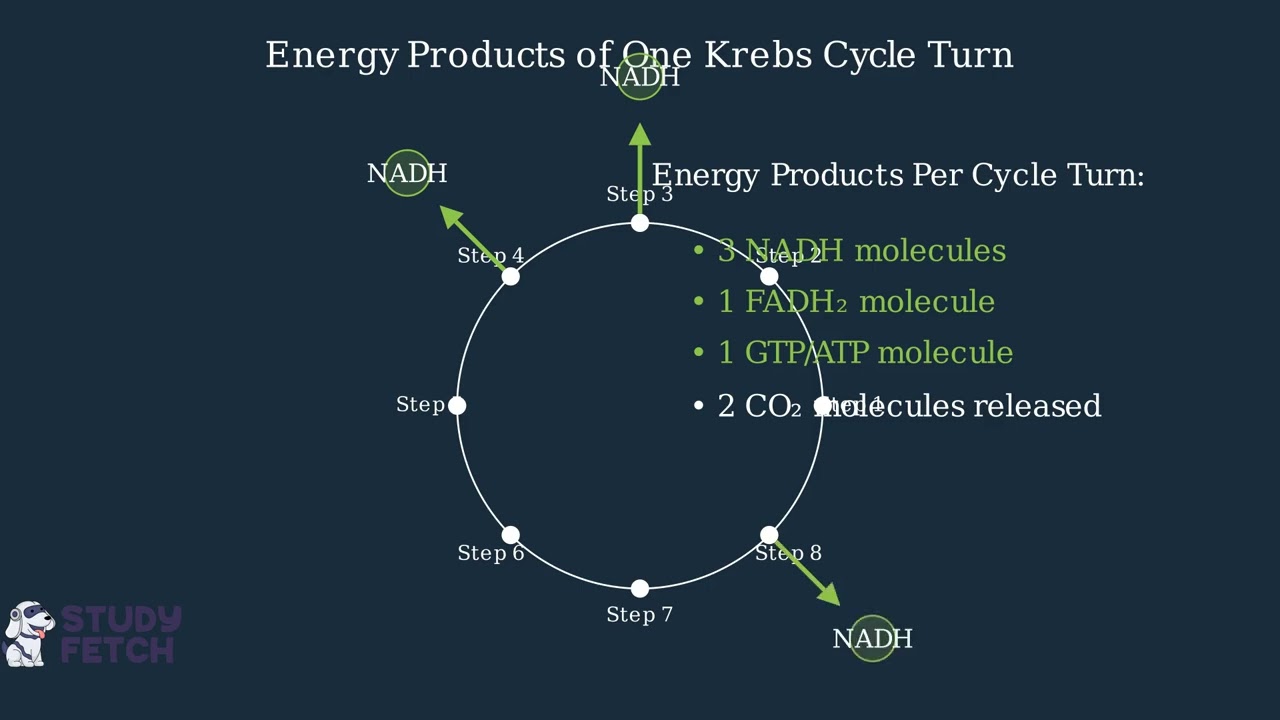
Phase two is erythrocytic schizogony, the blood stage. Merozoites released from the liver invade red blood cells, where they multiply and cause the characteristic symptoms of malaria. This cycle repeats every 48 to 72 hours.
Phase three is gametogony, where some parasites develop into male and female gametocytes instead of continuing asexual reproduction. These sexual forms are essential for transmission back to mosquitoes.
Phase four is exoerythrocytic schizogony, unique to Plasmodium vivax and ovale. Some sporozoites remain dormant in the liver as hypnozoites, which can reactivate months or years later, causing relapsing malaria.
Phase five is sporogony, occurring in the mosquito. When a mosquito ingests gametocytes, they develop into gametes, fertilize, and eventually produce sporozoites in the salivary glands, ready to infect a new human host.
These five phases create a complex cycle that allows malaria parasites to survive, multiply, and spread between human and mosquito hosts. Understanding each phase is crucial for developing effective treatments and prevention strategies.
Diagnosing malaria accurately is crucial for saving lives. When someone shows symptoms of malaria, doctors need to quickly confirm whether Plasmodium parasites are present in their blood.
There are two primary methods used to diagnose malaria: microscopy and rapid diagnostic tests. Each method has its own advantages and is used in different healthcare settings.
Microscopy is the gold standard for malaria diagnosis. A technician takes a blood sample from the patient and examines it under a high-powered microscope to look for Plasmodium parasites inside red blood cells.
Under the microscope, trained technicians can identify the characteristic ring-shaped parasites within infected red blood cells. This method can also determine the species of Plasmodium and estimate the level of infection.
Rapid diagnostic tests provide a faster alternative to microscopy. A small blood sample is placed on a test strip that contains antibodies designed to detect specific Plasmodium antigens.
The test shows colored lines to indicate results. A control line confirms the test is working properly, while a test line appears if Plasmodium antigens are detected, indicating a positive result for malaria.
Accurate malaria diagnosis is essential for effective treatment and preventing complications. Early detection allows doctors to start appropriate antimalarial therapy quickly, which can be life-saving.
Both diagnostic methods have their strengths. Microscopy provides more detailed information but requires trained technicians, while rapid tests offer quick results and can be used in remote healthcare settings where microscopy is not available.
When someone is diagnosed with malaria, immediate treatment with antimalarial drugs is essential. The choice of medication is not one-size-fits-all and depends on several critical factors.
Healthcare providers must consider four key factors when selecting antimalarial treatment. First, the specific Plasmodium species causing the infection. Second, known drug resistance patterns in the region. Third, patient characteristics like age, weight, and pregnancy status. And fourth, the severity of the disease.
There are three main categories of antimalarial drugs. Artemisinin-based combination therapies, or ACTs, are the first-line treatment for most malaria cases. They are highly effective and combining two drugs helps prevent resistance development.
Chloroquine was once the standard treatment but is now limited to areas where parasites remain sensitive to it. Drug resistance has made it ineffective in many regions, particularly for Plasmodium falciparum.
Primaquine serves a special purpose – it eliminates dormant liver stages called hypnozoites found in P. vivax and P. ovale infections. This prevents relapses months or years later. However, patients must be tested for G6PD deficiency before receiving primaquine.
Successful malaria treatment follows four key principles. First, early treatment is critical – delays can be life-threatening. Second, treatment must be individualized based on the specific case. Third, patients must complete the full course of medication to prevent drug resistance. Finally, follow-up care ensures complete recovery and monitors for any complications.
Preventing malaria requires a multi-layered approach that protects individuals and communities from mosquito-borne transmission. We’ll explore four key prevention strategies that work together to reduce malaria risk.
The first line of defense is personal protection against mosquito bites. This includes using insect repellents containing DEET or picaridin, wearing long-sleeved clothing in light colors, and sleeping under insecticide-treated bed nets.
Travelers to malaria-endemic areas should take preventive medications called chemoprophylaxis. These antimalarial drugs must be started before travel, continued during the trip, and taken for several weeks after returning home.
Community-level vector control targets mosquito populations directly. Indoor residual spraying applies long-lasting insecticides to walls and surfaces. Mass distribution of insecticide-treated nets protects entire communities. Environmental management eliminates mosquito breeding sites like standing water.
The World Health Organization recommends malaria vaccination for children living in areas with high malaria transmission. The RTS,S vaccine provides partial protection and must be combined with other prevention measures for maximum effectiveness.
Remember, no single prevention method is one hundred percent effective. The most successful malaria prevention combines personal protection, community vector control, and medical interventions. This integrated approach has dramatically reduced malaria cases worldwide.
Now let’s examine three important examples of Plasmodium species that demonstrate the diversity and global impact of these parasites.
First, Plasmodium falciparum is the most dangerous malaria parasite. This species is responsible for over ninety percent of malaria deaths worldwide and is most prevalent across sub-Saharan Africa.
Second, Plasmodium vivax is the dominant malaria parasite in most countries outside sub-Saharan Africa. This species has a unique ability to remain dormant in the liver as hypnozoites, which can cause malaria relapses months or even years after the initial infection.
Third, Plasmodium knowlesi represents an emerging threat. This zoonotic parasite primarily infects macaque monkeys in Southeast Asia but can cause severe malaria in humans. It demonstrates how malaria parasites can jump between species.
These three examples illustrate the remarkable diversity of Plasmodium parasites. Each species has evolved different strategies for survival and transmission, from falciparum’s deadly efficiency to vivax’s dormancy mechanism and knowlesi’s ability to cross species barriers.
Study Materials
Life Cycle of Plasmodium vivax in Man and in Mosquito
Plasmodium vivax - Morphology, Life Cycle, Epidemiology, Pathogenicity, Diagnosis, Prophylaxis and Treatment
Comments 1
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
Start Asking Questions Cancel reply
Helpful: 0%
Related Videos

good.