Sourav Pan
Transcript
What is Glycogenolysis?
Glycogenolysis is the metabolic process of breaking down glycogen, which is the stored form of glucose, into individual glucose molecules.
This process involves the systematic breakdown of glycogen, a large branched polymer of glucose, into its constituent glucose units.
Glycogenolysis is essential for several important physiological functions.
It provides energy during fasting periods when glucose is not being consumed through diet.
It helps maintain stable blood glucose levels, which is crucial for brain function and overall homeostasis.
And it responds to increased energy demands, such as during exercise or stress.
Glycogenolysis is a fundamental process in human metabolism that helps ensure a steady supply of glucose, the body’s primary energy source.
Glycogen phosphorylase is the principal enzyme responsible for initiating glycogen breakdown during glycogenolysis.
Glycogen phosphorylase exists as a dimer, consisting of two identical protein subunits that work together for its enzymatic function.
The enzyme requires pyridoxal phosphate, a derivative of vitamin B6, as a cofactor for its catalytic activity.
Glycogen phosphorylase specifically cleaves alpha-1,4 glycosidic bonds in the glycogen chain.
When the enzyme acts on glycogen, it breaks the alpha-1,4 bonds and releases glucose-1-phosphate units.
Each cleavage reaction releases a single glucose-1-phosphate unit, which can then enter metabolic pathways.
To summarize, glycogen phosphorylase is the principal enzyme in glycogenolysis, with a dimeric structure requiring vitamin B6 as a cofactor, and releasing glucose-1-phosphate units through its action.
Glycogen phosphorylase catalyzes the breakdown of glycogen into glucose-1-phosphate through a process called phosphorolysis.
Unlike hydrolysis which uses water, phosphorolysis uses inorganic phosphate to break glycosidic bonds.
Glycogen phosphorylase works specifically from the non-reducing ends of glycogen chains.
The enzyme attaches to the non-reducing end of a glycogen chain, and with the help of inorganic phosphate, it cleaves off one glucose unit at a time.
This process repeats sequentially, removing one glucose unit after another, generating glucose-1-phosphate with each cleavage.
Importantly, glycogen phosphorylase can only continue cleaving until it reaches about four glucose units from a branch point. At this point, another enzyme, the debranching enzyme, is required to continue the process.
To summarize, glycogen phosphorylase works by phosphorolysis to sequentially remove glucose units from the non-reducing ends of glycogen, producing glucose-1-phosphate, until it reaches about four glucose units from a branch point.
Phosphoglucomutase is a crucial enzyme in the glycogenolysis pathway.
This enzyme catalyzes an important isomerization reaction, converting glucose-1-phosphate to glucose-6-phosphate.
The enzyme catalyzes the conversion between two isomers of glucose phosphate.
This reaction is an isomerization, where the phosphate group moves from carbon 1 to carbon 6. The mechanism involves a temporary addition of another phosphate group, forming glucose-1,6-bisphosphate as an intermediate.
This conversion is crucial because glucose-6-phosphate is a versatile metabolic intermediate that can enter various pathways.
In the liver, glucose-6-phosphate can be converted to free glucose by the enzyme glucose-6-phosphatase, allowing glucose to be released into the bloodstream to maintain blood glucose levels.
In muscle tissue, which lacks glucose-6-phosphatase, glucose-6-phosphate enters glycolysis directly to produce energy in the form of ATP.
In summary, phosphoglucomutase provides metabolic flexibility by converting glucose-1-phosphate from glycogen breakdown to glucose-6-phosphate, which can then feed into multiple metabolic pathways depending on the tissue and the body’s needs.
Glucagon is a hormone secreted by pancreatic alpha cells when blood glucose levels are low.
When blood glucose drops, alpha cells release glucagon into the bloodstream.
Glucagon primarily targets the liver, where it binds to specific receptors on the cell membrane.
When glucagon binds to its receptor, it triggers a signaling cascade inside the liver cell.
The activated receptor stimulates an enzyme called adenylyl cyclase.
Adenylyl cyclase converts ATP into cyclic AMP, or cAMP, which acts as a second messenger.
Increased cAMP activates Protein Kinase A, an enzyme that adds phosphate groups to other proteins.
Protein Kinase A then activates Phosphorylase Kinase through phosphorylation.
Finally, Phosphorylase Kinase activates Glycogen Phosphorylase, the key enzyme that catalyzes glycogenolysis.
Activated Glycogen Phosphorylase breaks down glycogen into glucose-1-phosphate molecules, which can then be converted to glucose-6-phosphate and either used by the cell or released into the bloodstream.
This entire cascade ensures that when blood glucose levels are low, the liver breaks down its glycogen stores to release glucose and restore normal blood glucose levels.
Epinephrine, also known as adrenaline, is a hormone released during the fight-or-flight response.
When released, epinephrine stimulates glycogenolysis in both liver and muscle tissues to rapidly provide glucose for energy.
In the liver, epinephrine works through a cAMP-dependent pathway, similar to glucagon. It binds to beta-adrenergic receptors, activating G proteins and adenylyl cyclase.
This increases cAMP levels, which activates Protein Kinase A. PKA then phosphorylates and activates glycogen phosphorylase, initiating glycogenolysis.
In muscle tissue, epinephrine operates through two mechanisms. First, the cAMP pathway via beta-adrenergic receptors, similar to the liver.
But muscle tissue also responds through alpha-adrenergic receptors, activating a calcium-dependent pathway. This involves phospholipase C and IP3 production.
The IP3 triggers calcium release from the sarcoplasmic reticulum. This calcium then activates phosphorylase kinase, which in turn activates glycogen phosphorylase, leading to glycogenolysis.
Both pathways lead to increased glycogenolysis, releasing glucose-1-phosphate that can be converted to glucose-6-phosphate. In the liver, this can become free glucose to raise blood glucose levels.
To summarize, epinephrine stimulates glycogenolysis in both liver and muscle through cAMP-dependent pathways, with muscle having an additional calcium-dependent mechanism, allowing for a rapid response during stress or physical activity.
Glycogen phosphorylase activity is finely controlled through allosteric regulation.
Glycogen phosphorylase has an active site where catalysis occurs, and separate allosteric sites where regulatory molecules can bind.
When cellular energy is low, AMP levels increase. AMP is an allosteric activator of glycogen phosphorylase.
When AMP binds to the allosteric site, it causes a conformational change that activates the enzyme.
The activated enzyme can now more efficiently break down glycogen, releasing glucose-1-phosphate molecules.
In contrast, when energy is abundant, both glucose and ATP act as allosteric inhibitors of glycogen phosphorylase.
When glucose levels are high, it binds to the allosteric site and inhibits the enzyme.
Similarly, high ATP levels indicate that the cell has sufficient energy. ATP binds to another allosteric site, further stabilizing the inactive conformation.
With both glucose and ATP bound, the enzyme adopts a fully inhibited conformation, significantly reducing glycogenolysis.
These regulatory mechanisms involve shifting the enzyme between two conformational states: the tense T state with lower activity, and the relaxed R state with higher activity.
In summary, AMP shifts the enzyme toward the active R state, while glucose and ATP promote the inactive T state. This allows glycogen breakdown to be precisely regulated based on the cell’s energy status.
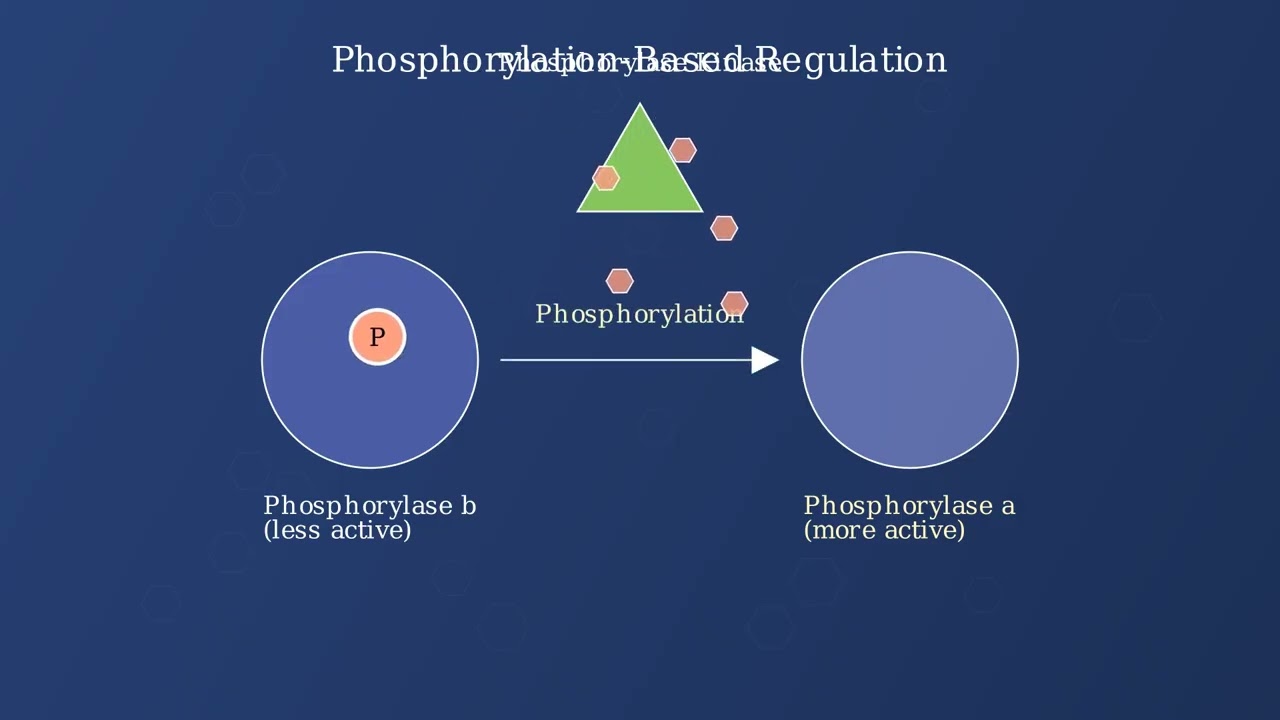
We’ll now explore how glycogen phosphorylase is regulated through phosphorylation.
Glycogen phosphorylase exists in two main forms: the less active phosphorylase b and the more active phosphorylase a.
The conversion from phosphorylase b to phosphorylase a is catalyzed by an enzyme called phosphorylase kinase.
Phosphorylase kinase adds a phosphate group to phosphorylase b, converting it to phosphorylase a.
This phosphorylation dramatically increases the enzyme’s activity. Phosphorylase a is much more efficient at breaking down glycogen than phosphorylase b.
This phosphorylation-based regulation is initiated by hormonal signals like glucagon and epinephrine. When these hormones bind to cell receptors, they trigger a signaling cascade.
This cascade activates several enzymes in sequence, ultimately leading to the activation of phosphorylase kinase.
This phosphorylation-based regulation system provides rapid and sensitive control of glycogen breakdown in response to hormonal signals.
The system allows for rapid responses to metabolic demands, amplification of hormonal signals, and precise control of glycogen breakdown when energy is needed.
Calcium ions serve as critical second messengers in the regulation of glycogenolysis, particularly in muscle tissue during exercise.
When muscles contract, calcium is released from the sarcoplasmic reticulum into the sarcoplasm.
This sudden increase in cytosolic calcium concentration triggers a coordinated response that links muscle contraction with energy production.
Calcium directly binds to phosphorylase kinase, which has a specific calcium-binding subunit, triggering its activation.
The activated phosphorylase kinase then phosphorylates and activates glycogen phosphorylase, the key enzyme in glycogenolysis.
Activated glycogen phosphorylase begins breaking down glycogen into glucose-1-phosphate molecules, providing energy for the contracting muscle.
This calcium-mediated mechanism ensures that glycogen breakdown is tightly coordinated with muscle contraction, providing energy precisely when and where it is needed during exercise.
This calcium-dependent regulation is rapid, operating within milliseconds, and functions independently of hormonal signals. It provides localized energy at the site of muscle contraction without causing systemic changes in blood glucose levels.
Liver glycogenolysis is a critical process that maintains blood glucose levels between meals.
When blood glucose begins to fall after a meal, the liver breaks down glycogen stores to release glucose.
This released glucose enters the bloodstream, maintaining blood glucose levels and preventing hypoglycemia.
Glycogenolysis is one of the body’s first responses to declining blood glucose, occurring within a few hours after a meal and before gluconeogenesis becomes active.
Without glycogenolysis, blood glucose levels would rapidly fall below the normal range, leading to hypoglycemia during fasting periods.
Glycogenolysis is essential for preventing hypoglycemia during fasting periods. It provides a rapid source of glucose before other metabolic pathways like gluconeogenesis become fully active.
As one of the body’s primary metabolic defenses, liver glycogenolysis ensures a constant supply of glucose to the brain and other vital organs between meals.
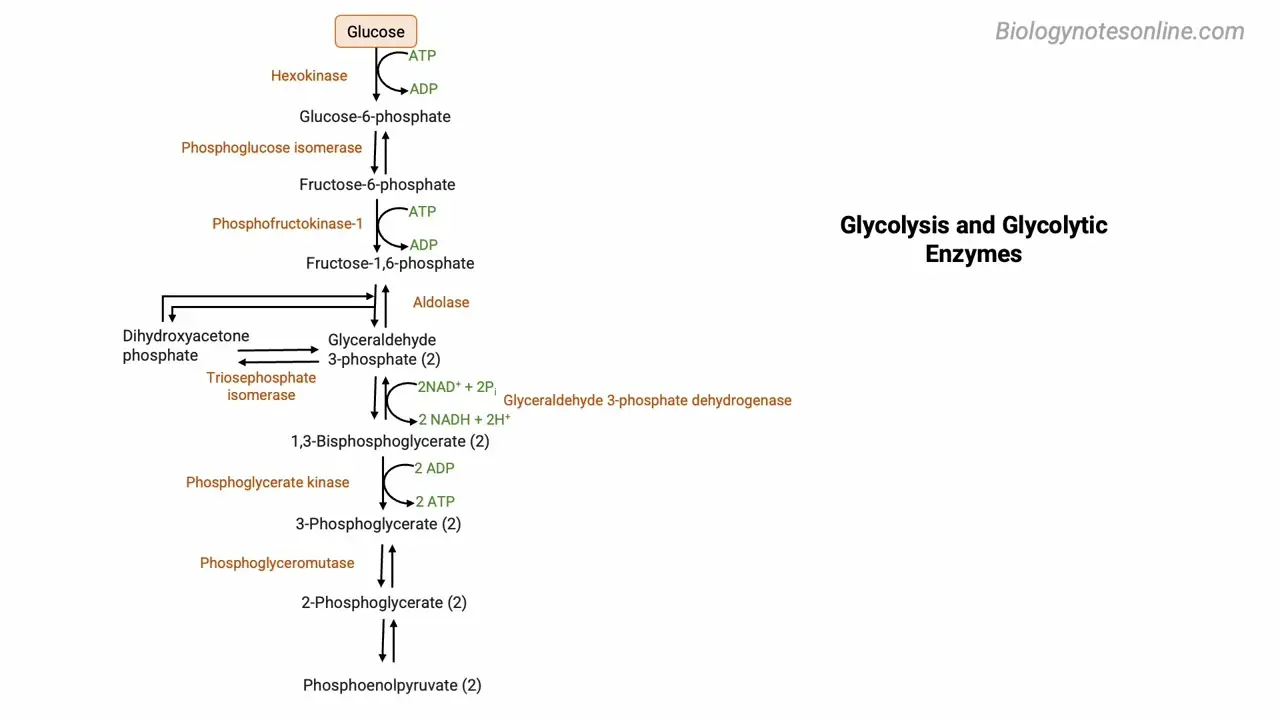
During exercise, muscle cells need a rapid source of energy.
Muscle glycogenolysis is crucial for providing immediate energy, especially during high-intensity activities.
During exercise, glycogen in muscles is broken down through glycogenolysis, releasing glucose-6-phosphate.
Glucose-6-phosphate enters glycolysis, a metabolic pathway that generates ATP rapidly.
This process is especially important because it can generate energy without requiring oxygen, making it crucial for intense bursts of activity like sprinting or weightlifting.
This makes muscle glycogenolysis critical for short-duration, high-intensity exercise, where ATP demands are high and oxygen utilization cannot keep pace.
Glycogenolysis has important functions beyond simply generating energy.
The glucose-6-phosphate released from glycogen can support various other cellular activities.
One crucial pathway is the pentose phosphate pathway, which uses glucose-6-phosphate to generate NADPH.
NADPH is essential for biosynthetic reactions like lipid synthesis and provides electrons for antioxidant defense systems.
Glucose from glycogenolysis also provides substrates for protein glycosylation, a critical post-translational modification.
Glycosylation is essential for cell-cell recognition, proper protein folding, and protein stability.
In the liver, glycogenolysis plays a particularly important role in supplying glucose for various tissues and cellular processes.
For example, red blood cells rely on the pentose phosphate pathway for antioxidant defense, the brain needs glucose for proper functioning, and immune cells require glycosylation for cell recognition and signaling.
Diagnosing glycogenolysis disorders requires a comprehensive approach using multiple testing methods.
Enzyme assays from tissue biopsies are a cornerstone of diagnosis. Samples are usually taken from liver or muscle tissue to directly measure the activity of enzymes involved in glycogen breakdown.
Genetic testing identifies mutations in genes responsible for glycogenolysis. This allows precise diagnosis of specific disorders like Von Gierke disease, Pompe disease, and others. It also helps identify carriers and enables genetic counseling.
Exercise tolerance tests examine how the body responds to physical activity. In glycogenolysis disorders, patients often show abnormal patterns of lactate production, glucose utilization, and fatigue. These tests are particularly valuable for diagnosing muscle-related glycogen storage diseases.
Imaging studies provide non-invasive visualization of affected organs. Ultrasound, MRI, CT scans, and FibroScan can detect hepatomegaly or enlarged liver, a common feature in many glycogenolysis disorders. These scans can also identify muscle abnormalities and help monitor disease progression.
By combining different diagnostic approaches, clinicians can differentiate between various glycogenolysis disorders. Each disorder has a unique pattern of enzyme deficiencies, genetic mutations, and clinical features. This comprehensive approach ensures accurate diagnosis, which is essential for proper management and treatment.
Glycogenolysis is the enzymatic process of breaking down glycogen into glucose-1-phosphate, which is converted to glucose for energy use.
Glycogenolysis occurs primarily in the liver and skeletal muscle, but through slightly different pathways. Both tissues use glycogen phosphorylase as the rate-limiting enzyme, followed by debranching enzyme and phosphoglucomutase.
The critical difference is that liver cells possess glucose-6-phosphatase, allowing them to release free glucose into the bloodstream to maintain blood glucose levels. Muscle cells lack this enzyme and use glucose primarily for their own energy needs.
Glycogenolysis is tightly regulated through multiple mechanisms. Hormonal control includes glucagon and epinephrine, which promote the process, while insulin inhibits it.
Allosteric regulators include AMP which activates and ATP and glucose-6-phosphate which inhibit the process. Enzyme phosphorylation through protein kinase A and phosphorylase kinase plays a crucial role.
In muscle, calcium release during contraction directly activates phosphorylase kinase, rapidly mobilizing glycogen during exercise.
Glycogenolysis serves three primary physiological functions. First, it maintains blood glucose levels, especially during fasting periods, which is essential for brain function.
Second, it provides rapid energy during exercise, particularly during high-intensity activities when oxygen delivery isn’t sufficient for aerobic metabolism.
Third, it supports the body’s immediate energy needs during stress responses and helps cells adapt to changing metabolic demands.
The clinical significance of glycogenolysis is most evident in glycogen storage diseases, where genetic enzyme deficiencies disrupt the normal breakdown of glycogen.
Type I GSD, or von Gierke disease, involves glucose-6-phosphatase deficiency, preventing liver glucose release. This causes severe hypoglycemia, hepatomegaly, and growth retardation.
Type V GSD, or McArdle disease, involves muscle glycogen phosphorylase deficiency, causing exercise intolerance and muscle cramps because muscle cells cannot use their glycogen stores during activity.
Understanding glycogenolysis has significant implications for medical practice. It’s crucial for diabetes management, where disrupted glycogen metabolism contributes to glucose dysregulation.
It’s essential knowledge for exercise physiology, sports medicine, and critical care, where stress can induce hyperglycemia through accelerated glycogenolysis.
It informs genetic counseling for glycogen storage diseases and enables drug development targeting specific steps in the pathway.
In conclusion, glycogenolysis represents a fundamental metabolic process that maintains energy homeostasis and ensures glucose availability when needed, highlighting the elegant balance of our metabolic systems.
Study Materials
Glycogenolysis - Enzymes, Steps, Regulation, Functions
Glycogenesis vs Glycogenolysis
Helpful: 0%
Related Videos
- Text Highlighting: Select any text in the post content to highlight it
- Text Annotation: Select text and add comments with annotations
- Comment Management: Edit or delete your own comments
- Highlight Management: Remove your own highlights
How to use: Simply select any text in the post content above, and you'll see annotation options. Login here or create an account to get started.